- Department of Orthopaedic, Spine Division, P.D. Hinduja National Hospital and Medical Research Centre, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_839_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Pratik Patel, Dhanish Mehendiratta, Vivek Bhambhu, Samir Dalvie. Clinical outcome of intradural extramedullary spinal cord tumors: A single-center retrospective analytical study. 08-Apr-2021;12:145
How to cite this URL: Pratik Patel, Dhanish Mehendiratta, Vivek Bhambhu, Samir Dalvie. Clinical outcome of intradural extramedullary spinal cord tumors: A single-center retrospective analytical study. 08-Apr-2021;12:145. Available from: https://surgicalneurologyint.com/surgicalint-articles/10698/
Abstract
Background: Intradural extramedullary spinal cord tumors (IESCT) account for approximately two-thirds of largely benign intraspinal neoplasms. They occasionally present with acute neurological deterioration warranting emergent surgical intervention.
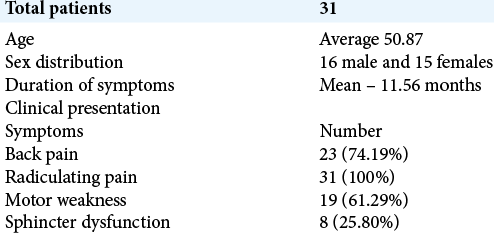
Methods: Here, we reviewed a series of 31 patients with intradural extramedullary spinal tumors who underwent surgery from 2012 to 2019. Patients averaged 50.8 years of age, and there were 16 males and 15 females. Patients were followed for a minimum of 1 year. Multiple clinical outcome variables were studied (e.g., Karnofsky Performance Score [KPS], visual analog scale (VAS), and Frankel grade).
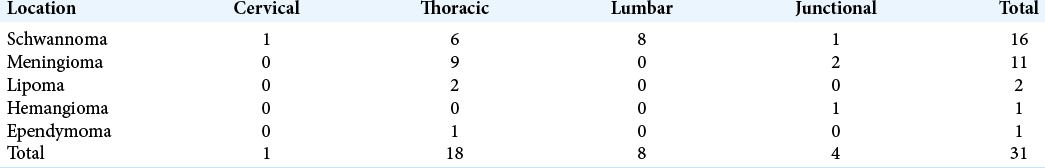
Results: The majority of IESCT tumors were found in the thoracic spine 18 (58.06%) followed by the lumbar 8 (25.80%), cervical 1 (3.22%), and combined junctional tumors 4 (12.90%) (cervicothoracic-02 and thoracolumbar-02). Histopathological diagnoses included schwannomas-16 (51.61%), meningiomas-11 (35.48%), lipomas-2 (6.45%), hemangiomas-1 (3.22), and ependymomas-01 (03.22%). The VAS score was reduced in all cases, while KPS and Frankel grades were significantly improved. Complications included cerebrospinal fluid leakage, new/residual paresthesias, and tumor recurrence (12.50%).
Conclusion: Most intradural extramedullary tumors are benign and are readily diagnosed utilizing MRI scans. Notably, good functional outcomes follow surgical intervention.
