- Department of Surgery, Federal Teaching Hospital, Ido Ekiti/Afe Babalola University, Ado Ekiti, Nigeria. and
- Department of Radiology, Federal Teaching Hospital, Ido Ekiti/Afe Babalola University, Ado Ekiti, Nigeria.
Correspondence Address:
Abiodun Idowu Okunlola, Department of Surgery, Federal Teaching Hospital, Ido Ekiti/ Afe Babalola University, Ado Ekiti, Nigeria.
DOI:10.25259/SNI_449_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abiodun Idowu Okunlola1, Paul Olukayode Abiola1, Olakunle Fatai Babalola1, Chijioke Cosmas Achebe2. Cervical spine computed tomography motion artifact mimicking spine injury in a patient with severe head injury. 03-Aug-2021;12:390
How to cite this URL: Abiodun Idowu Okunlola1, Paul Olukayode Abiola1, Olakunle Fatai Babalola1, Chijioke Cosmas Achebe2. Cervical spine computed tomography motion artifact mimicking spine injury in a patient with severe head injury. 03-Aug-2021;12:390. Available from: https://surgicalneurologyint.com/surgicalint-articles/11011/
Abstract
Background: Craniocervical CT scan is an essential part of the routine evaluation of patient with moderate and severe head injury to rule out associated cervical spine injury. Computed tomography motion artifacts can affect clinical decision making. The aim of this report is to emphasize that motion artifact still exists despite advance in technology and this can pose clinical challenge.
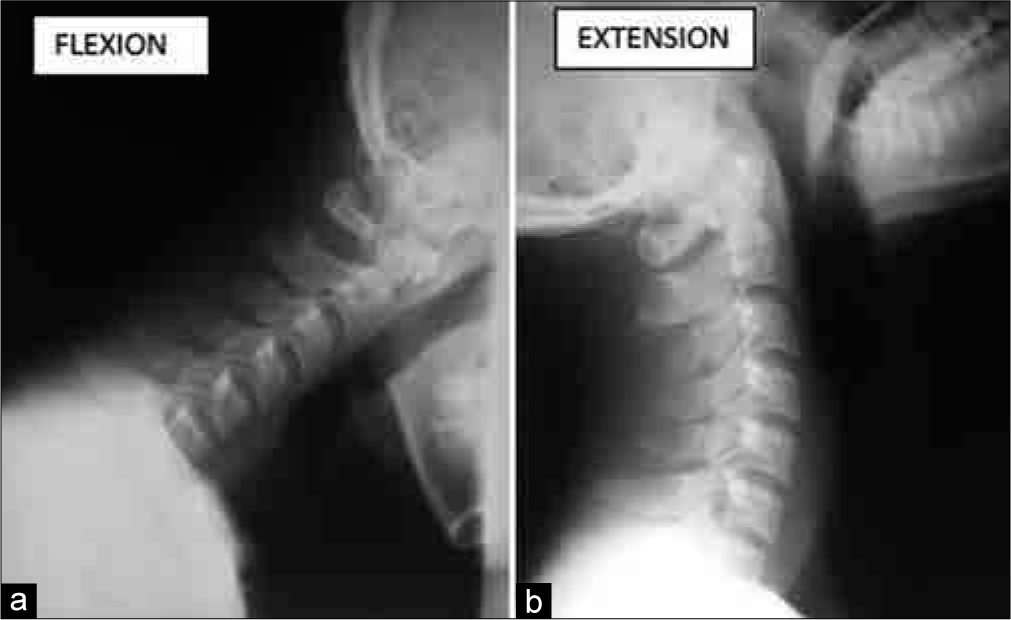
Case Description: A 20-year-old man presented to our facility with severe head injury GCS 8. Craniocervical CT scan reported 75% C3 on C4 anterior subluxation and urgent spinal stabilization surgery was recommended. A static lateral cervical spine X-ray showed normal bony alignment. He was successfully managed and dynamic studies after recovery were normal.
