- Department of Neurosurgery, Henry Ford Hospital, Detroit, Michigan, USA
- Department of Orthopedic Surgery, Henry Ford Hospital, Detroit, Michigan, USA
Correspondence Address:
Azam Basheer
Department of Neurosurgery, Henry Ford Hospital, Detroit, Michigan, USA
DOI:10.4103/sni.sni_171_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Azam Basheer, Mohamed Macki, Morenikeji Buraimoh, Asim Mahmood. Chronic thoracolumbar subdural empyema: Case report and surgical management. 01-Aug-2017;8:167
How to cite this URL: Azam Basheer, Mohamed Macki, Morenikeji Buraimoh, Asim Mahmood. Chronic thoracolumbar subdural empyema: Case report and surgical management. 01-Aug-2017;8:167. Available from: http://surgicalneurologyint.com/surgicalint-articles/chronic-thoracolumbar-subdural-empyema-case-report-and-surgical-management/
Abstract
Background:Spinal cord abscesses and spinal subdural empyemas are rare and difficult to treat.
Case Description:A 35-year-old male presented to an outside institution with 2 months of progressive low back pain, weakness, and bowel incontinence; he was diagnosed with an L4 epidural abscess that was poorly managed. When the patient presented to our institution, magnetic resonance imaging (MRI) revealed a well-organized chronic subdural abscess at the thoracolumbar junction. Following resection, his back pain resolved but he was left with a residual paraparesis.
Conclusion:Subdural abscesses are rare and should be considered among the differential diagnoses for intraspinal mass lesions. Treatment should include prompt surgical exploration and decompression combined with appropriate prolonged antibiotic treatment.
Keywords: Chronic spinal subdural abscess, epidural abscess, spinal subdural abscess, spinal subdural empyema
INTRODUCTION
Chronic spinal subdural abscesses are rare. They are typically intradural/extramedullary and are only rarely intramedullary in location.[
CASE REPORT
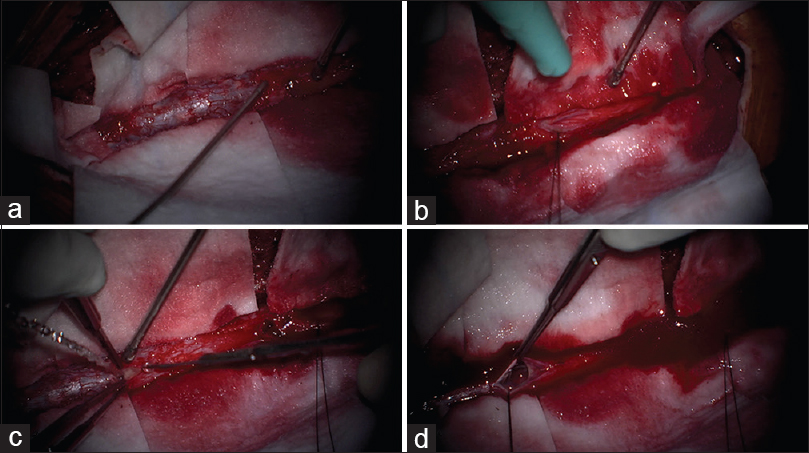
Initial presentation
A 35-year-old male, with a history of intravenous drug and cocaine abuse, presented to an outside hospital with back pain, bilateral lower extremity numbness, and bladder incontinence. When magnetic resonance imaging (MRI) revealed a possible epidural collection around the lamina of L4, a lumbar puncture (LP) was performed. The LP revealed numerous polymorphonuclear leukocytes (PMNs); the cerebrospinal fluid gram staining and cultures were negative. The patient underwent an L4 laminectomy, however, no purulence was encountered in the epidural space. Only reactive fibrous tissue and a markedly thickened dura were identified. Despite a negative biopsy and no growth on cultures, the patient was empirically treated with vancomycin for four weeks (e.g., presumptive Staphylococcal and Streptococcal species).
Second presentation
Two months later, with progressive lower extremity pain, weakness (4/5 mid/distal lower extremities bilaterally), and continued bladder and bowel incontinence, the patient presented to our institution [
New magnetic resonance imaging
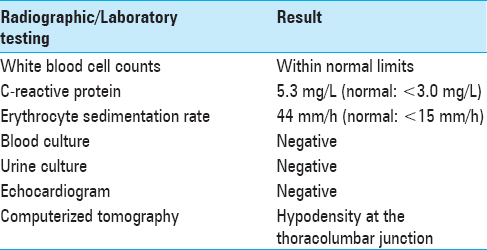
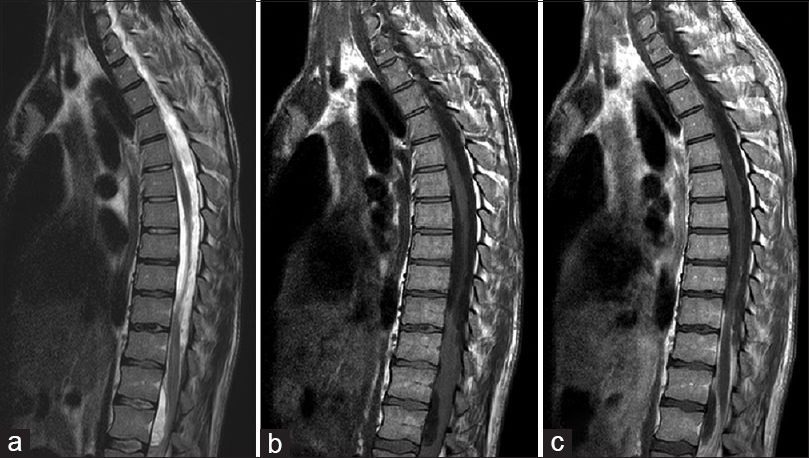
The new contrast-enhanced high-resolution MRI of the whole neuraxis demonstrated multiple foci of subdural empyema. There were heterogeneous pockets of enhancement along the ventral and dorsal leptomeninges of the cervical and thoracic and lumbar spine (e.g., involving the nerve roots of the cauda equina) [
Figure 1
(a) T2 sagittal MRI: extensive loculated fluid collections compressing the spinal cord ventrally at T12-L2 and dorsally at T8-T12 level. Note T2 cord signal change within the distal thoracic cord/conus at T11-T12. (b) T1 sagittal MRI without contrast: anterior displacement of the cord from T9-T12 level. (c) T1 Sagittal MRI with contrast: distinct enhancement of the fluid collections at T8-T12, T12-L2 and leptomeninges/nerve roots in the cauda equina