Keywords: Clinical outcome, Intradural extramedullary tumors, Spinal tumors, Surgical excision
INTRODUCTION
Primary spinal cord tumors constitute 2–4% of all central nervous system neoplasms; they are characterized as extradural, intradural extramedullary (IDEM: 65%), and intramedullary.[
MATERIALS AND METHODS
There were 31 intradural extramedullary tumors operated on between 2012 and 2019 by single surgeon. Karnofsky Performance Scores (KPSs), visual analog scales, and Frankel grades were studied pre-operatively, at the time of discharge, 3 and 12 months post-operatively. Patients averaged 50.87 years of age and included 16 males and 15 females. They were symptomatic on average for nearly a year (e.g., mean-11.56 months) before diagnosis and exhibited radiculopathy (RS: 100%), back pain (BP: 74.19%), motor deficits (MW: 61.29 %), and sphincter dysfunction (SD: 25.80 %) [
Radiological evaluation of location of tumors
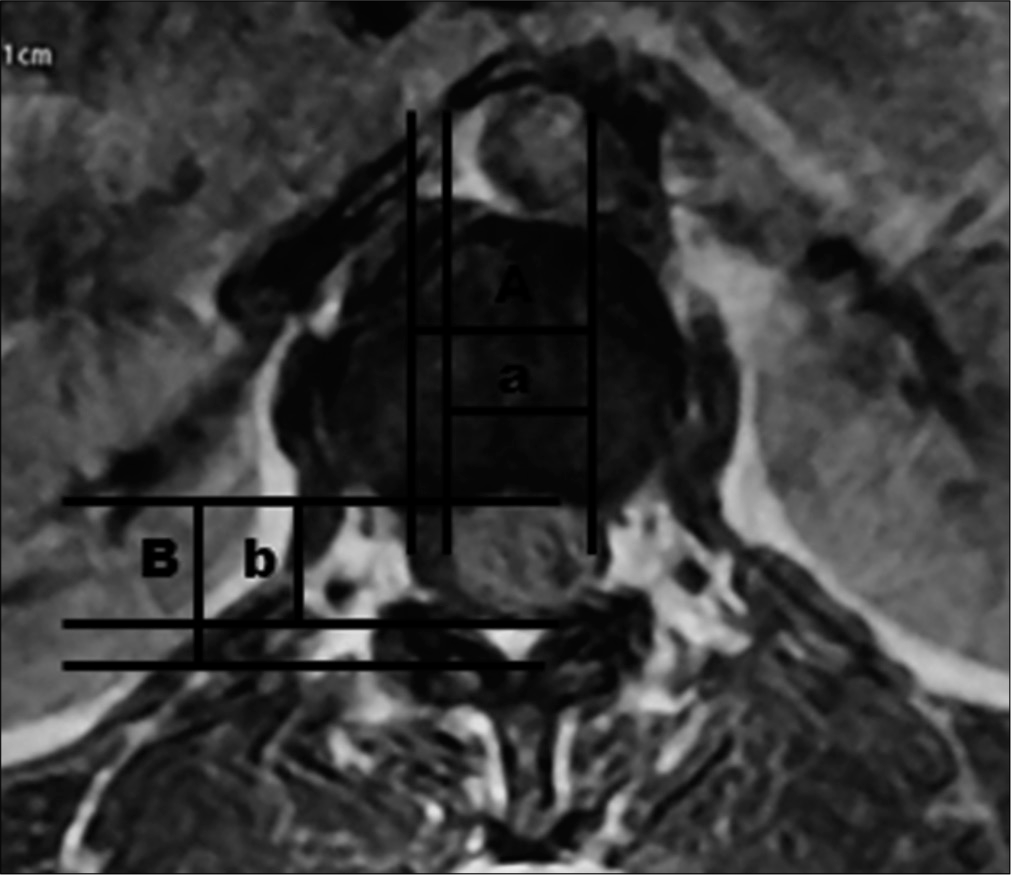
