- Department of Neurosurgery, Université Félix Houphouet Boigny, Chu de Yopougon, Cote D’Ivoire.
Correspondence Address:
Djiby Jean Marcel Okamon, Department of Neurosurgery, Université Félix Houphouet Boigny, Chu de Yopougon, Cote D’Ivoire.
DOI:10.25259/SNI_672_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Djiby Jean Marcel Okamon, Mahamadou Coulibaly, Dominique N’dri. Cervical spinal meningioma mimicking an arachnoid cyst: A pediatric case report. 22-Dec-2023;14:441
How to cite this URL: Djiby Jean Marcel Okamon, Mahamadou Coulibaly, Dominique N’dri. Cervical spinal meningioma mimicking an arachnoid cyst: A pediatric case report. 22-Dec-2023;14:441. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12679
Abstract
Background: Meningiomas are rare tumors in children. Although magnetic resonance imaging (MRI) diagnosis is usually easy, its cystic form can wrongly suggest other diagnoses, such as an epidermoid or arachnoid cyst. We describe an unusual case of cervical cystic meningioma in a child.
Case Description: A 5-year-old patient was consulted for progressive weakness of all four limbs, making walking impossible. Neurological examination revealed cervical stiffness without meningeal signs and tetrapyramidal syndrome with incomplete tetraplegia. A cervical spine MRI showed a circumscribed intradural extramedullary lesion at the level of C2–C3, which led to a suspicion of a compressive arachnoid cyst. A gross total resection was performed through a posterior approach. During surgery, it was an extramedullary intradural cystic formation containing a clear liquid and a shell adherent to the Dura mater. Postoperative MRI shows satisfactory spinal cord decompression without evidence of residual tumor. The postoperative course was uneventful, with the resumption of independent walking on the 21st day. Histopathologic examination and immunohistochemistry revealed a grade I meningothelial meningioma according to the 2021 World Health Organization classification of tumors of the central nervous system.
Conclusion: Cystic meningiomas can sometimes suggest another diagnosis on imaging, especially since they are rare in children.
Keywords: Arachnoid cyst, Case report, Pediatric, Spinal meningioma
INTRODUCTION
Meningiomas are benign extraparenchymal tumors developed from arachnoid cells. Although common in adults, meningiomas are rare in children and account for <2% of all meningiomas.[
CASE DESCRIPTION
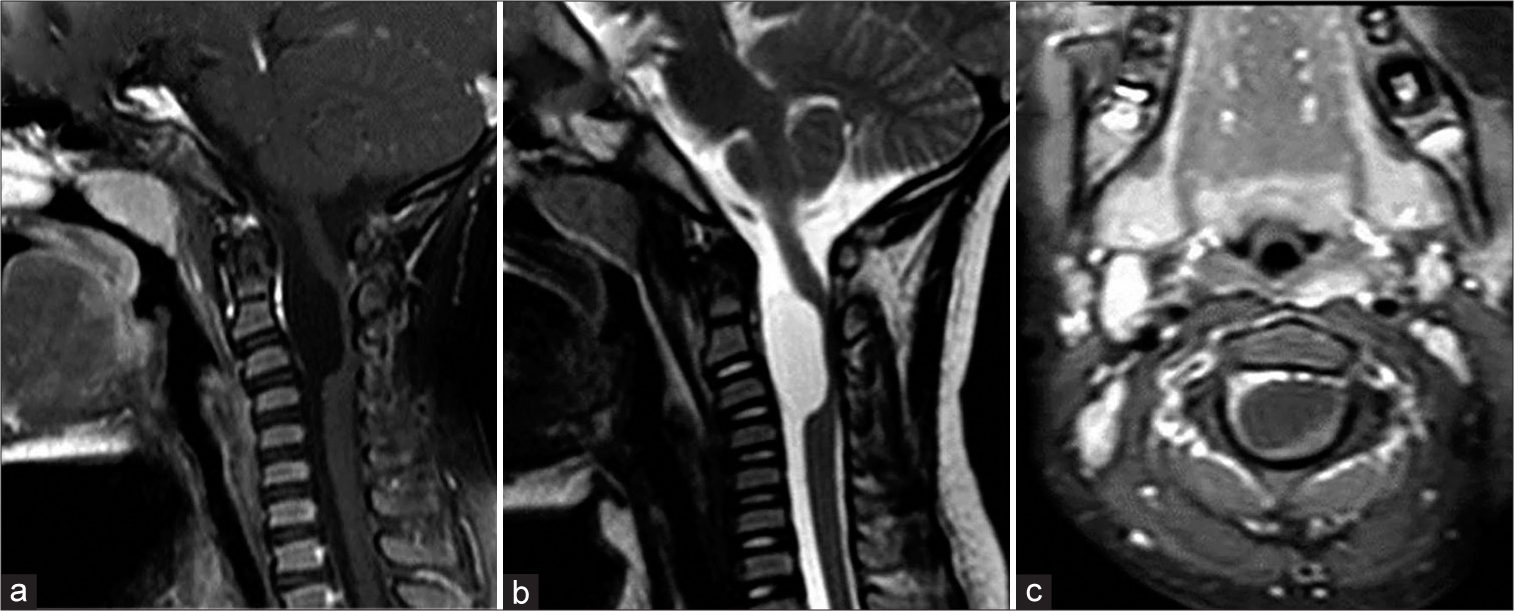
A 5-year-old patient who was consulted for progressive weakness of all four limbs, making walking impossible. He also complained of neck pain. The patient has no medical history. Neurological examination revealed a normal state of consciousness, cervical stiffness without meningeal signs, and tetrapyramidal syndrome with incomplete tetraplegia. Cervical spine MRI showed a circumscribed intradural extramedullary lesion at the level of C2–C3, which was hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging, without contrast enhancement [