Surgery
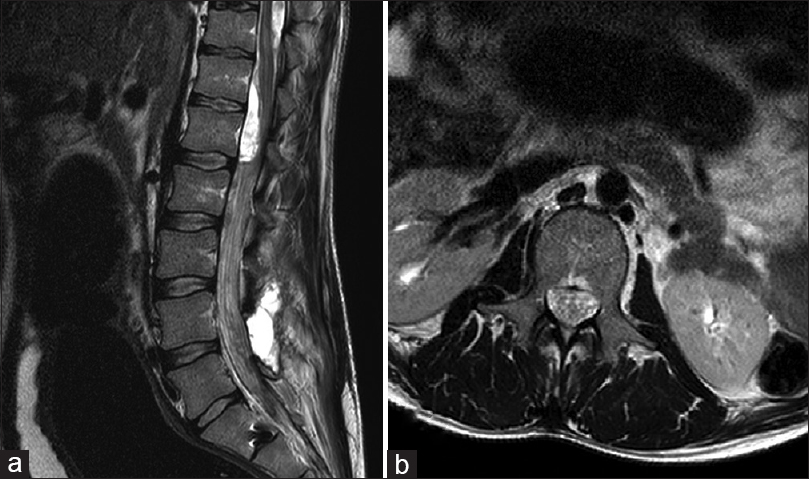
The patient underwent an emergent laminectomy from T10 to L2. No epidural abscess was seen, but the thecal sac appeared tense. A durotomy started at the L2 level and extended superiorly revealed a lobulated lesion in the intradural space and terminal filum. This phlegmon was tightly attached to the spinal cord and neighboring nerve roots by fibrotic gliotic tissue [
Figure 3
Intraoperative images. (a) Tense, thickened dura without any epidural abscess. (b) The dural opening at L2 showed nerve root clumping with very little cerebrospinal fluid egress/phlegmon. (c) Second dural opening at T10 showed purulent discharge. (d) Intradural spinal cord thickening/adhesions
Pathology
Histologic examination showed an organized abscess (e.g., marked infiltration of plasma and lymphocytes). Although the gram and acid-fast bacilli (AFB) stains were negative, as were the cultures, the patient was presumptively started on a 6-week course of vancomycin and ertapenem. At 6-week follow-up, his weakness remained stable but his back pain resolved. Furthermore, the white blood cell count was normal. A follow-up MR was not available at this time.
DISCUSSION
Spinal subdural empyema is rare and is typically attributed to Staphylococcus aureus (over 50% of cases).[
Four mechanisms contribute to the development of these lesions; direct spread of infection can occur secondary to congenital deformities (dysraphism), hematogenous spread from a distant site, iatrogenic contamination of the subdural space (33%), and/or contiguous spread from adjacent infection.
Symptoms of chronic subdural abscesses are typically nonspecific and sometimes even absent.[
Although the best practice for treating subdural infections has not been well-established, the goals of surgical washout include lowering the infectious burden and obtaining culture diagnosis. Furthermore, most decompressions include consecutive or “skip” laminectomies with consecutive or skip durotomies to ensure adequate debridement of these potentially extensive lesions.
CONCLUSION
Diabetes, intravenous drug abuse (IVDA), and immunocompromise are known risk factors for a spinal subdural abscess. This diagnosis should be considered if patients present with evidence of infection. Contrast-enhanced high-resolution MRI scans of the entire neuraxis allow the surgeon to distinguish between subdural and epidural lesions. These should be promptly explored, decompressed/washed out, and followed with appropriate long-term antibiotic treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Diehn FE. Imaging of spine infection. Radiol Clin North Am. 2012. 50: 777-98
2. Semlali S, Akjouj S, Chaouir S, Hanine A, Ben Ameur M. Spinal subdural tuberculous abscess in a patient with tuberculous meningitis. J Radiol. 2007. 88: 280-1
3. Sorar M, Er U, Seckin H, Ozturk MH, Bavbek M. Spinal subdural abscess: A rare cause of low back pain. J Clin Neurosci. 2008. 15: 292-4
4. Velissaris D, Aretha D, Fligou F, Filos KS. Spinal Subdural Staphylococcus Aureus Abscess: Case report and review of the literature. World J Emerg Surg. 2009. 4: 31-
5. Vural M, Arslantas A, Adapinar B, Kiremitci A, Usluer G, Cuong B. Spinal subdural Staphylococcus aureus abscess: Case report and review of the literature. Acta Neurol Scand. 2005. 112: 343-6
6. Zemmoura I, Hamlat A, Morandi X. Intradural extramedullary spinal inflammatory myofibroblastic tumor: Case report and literature review. Eur Spine J. 2011. 20: S330-5