MR studies determined the location and the size of these intradural lesions (TOIDS %) [
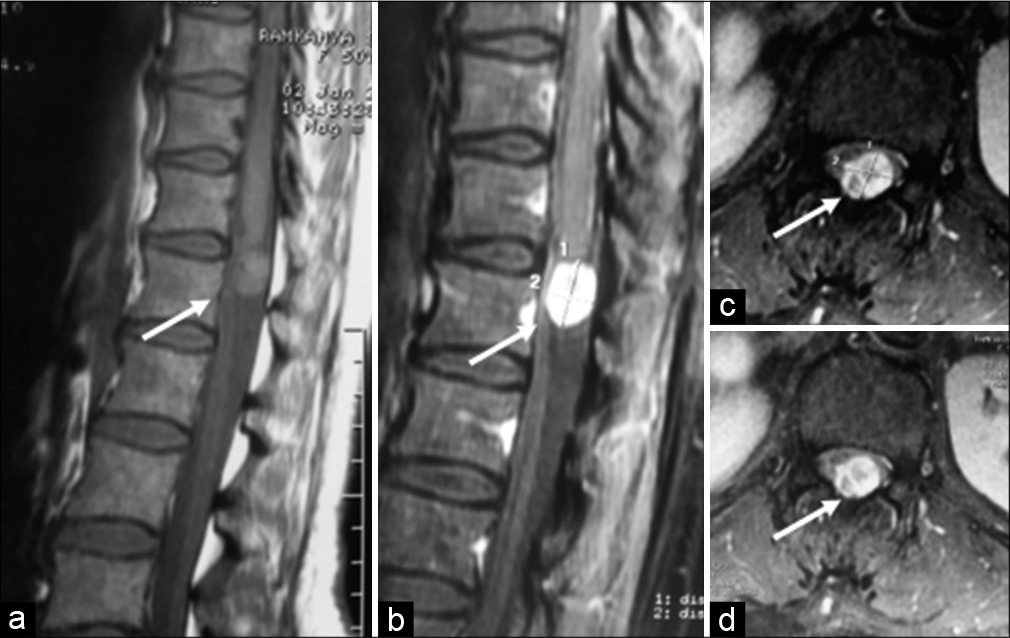
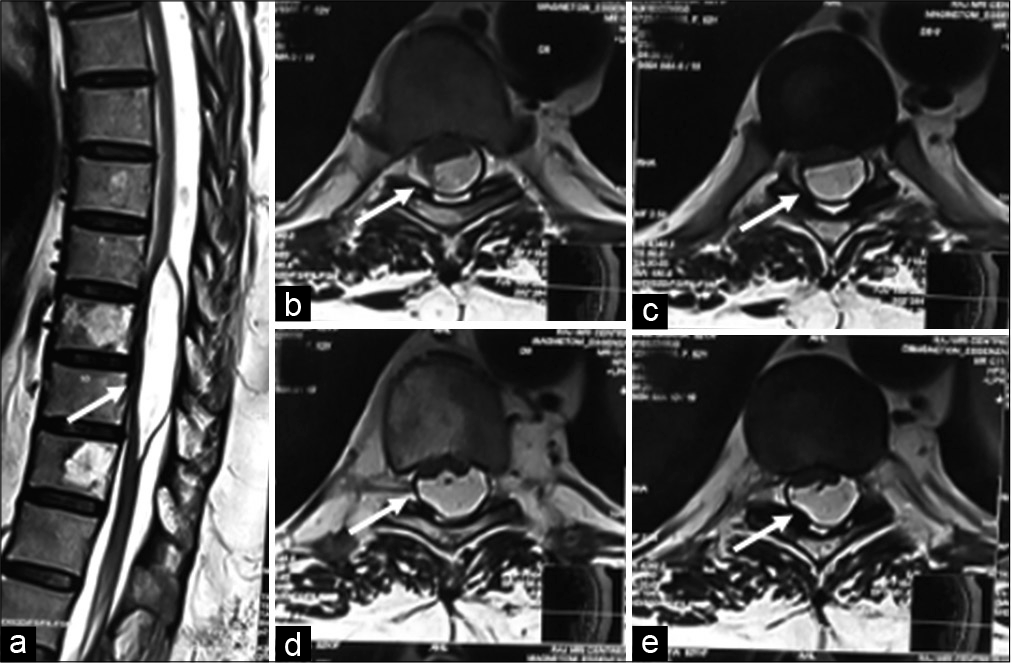
Figure 2:
Schwannoma (Arrow) – (a) (sagittal T2), (b) (post-contrast T1) lobulated heterogenous signal intensity lesion shows intense enhancement. (c) (axial T2), and (d) (post-contrast T1) lobulated heterogenous T1/T2 hyperintense intradural extramedullary lesion occupying left half of the spinal canal displacing cauda equina nerve roots toward the right.
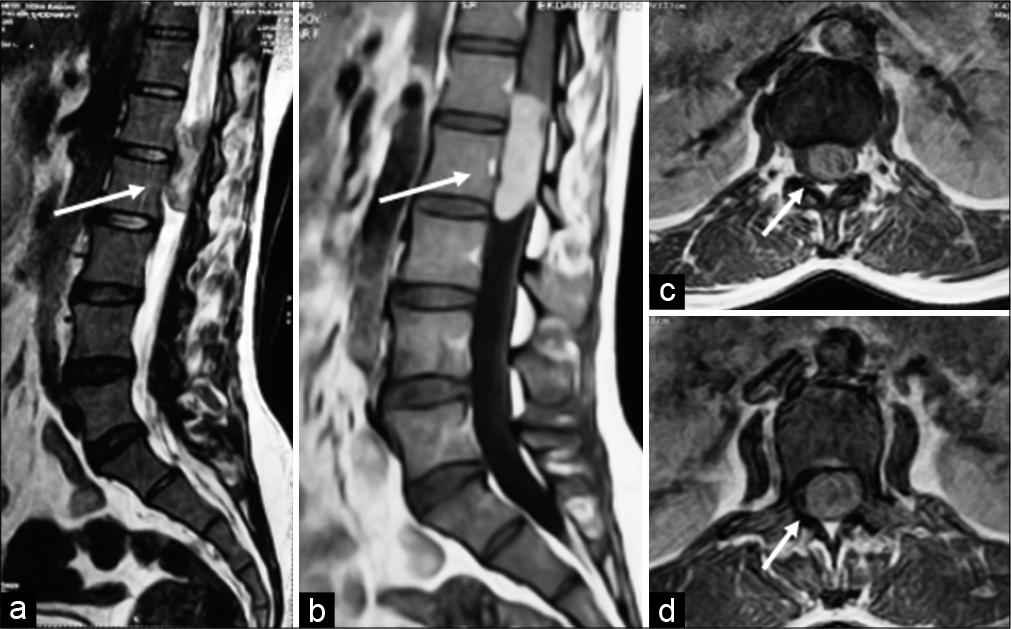
Figure 4:
Hemangioma (Arrow) – (a) (sagittal T1), (b) (post-contrast sagittal T1), and (c and d) (post-contrast axial T1 images) - Fairly marginated extramedullary intradural lesion appearing isointense to the adjacent cord on sagittal T1 sequence (3a image) occupying postero-central part of spinal canal, compresses and displaces cord anteriorly, and shows intense contrast enhancement.
