- Department of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, United States.
- Department of Neurosurgery, Erie County Medical Center, Buffalo, New York, United States.
- Department of Diagnostic Radiology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, United States.
- Department of Radiology, Eric County Medical Center, Buffalo, New York, United States.
Correspondence Address:
Richard M. Spiro, Department of Neurosurgery, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, Buffalo, New York, United States.
DOI:10.25259/SNI_480_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jaims Lim1,2, Steven B. Housley1,2, Douglas Drumsta3,4, Richard M. Spiro1,2,3. Chronic epidural hematoma presenting with diplopia. 24-Aug-2021;12:420
How to cite this URL: Jaims Lim1,2, Steven B. Housley1,2, Douglas Drumsta3,4, Richard M. Spiro1,2,3. Chronic epidural hematoma presenting with diplopia. 24-Aug-2021;12:420. Available from: https://surgicalneurologyint.com/surgicalint-articles/11065/
Abstract
Background: Epidural hematomas are common intracranial pathologies secondary to traumatic brain injuries and are associated with overlying skull fractures up to 85% of the time. Although many require immediate surgical evacuation, some are observed for stability and followed up conservatively with serial imaging or enlarge slowly overtime, similar to chronic subdural hematomas. Those in the latter category may present with vague symptoms such as diplopia or headache and are often found on routine outpatient evaluation. When concerning findings such as significant mass effect are present, surgical evacuation is necessary.
Case Description: Here, we present the case of a 32-year-old man who presented with diplopia 6 weeks after experiencing head trauma and was found to have a chronic epidural hematoma. On resection, thick, inflammatory tissue was observed and carefully resected, revealing normal dura underneath. Six weeks after evacuation of the hematoma, the patient had near-complete resolution of his diplopia and complete resolution of his epidural hematoma.
Conclusion: Given the consistency and nature of the fibrous material observed intraoperatively in this case, near-complete resection of the tissue was likely necessary to help facilitate adequate reexpansion of brain parenchyma and improve clinical outcomes.
Keywords: Chronic epidural hematoma, Diplopia, Hemorrhage
INTRODUCTION
Epidural hematomas are common intracranial pathologies secondary to traumatic brain injuries and are associated with overlying skull fractures up to 85% of the time.[
