- Departments of Neurosurgery, University of California, Los Angeles.
- Departments of Anesthesiology, University of California, Los Angeles.
Correspondence Address:
Luke Macyszyn
Departments of Neurosurgery, University of California, Los Angeles.
DOI:10.25259/SNI_374_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kevin Mckay, Mark Attiah, Tianyi Niu, Daniel Nagasawa, Kunal Patel, Bilwaj Gaonkar, Barbara Van de Wiele, Natalie Moreland, Alexander Tucker, Pedro Churchman, Ulrich Batzdorf, Luke Macyszyn. Clinical and surgical management of holocervical spinal cord ependymomas. 22-Nov-2019;10:223
How to cite this URL: Kevin Mckay, Mark Attiah, Tianyi Niu, Daniel Nagasawa, Kunal Patel, Bilwaj Gaonkar, Barbara Van de Wiele, Natalie Moreland, Alexander Tucker, Pedro Churchman, Ulrich Batzdorf, Luke Macyszyn. Clinical and surgical management of holocervical spinal cord ependymomas. 22-Nov-2019;10:223. Available from: http://surgicalneurologyint.com/surgicalint-articles/9766/
Abstract
Background: Spinal ependymomas are rare tumors of the central nervous system, and those spanning the entire cervical spine are atypical. Here, we present two unusual cases of holocervical (C1-C7) spinal ependymomas.
Case Description: Two patients, a 32-year-old female and a 24-year-old male presented with neck pain, motor, and sensory deficits. Sagittal MRI confirmed hypointense lesions on T1 and hyperintense regions on T2 spanning the entire cervical spine. These were accompanied by cystic cavities extending caudally into the thoracic spine and rostrally to the cervicomedullary junction. Both patients underwent gross total resection of these lesions and sustained excellent recoveries.
Conclusion: Two holocervical cord intramedullary ependymomas were safely and effectively surgically resected without incurring significant perioperative morbidity.
Keywords: Ependymoma, Spinal cord tumor, Tumor cyst
INTRODUCTION
Ependymomas are exceptionally rare primary intramedullary gliomas of the central nervous system.[
CASE DESCRIPTION
Patient 1
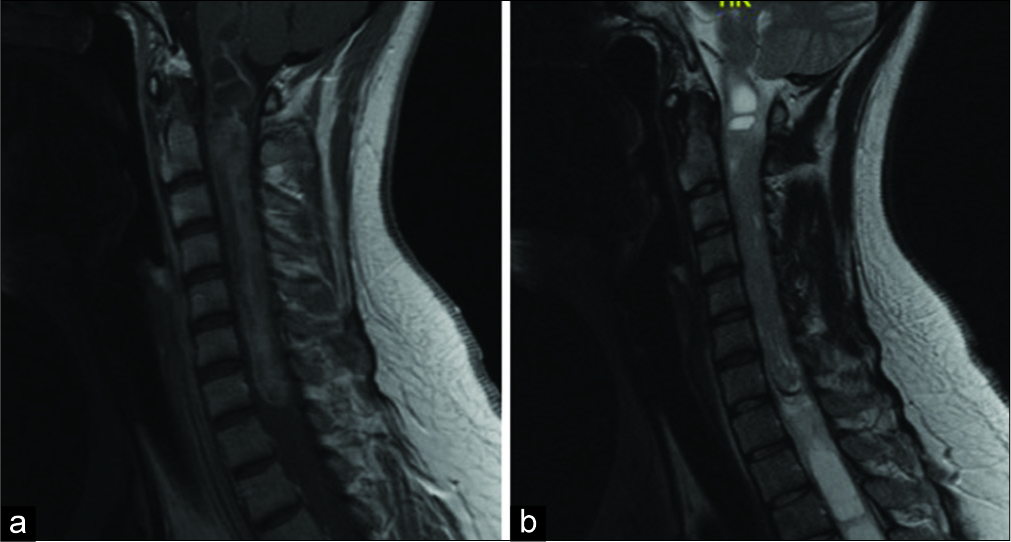
A 32-year-old female presented with severe progressive spastic quadriparesis attributed to a cervical cord intramedullary tumor (e.g., large cystic-enhancing expansile mass) extending from C1 to C7-T1 on MRI [
Figure 1:
Case 1. Preoperative MRI cervical spine T1-weighted with contrast (left) and T2 weighted (right). There is a large-enhancing expansile mass of the cervical spinal cord extending from the level C1-C7 measuring 9.8 × 1.2 cm. A large tumor cyst extends from end of mass at C7 inferiorly into the thoracic spine.