Surgery for 31 intradural extramedullary tumors
Under X-ray/fluoroscopic guidance and utilizing intraoperative neural monitoring, all patients underwent laminectomies.[
Statistical analysis
The MedCalc version 19.4.0 was used. For continuous variables, means were compared using Mann–Whitney U-test, Wilcoxon signed-rank test, and Kruskal–Wallis test. Pearson’s correlation coefficient was used to calculate the correlation between tumor occupancy ratio and KPS. For categorized variables, Pearson’s chi-squared test or Fisher’s exact test were being used. P < 0.05 was considered to be statistically significant and < 0.005 as highly significant.
RESULTS
Pathology and location of intradural extramedullary tumors
The histopathological diagnoses included 16 schwannomas, 11 meningiomas, 2 lipomas, 1 hemangioma, and 1 ependymoma. Most meningiomas were located dorsally (81.81%) and schwannomas’ most common location is lower dorsal-lumbar group (93.75%).
Outcomes
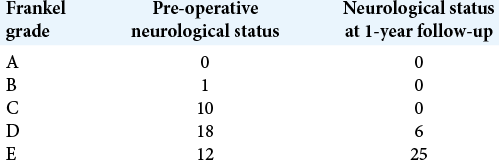
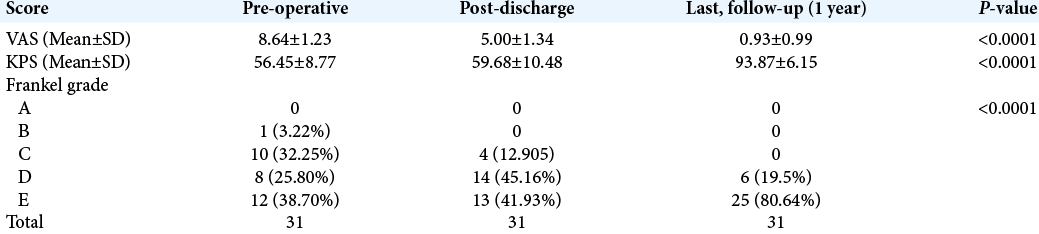
All patients’ symptoms and neurological signs improved post-operatively. There were 1 patient with Frankel’s grade B, 10 patients with grade C, 8 patients with grade D, and 12 patients with grade E pre-operatively. Post-operatively, there were 6 patients with grade D and 25 with Grade E. The pre-operative neurological deficits improved within 8 postoperative weeks in most cases and within 1 year in all cases [
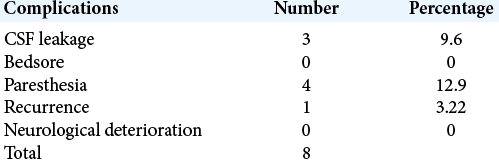
Complications
The post-operative complications included 3 CSF leaks, 4 with new or persistent paresthesias, and 1 with current tumor [
DISCUSSION
Intradural extramedullary tumors, that are typically benign, account for two-thirds of primary spinal tumors.[
Here, we retrospectively evaluated 31 cases of IDEM tumors, 27 of which were totally removed, and 4 were partially excised. The mean age of presentation in our study was 50.87 years, and the mean duration of illness was 11.56 months, most patients were male (51.61%), and no significant difference was found between the clinical presentation and duration of illness between the genders. The literature shows the female preponderance in western countries while Asian studies[
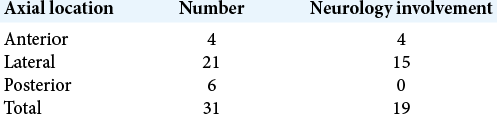
We have assessed the axial/sagittal location of tumors with outcome and complication. Ventrally located upper thoracic spine IDEM tumors were correlated with higher neurological involvement and poorer post-operative outcomes as in our four cases.[
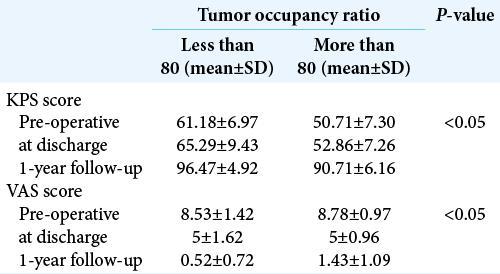
We have also analyzed the tumor occupancy ratio with the disability score and found that once the tumor occupancy increased, the disability also increased. We have divided TOR in two groups; if the TOR was above 80, KPS and VAS scores were poor while those in patients with ratios below 80 demonstrated better outcomes.[