We present an interesting case involving a 32-year-old man who presented with diplopia 6 weeks after experiencing head trauma and physical assault and was subsequently found to have a large left chronic epidural hematoma that was rim enhancing on computed tomography (CT) and T1 rim hyperintense and T1 core heterointense on magnetic resonance imaging (MRI). Given the significant mass effect, the hematoma was surgically evacuated.
CASE DESCRIPTION
A 32-year-old man with a remarkable history of polysubstance abuse presented to the emergency room with a 2-week history of diplopia. Six weeks earlier, the patient had presented to the emergency department after being found unconscious secondary to a suspected drug overdose and a question of possible physical assault and head injury. Toxicology panel was positive for cocaine, cannabinoids, and opioids. The patient was observed and improved, returning to his neurological baseline level after overnight monitoring. He was unable to recall additional details of the event and was discharged the day after his presentation. Cranial imaging during this initial encounter was not obtained by the trauma team. Approximately 4 weeks after his initial presentation, the patient reported to his primary care physician because he was experiencing diplopia. Brain MRI was obtained as part of an outpatient workup 2 weeks following symptom onset, and the sagittal T1 sequence revealed an abnormal rim – hyperintense core – heterointense lesion on the sagittal T1 sequence [
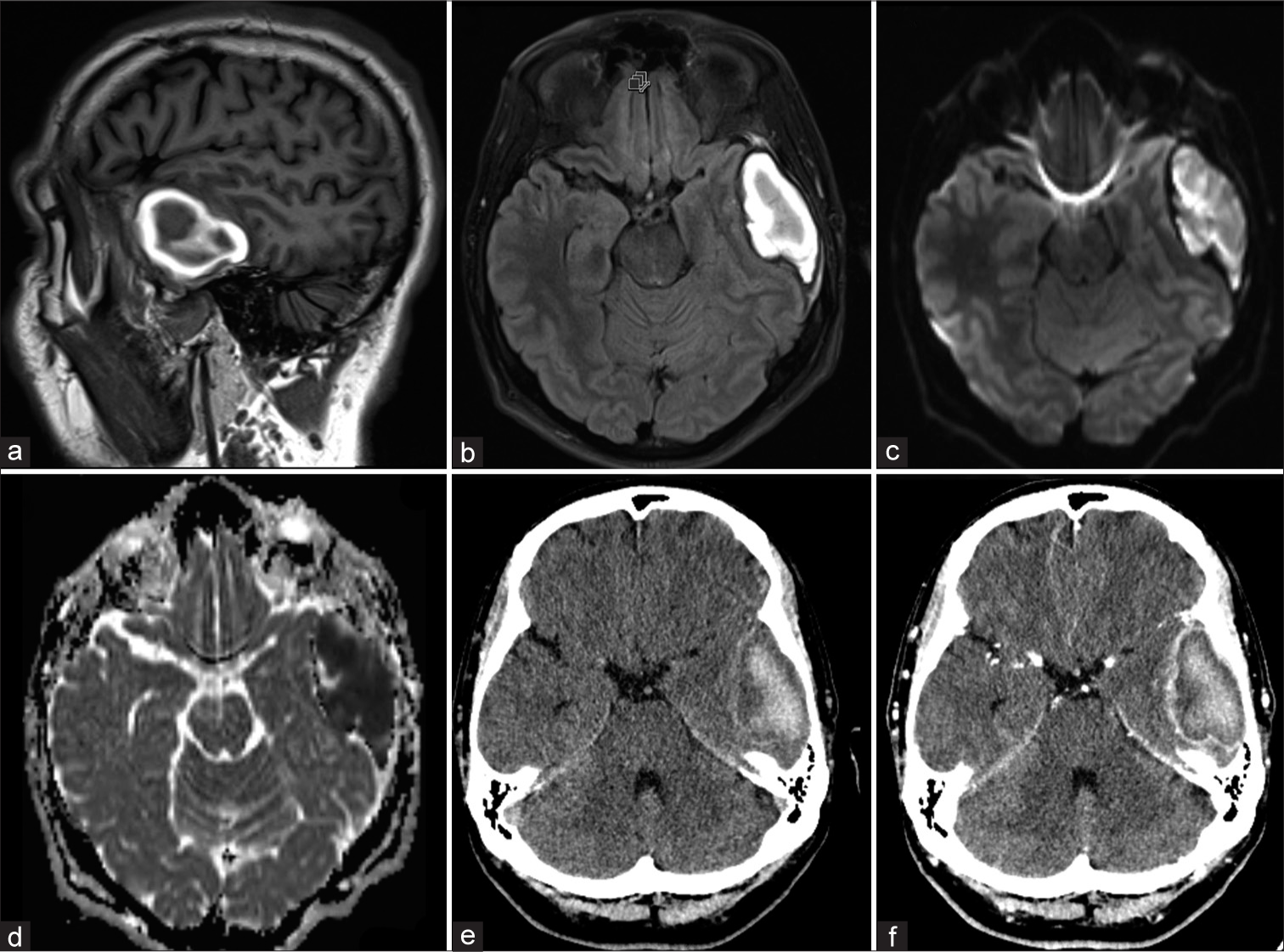
Figure 1:
Preoperative imaging of the head and brain. Magnetic resonance imaging of the brain shows a sagittal T1 sequence hyperintense rim and heterointense core (a) and a T2 fluid-attenuated inversion recovery sequence revealing a hyperintense (b) lesion. Diffusion restricting (c) and apparent diffusion coefficient (d) images, respectively, demonstrate a hyperintense and hypointense lesion. Computed tomography images of the head with (e) and without (f) contrast enhancement highlight a hyperdense lesion in the left temporal region.
At the time of neurosurgical evaluation, the patient complained of double vision with downward gaze in the bilateral lower visual quadrants. He denied any alleviating or exacerbating factors and described it as constant throughout the day. The patient was otherwise healthy, with no other medical conditions. Contrast-enhanced CT of the head was obtained to assess for the progression or change in the lesion observed on MRI and demonstrated the similar contrast rim-enhancing lesion with significant surrounding mass effect [
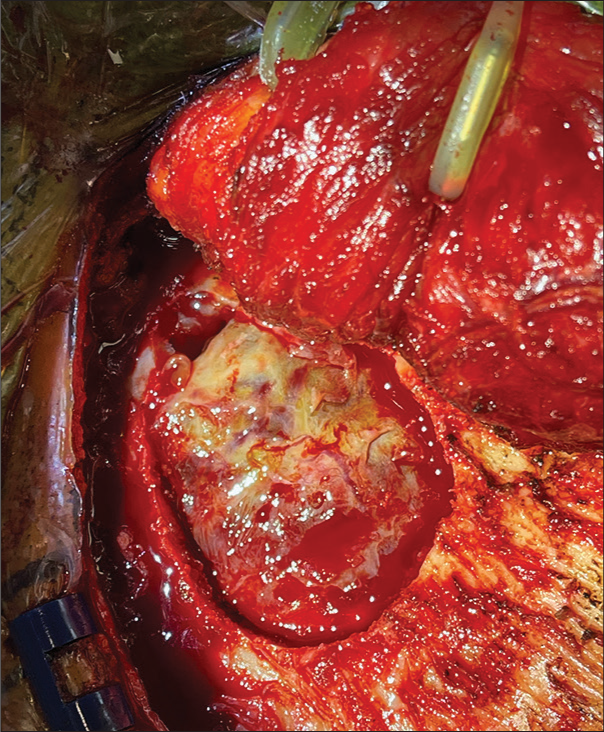
Due to the significant size and mass effect on the left midbrain in addition to the diplopia, the patient was taken for a left temporal craniotomy for evacuation and removal of the lesion. A small temporal craniotomy was performed. On removal of the bone flap, normal dura was not clearly visualized. Instead, a rather thick, yellow fibrous-like tissue was observed [