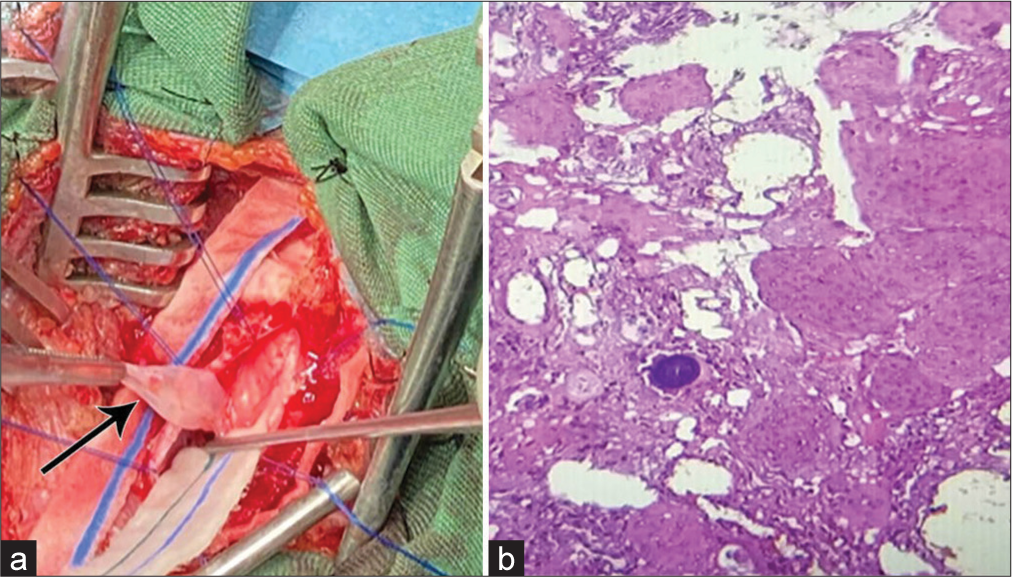
Figure 2:
(a) Preoperative image showing the tumor capsule (black arrow) removed from the surgical bed; (b) Microphotograph showing histopathological findings, tumor proliferation made of cords, lobule. Arachnoid-like tumor cells are rounded, with an abundant basophilic cytoplasm containing a more or less regular nucleus. There are some cytonuclear atypia without mitosis.
DISCUSSION
Spinal meningiomas are rarely found in the pediatric population.[
CONCLUSION
Cystic meningiomas can sometimes suggest another diagnosis on imaging, especially since they are rare in children. Surgical findings, especially histopathology, represent a major asset for the rest of the diagnostic and therapeutic management.
Ethical Approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Dudley RW, Torok MR, Randall S, Béland B, Handler MH, Mulcahy-Levy JM. Pediatric versus adult meningioma: Comparison of epidemiology, treatments, and outcomes using the Surveillance, Epidemiology, and End Results database. J Neurooncol. 2018. 137: 621-9
2. Greene S, Nair N, Ojemann JG, Ellenbogen RG, Avellino AM. Meningiomas in children. Pediatr Neurosurg. 2008. 44: 9-13
3. Grossbach AJ, Mahaney KB, Menezes AH. Pediatric meningiomas: 65-year experience at a single institution. J Neurosurg Pediatr. 2017. 20: 42-50
4. Hao Z, Hu S, Yu NZ. Rare intraspinal clear cell meningioma in children: A case report and literature review. J Int Med Res. 2020. 48: 300060520952266
5. Kobayashi K, Ando K, Matsumoto T, Sato K, Kato F, Kanemura T. Clinical features and prognostic factors in spinal meningioma surgery from a multicenter study. Sci Rep. 2021. 11: 11630
6. Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T. Long-term surgical outcomes of spinal meningiomas. Spine (Phila Pa 1976). 2012. 37: E617-23
7. Piątek P, Kwiatkowski S, Milczarek O. Spinal meningiomas in pediatric patients-A case series and literature review. Surg Neurol Int. 2022. 13: 445
8. Sheikh BY, Siqueira E, Dayel F. Meningioma in children: A report of nine cases and a review of the literature. Surg Neurol. 1996. 45: 328-35
9. Vaneckova M, Seidl Z, Kemlink D, Zamecnik J, Burgetova A. Cervical meningioma in childhood. A case report. Neuroradiol J. 2008. 21: 383-7
10. Wang XQ, Zeng XW, Zhang BY, Dou YF, Wu JS, Jiang CC. Spinal meningioma in childhood: Clinical features and treatment. Childs Nerv Syst. 2012. 28: 129-36
11. Wu L, Yang C, Liu T, Fang J, Yang J, Xu Y. Clinical features and long-term outcomes of pediatric spinal meningiomas. J Neurooncol. 2017. 133: 347-55