We had done 27 gross total excisions and 4 partial excisions of tumors and found one recurrence case. We have done coagulation and cutting of involved rootlet in nerve sheath tumor and found no functional neurological deficit even in ventrally located tumors except sensory deficits in few cases in the involved region. Approximately 20% of patients in our study had residual focal deficits, none of which were disabling. Notably, two-thirds of patients had excellent postoperative results, a finding corroborated by the literature recovery rates (e.g., 62–88% cases).[
CONCLUSION
Intradural extramedullary tumors are mostly benign, are readily diagnosed on MRI scans, and are typically best managed with gross total surgical excision. Notably, anteriorly located lesions have the greatest pre-operative deficits and highest risk of post-operative residual neurological dysfunction.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahsan MK, Awwal MA, Khan SI, Haque MH, Zaman N. Intradural extramedullary spinal cord tumours: A retrospective study of surgical outcomes. Bangabandhu Sheikh Mujib Med Univ J. 2016. 9: 11-9
2. Chung JY, Lee JJ, Kim HJ, Seo HY. Characterization of magnetic resonance images for spinal cord tumors. Asian Spine J. 2008. 2: 15-21
3. Cohen-Gadol AA, Zikel OM, Koch CA, Scheithauer BW, Krauss WE. Spinal meningiomas in patients younger than 50 years of age: A 21-year experience. J Neurosurg. 2003. 98: 258-63
4. Govind M, Mittal R, Sharma A, Gandhi A. Intradural extramedullary spinal cord tumors: A retrospective study at tertiary referral hospital. Rom Neurosurg. 2016. 30: 106-12
5. Mehta AI, Adogwa O, Karikari IO, Thompson P, Verla T, Null UT. Anatomical location dictating major surgical complications for intradural extramedullary spinal tumors: A 10-year single-institutional experience. J Neurosurg Spine. 2013. 19: 701-7
6. Nizami FA, Mustafa SA, Nazir R, Salaria H, Singh GP, Gadgotra P. Intradural extramedullary spinal cord tumors: Surgical outcome in a newly developed tertiary care hospital. Int J Sci Study. 2017. 5: 48-53
7. Ozawa H, Onoda Y, Aizawa T, Nakamura T, Koakutsu T, Itoi E. Natural history of intradural-extramedullary spinal cord tumors. Acta Neurol Belg. 2012. 112: 265-70
8. Schweitzer JS, Batzdorf U. Ependymoma of the cauda equina region: Diagnosis, treatment, and outcome in 15 patients. Neurosurgery. 1992. 30: 202-7
9. Singh PR, Pandey TK, Ahmad F, Chhabra DK. A prospective observational study of clinical outcome of operated patients of intradural extramedullary spinal cord tumor in our tertiary care center. Rom Neurosurg. 2018. 32: 632-40
10. Song KW, Shin SI, Lee JY, Kim GL, Hyun YS, Park DY. Surgical results of intradural extramedullary tumors. Clin Orthop Surg. 2009. 1: 74-80