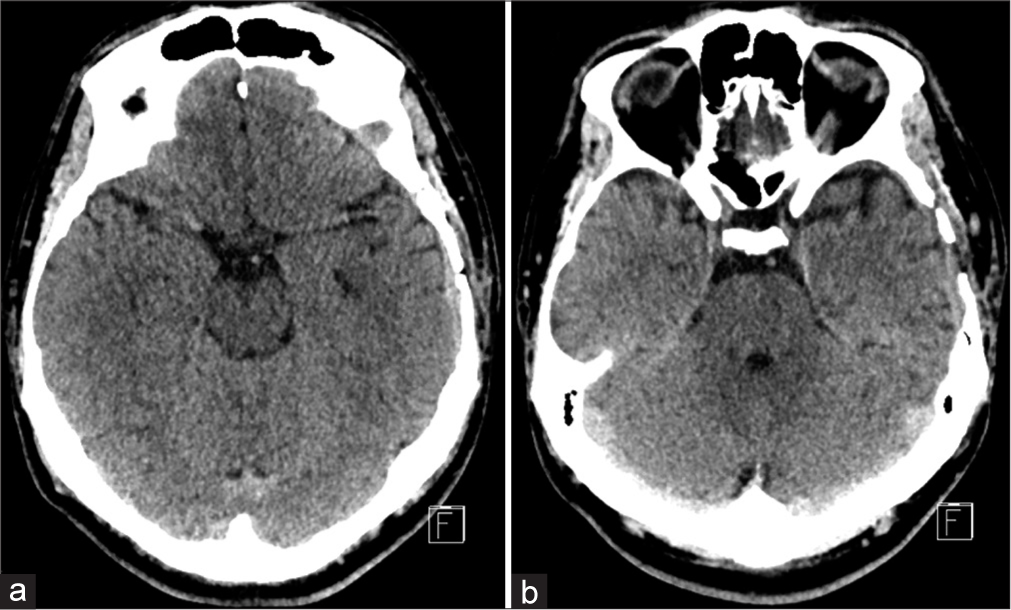
Postoperatively, the patient remained neurologically unchanged and was observed in the intensive care unit for 2 days. On postoperative day 1, a CT scan of the head showed gradual parenchymal expansion into the void that had previously been occupied by the hematoma. The patient was discharged on postoperative day 5. At the 6-week postoperative follow-up visit, he had near-complete resolution of his diplopia and complete resolution of his epidural hematoma on head CT [
DISCUSSION
We present the case of a 32-year-old man who initially presented to the emergency department after being found unconscious. His condition raised suspicions of a possible drug overdose and/or physical assault. The patient was neurologically intact during the initial visit, and cranial imaging was not obtained. If cranial imaging had been obtained during this initial visit and a large acute epidural hematoma had been visualized that met the operative criteria of being larger than 30 ml or causing brainstem compression or herniation, the hematoma might have been surgically evacuated. No imaging was obtained until the patient developed diplopia 6 weeks after experiencing the traumatic event and was subsequently found to have a large left chronic epidural hematoma during an outpatient evaluation. Traumatic chronic epidural hematomas may present at various intervals within their natural history. Common presenting symptoms include headache and/or decreased level of consciousness, but the neurological deficits on presentation are based on the location and size of the hematoma.[
Chronic epidural hematomas on CT
Chronic epidural hematomas are described on CT imaging as being of mixed density or radiolucent with contrast-enhancing membranes.[
Chronic epidural hematomas on MRI
The appearance of chronic epidural hematomas on MRI is not well described in the literature due to the overall rarity of the condition and the lack of an opportunity to obtain an MRI due to the need for immediate surgical intervention. Klepinowski et al. described a case of a vertex epidural hematoma that was MRI T1 isointense and T2 heterointense.[
Although our patient had a history of trauma and lacked any clinical signs? or symptoms? of infection, our patient also had a history of polysubstance abuse, and concern for an epidural abscess was raised. Due to the patient’s diplopia and symptomatic left midbrain compression secondary to mass effect and temporal lobe herniation from the hematoma, surgical evacuation was recommended.