Patient 2
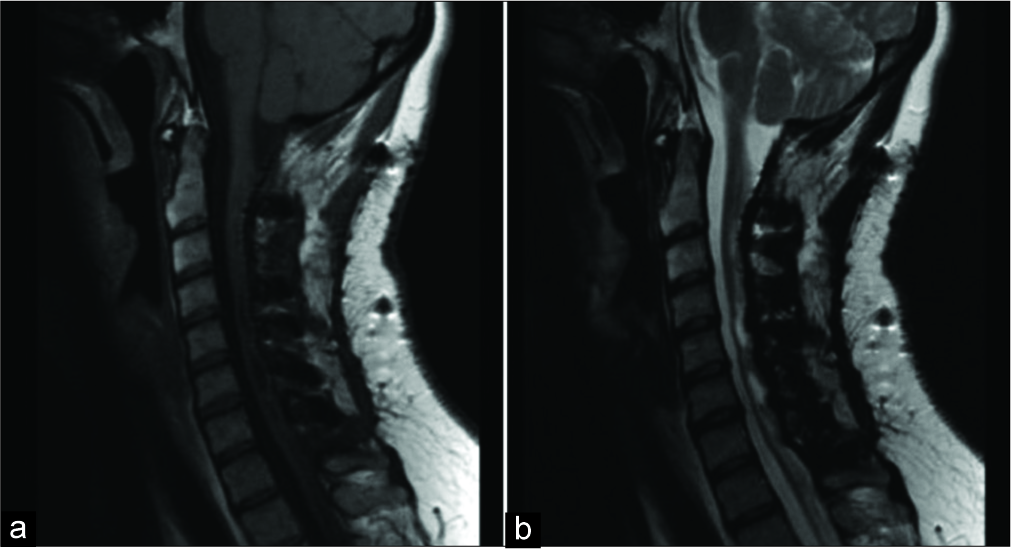
A 24-year-old male also presented with a spastic quadriparesis and cervical MR-documented cystic, enhancing, expansile intramedullary mass extending from C1-C7 [
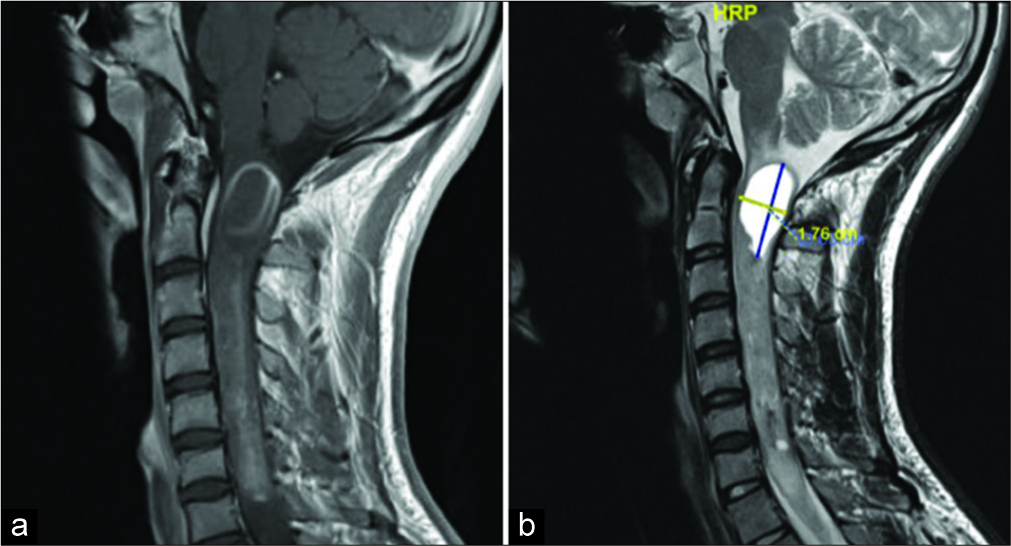
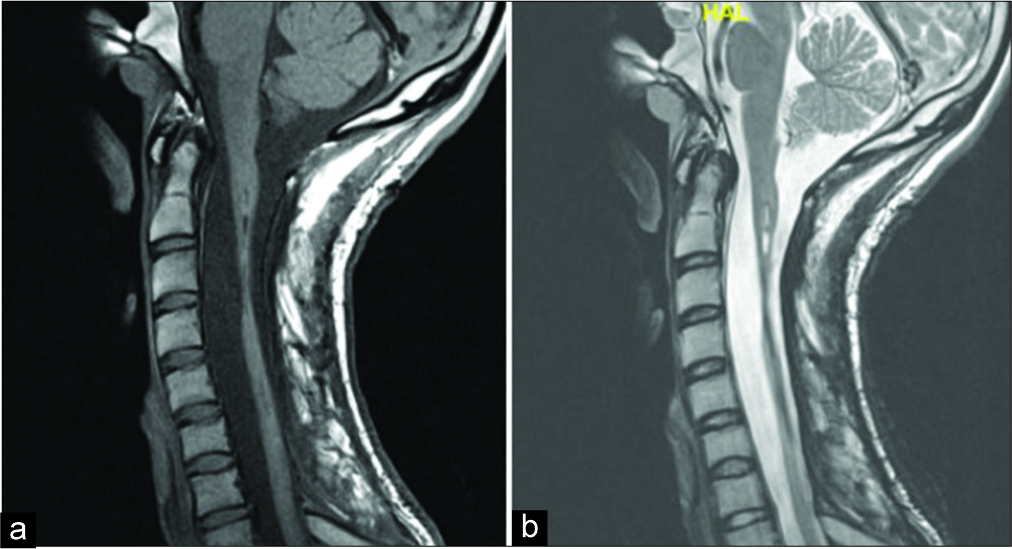
A C1-C7 laminectomy with midline myelotomy (en bloc tumor removal) and C2-C7 posterior fusion was performed. MEP’s remained unchanged during the surgery. Postoperatively, the patient showed no neurological worsening. Pathologically, this was deemed a WHO grade II ependymoma. One year later, the patient had 4+/5 motor strength in the upper extremities, intact motor strength in his lower extremities, and mild residual decreased sensation in the right C6-C7 dermatome. The 1-year postoperative cervical MRI showed no evidence of residual or recurrent tumor [
DISCUSSION
Demographics
Ependymomas tend to present more often in middle-aged adults and in the spinal cord.[
Clinical presentation
Patients commonly experience symptoms for over a year before their initial diagnosis.[
MR findings
MR imaging of spinal ependymomas demonstrates hypo- to isointensity on T1, hyperintense on T2 studies, often with a cystic component, and heterogenous enhancement with gadolinium.[
Surgical considerations and intraoperative monitoring
Both cases were performed with patient in the prone position. MEP and SSEP were used throughout. Both patients had wide laminectomies performed for adequate visualization. Following central durotomies, the spinal cords of both patients were significantly expanded. Midline myelotomies were performed in the both cases under microscopic visualization and were carried superiorly and inferiorly to the poles of the tumor. Both tumors were resected en bloc. We have found that if a favorable plane is delineated between tumor and normal tissue, internal debulking may add unnecessary time and undue cord manipulation potentially. Frequently in our practice, there is an associated cyst at the superior and inferior poles of the