Conclusion: Cervical spine CT motion artifact can lead to unneeded surgery but routine clinical evaluation and cervical spine static and dynamic X-rays may be sufficient to resolve the puzzle.
Keywords: Cervical spine X-ray, Cervical spine, Computed tomography, Head injury, Motion artifact
INTRODUCTION
Evaluation of patient with severe traumatic brain injury is not complete until cervical spine is screened.[
Routine spine X-ray has been replaced with more sophisticated computed tomography in evaluation of spine trauma.[
CASE REPORT
A 20-year-old man brought to our facility unconscious following rider motorcycle accident. Examination revealed a young man unconscious with Glasgow Coma Score of 8. Both pupils were 3 mm and briskly reactive to light. He moves all limbs spontaneously. There was left parieto-occipital scalp abrasion. Examination of other systems was normal.
Clinical diagnosis of severe head injury was made. Cranial CT scan showed left parietal skull fracture with underlying punctate cerebral contusions. Cervical spine CT scan [
DISCUSSION
The role of routine history and physical examination in the management of patient with traumatic brain injury cannot be replaced but complimented by the neuroimaging facilities.[
The impact of CT artifact on the patient may include unneeded surgery, transfer to another facility and delay in critical decision making due to fear of secondary cervical spinal cord injury.[
Static and dynamic cervical spine radiograph with or without cervical spine MRI is usually adequate to exclude cervical spine CT artifact mimicking cervical spine injury.[
CONCLUSION
Cervical spine CT artifact can lead to unneeded surgery but routine clinical evaluation and supine static cervical spine X-rays may be sufficient to resolve the puzzle.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bastos MD, Lee EY, Strauss KJ, Zurakowski D, Tracy DA, Boiselle PM. Motion artifact on high-resolution CT images of pediatric patients: Comparison of volumetric and axial CT methods. Am J Roentgenol. 2009. 193: 1414-8
2. Boas FE, Fleischmann D. CT artifacts: Causes and reduction techniques. Imaging Med. 2012. 4: 229-40
3. Ertel AE, Robinson BR, Eckman MH. Cost-effectiveness of cervical spine clearance interventions with litigation and long-term-care implications in obtunded adult patients following blunt injury. J Trauma Acute Care Surg. 2016. 81: 897-904
4. Holly L, Kelly D, Counelis G, Blinman T, McArthur D, Cryer H. Cervical spine trauma associated with moderate and severe head injury: Incidence, risk factors, and injury characteristics. J Neurosurg. 2002. 96: 285-91
5. Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: A meta-analysis. J Trauma. 2005. 58: 902-5
6. Nazir M, Khan SA, Raja RA, Bhatti SN, Ahmed E. Cervical spinal injuries in moderate to severe head injuries. J Ayub Med Coll Abbottabad. 2012. 24: 100-2
7. Patel SH, Moore TA. Motion artifact on computed tomography scan suggesting an unstable 3-column spine injury: Case report of a “near miss” root cause of unneeded surgery. Patient Saf Surg. 2013. 7: 35
8. Ritchie CJ, Crawford CR, Godwin JD, King KF, Kim Y. Correction of computed tomography motion artifacts using pixel-specific back-projection. IEEE Trans Med Imaging. 1996. 15: 333-42
9. Sugimoto Y, Ito Y, Shiozaki Y, Shimokawa T, Mazaki T. Motion induced artifact mimicking cervical dens fracture on the CT Scan: A case report. Asian Spine J. 2012. 6: 216-8
10. Vahldiek JL, Thieme S, Hamm B, Niehues SM. Incidence of combined cranial and cervical spine injuries in patients with blunt minor trauma: Are combined CT examinations of the head and cervical spine justified?. Acta Radiol. 2016. 58: 856-60
11. Zhang D, Marques L, Serafim A, Cabral J. Computed tomography artifacts mimicking Type II odontoid fractures: Report of two cases and review of the literature. Interdiscip Neurosurg Adv Tech Case Manag. 2020. 19: 1-5