Intraoperative findings and management
Neither clear bleeding sources nor signs of purulence or infection were identified during the evacuation in our case. Iwakuma and Brunngraber described the largest to date series of 21 patients with chronic epidural hematomas, and no sources of hemorrhage were identified in 13 of 20 cases.[
A thick capsule of inflammatory tissue that was very adherent to the dura was encountered after the bone flap was removed. It is well known that the dura mater is highly vascularized and responds to injury through inflammation, repair, and remodeling, but the exact mechanism of inflammatory tissue propagation and encapsulation is not well understood. This thick inflammatory capsule has been suggested to form due to the formation of a fibroblast layer of tissue around the hematoma and outer layer of dura.[
Although there are no clear guidelines for the management of chronic epidural hematomas, patients presenting more than 2 weeks after the initial injury will likely have an element of calcification and encapsulation around the hematoma based on prior reports and our case description.[
CONCLUSION
Patients with chronic intracranial epidural hematomas following trauma can have various presentations ranging from chronic headache to altered mentation to cranial nerve palsies and, rarely, with diplopia as the only symptom. CT imaging obtained 2 weeks postinjury will likely show hyperdense rim formation with ossification secondary to inflammation, and MRI will demonstrate varying T1 and T2 intensities. Removal of the thick, fibrous capsule may be critical to allow for proper parenchyma reexpansion, reduction of mass effect, and complete clinical and imaging resolution.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bonilha L, Mattos JP, Borges WA, Fernandes YB, Andrioli MS, Borges G. Chronic epidural hematoma of the vertex. Clin Neurol Neurosurg. 2003. 106: 69-73
2. Cambria S, Marra GA, di Perri R, Bramanti P. Ossified epidural hematoma, Report of a case with epilepsy. J Neurosurg Sci. 1985. 29: 285-8
3. de Oliveira Sillero R, Zanini MA, Gabarra RC. Large chronic epidural hematoma with calcification: A case report. J Trauma. 2008. 64: 1619-21
4. Hirsh LF. Chronic epidural hematomas. Neurosurgery. 1980. 6: 508-12
5. Iwakuma T, Brunngraber CV. Chronic extradural hematomas. A study of 21 cases. J Neurosurg. 1973. 38: 488-93
6. Kaufman HH, Herschberger J, Kopitnik T, McAllister P, Hogg J, Conner T. Chronic extradural haematomas: Indications for surgery. Br J Neurosurg. 1992. 6: 359-64
7. Kaye EM, Cass PR, Dooling E, Rosman NP. Chronic epidural hematomas in childhood: Increased recognition and non-surgical management. Pediatr Neurol. 1985. 1: 255-9
8. Kim do Y, Jung JH, Kim DY, Seung WB, Park YS. Rapid ossification of epidural hematoma in a child: A case report. Korean J Neurotrauma. 2014. 10: 152-4
9. Klepinowski T, Kawalec P, Larysz M, Sagan L. Acute-on-chronic vertex epidural hematoma with diastasis of the sagittal suture in an adult. World Neurosurg. 2020. 139: 245-9
10. McLaurin RL, Ford LE. Extradural hematoma; statistical survey of forty-seven cases. J Neurosurg. 1964. 21: 364-71
11. Miller DJ, Steinmetz M, McCutcheon IE. Vertex epidural hematoma: Surgical versus conservative management: Two case reports and review of the literature. Neurosurgery. 1999. 45: 621-4
12. Nagane M, Oyama H, Shibui S, Nomura K, Nakanishi Y, Kamiya M. Ossified and calcified epidural hematoma incidentally found 40 years after head injury: Case report. Surg Neurol. 1994. 42: 65-9
13. Perera S, Keogh AJ. Chronic simultaneous bilateral extradural haematomas. Br J Neurosurg. 1995. 9: 533-5
14. Rosenthal AA, Solomon RJ, Eyerly-Webb SA, Sanchez R, Lee SK, Kiffin C. Traumatic epidural hematoma: Patient characteristics and management. Am Surg. 2017. 83: e438-40
15. Tuncer R, Kazan S, Ucar T, Acikbas C, Saveren M. Conservative management of epidural haematomas, Prospective study of 15 cases. Acta Neurochir (Wien). 1993. 121: 48-52
16. Umana GE, Cristaudo C, Scalia G, Passanisi M, Corsale G, Tomarchio L. Chronic epidural hematoma caused by traumatic intracranial pseudoaneurysm of the middle meningeal artery: Review of the literature with a focus on this unique entity. World Neurosurg. 2020. 136: 198-204
17. Watanabe T, Nakahara K, Miki Y, Shibui S, Takakura K, Nomura K. Chronic expanding epidural haematoma. Case report. Acta Neurochir (Wien). 1995. 132: 150-3
18. Zimmerman RA, Bilaniuk LT. Computed tomographic staging of traumatic epidural bleeding. Radiology. 1982. 144: 809-12