tumor. Care must be taken when resecting the poles of the tumors when next to a cystic cavity, as this may cause the surgeon to lose orientation, leading to inadvertent cord manipulation. At the end of the dissection/tumor removal, the arachnoid was approximated in both patients with 6-0 proline sutures, a maneuver performed to reduce pathologic traction, prevent adhesions, and reconstitute a more anatomic central canal. The extent of bony removal increases the potential for postoperative kyphosis. The risk of deformity can be mitigated by concurrently providing rigid or semirigid internal fixation, e.g., augmenting the decompression with laminoplasty or posterior lateral mass fusion.
CONCLUSION
Two patients underwent en bloc surgical resection of holocervical cord C1-C7 intramedullary WHO grade II ependymomas. Our patients had excellent recovery of neurological function up to and including their respective most recent follow-up visits at 28 and 12 months postoperatively.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Kobayashi K, Ando K, Kato F, Kanemura T, Sato K, Kamiya M. Surgical outcomes of spinal cord and cauda equina ependymoma: Postoperative motor status and recurrence for each WHO grade in a multicenter study. J Orthop Sci. 2018. 23: 614-21
2. Kobayashi K, Ando K, Kato F, Kanemura T, Sato K, Kamiya M. MRI characteristics of spinal ependymoma in WHO grade II: A review of 59 cases. Spine (Phila Pa 1976). 2018. 43: E525-30
3. Kucia EJ, Bambakidis NC, Chang SW, Spetzler RF. Surgical technique and outcomes in the treatment of spinal cord ependymomas, part 1: Intramedullary ependymomas. Neurosurgery. 2011. 68: 57-63
4. Wild F, Hartmann C, Heissler HE, Hong B, Krauss JK, Nakamura M. Surgical treatment of spinal ependymomas: Experience in 49 patients. World Neurosurg. 2018. 111: e703-9
5. Wostrack M, Ringel F, Eicker SO, Jägersberg M, Schaller K, Kerschbaumer J. Spinal ependymoma in adults: A multicenter investigation of surgical outcome and progression-free survival. J Neurosurg Spine. 2018. 28: 654-62