- Department of Neurosurgery, Ehime University School of Medicine, Toon, Japan
- Department of Hematology, Clinical Immunology and Infectious Diseases, Ehime University School of Medicine, Toon, Japan
- Division of Diagnostic Pathology, Ehime University Hospital, Toon, Japan.
Correspondence Address:
Akihiro Inoue, Department of Neurosurgery, Ehime University School of Medicine, Toon, Japan.
DOI:10.25259/SNI_1175_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryo Inagaki1, Akihiro Inoue1, Yukihiro Miyazaki2, Kota Kanehisa1, Joji Kunihiro1, Takuya Kondo3, Eiji Katayama3, Mashio Taniwaki3, Seiji Shigekawa1, Hideaki Watanabe1, Riko Kitazawa3, Takeharu Kunieda1. Clinical utility of positron emission tomography leading to rapid and accurate diagnosis of intravascular large B-cell lymphoma presenting with the central nervous system symptoms alone: A case report and review of the literature. 17-Mar-2023;14:89
How to cite this URL: Ryo Inagaki1, Akihiro Inoue1, Yukihiro Miyazaki2, Kota Kanehisa1, Joji Kunihiro1, Takuya Kondo3, Eiji Katayama3, Mashio Taniwaki3, Seiji Shigekawa1, Hideaki Watanabe1, Riko Kitazawa3, Takeharu Kunieda1. Clinical utility of positron emission tomography leading to rapid and accurate diagnosis of intravascular large B-cell lymphoma presenting with the central nervous system symptoms alone: A case report and review of the literature. 17-Mar-2023;14:89. Available from: https://surgicalneurologyint.com/surgicalint-articles/12198/
Abstract
Background: Intravascular large B-cell lymphoma (IVLBCL) is a rare entity among large B-cell non-Hodgkin lymphomas and is often difficult to diagnose. We report the case of a patient with IVLBCL who presented with central nervous system (CNS) symptoms alone, in which positron emission tomography (PET) enabled a rapid and accurate diagnosis.
Case Description: An 81-year-old woman was admitted to our hospital with a 3-month history of gradually progressive dementia and declining spontaneity. Magnetic resonance imaging revealed multiple hyperintense lesions bilaterally on diffusion-weighted imaging without enhancement on gadolinium-enhanced T1-weighted imaging. Laboratory findings showed elevated serum lactate dehydrogenase (626 U/L) and soluble interleukin-2 receptor (sIL-2R) (4692 U/mL). Cerebrospinal fluid (CSF) analysis showed slightly elevated levels of protein (166 mg/dL) and lymphocytic cells (29/μL), and β2-microglobulin (β2-MG) (4.6 mg/L) was highly elevated. Whole-body computed tomography revealed faint ground-glass opacities in the upper and middle lung fields and diffuse enlargement of both kidneys without lymph node swelling. 18F-fluorodeoxyglucose (FDG)-PET showed diffuse and remarkably high FDG uptake in both upper lungs and kidneys without uptake by lymph nodes, suggesting a malignant hematological disease. IVLBCL was confirmed histologically by incisional random skin biopsy from the abdomen. Chemotherapy using R-CHOP regimen in combination with intrathecal methotrexate injection was started on day 5 after admission and follow-up neuroimaging showed no signs of recurrence.
Conclusion: IVLBCL presenting with CNS symptoms alone is rare and often has a poor prognosis associated with delayed diagnosis, and various evaluations (including systemic analysis) are therefore necessary for early diagnosis. FDG-PET, in addition to identification of clinical symptoms and evaluation of serum sIL-2R and CSF β2-MG, enables rapid therapeutic intervention in IVLBCL presenting with CNS symptoms.
Keywords: 18F-fluorodeoxyglucose, Intravascular large B-cell lymphoma, Positron emission tomography, Random skin biopsy, R-CHOP
INTRODUCTION
Intravascular large B-cell lymphoma (IVLBCL) is a rare entity of large B-cell non-Hodgkin lymphoma that is characterized by selective proliferation of large cells within the lumen of small- and medium-sized vessels of various organs.[
CASE DESCRIPTION
An 81-year-old woman presented to our department with a 3-month history of gradually progressive dementia and decline in spontaneity. She had no medical history of atrial fibrillation. Neurological examination on admission revealed disturbance of consciousness but no weakness of the extremities. Her score of 12/30 on the mini-mental state examination (MMSE) indicated severe cognitive impairment. No fever or skin eruptions were present. Neuroimaging on magnetic resonance imaging demonstrated multiple hyperintense lesions bilaterally, including in the periventricular white matter, centrum semiovale, and corpus callosum on diffusion-weighted imaging and fluid attenuated inversion recovery. The lesions showed no enhancement on T1-weighted imaging following administration of gadolinium [
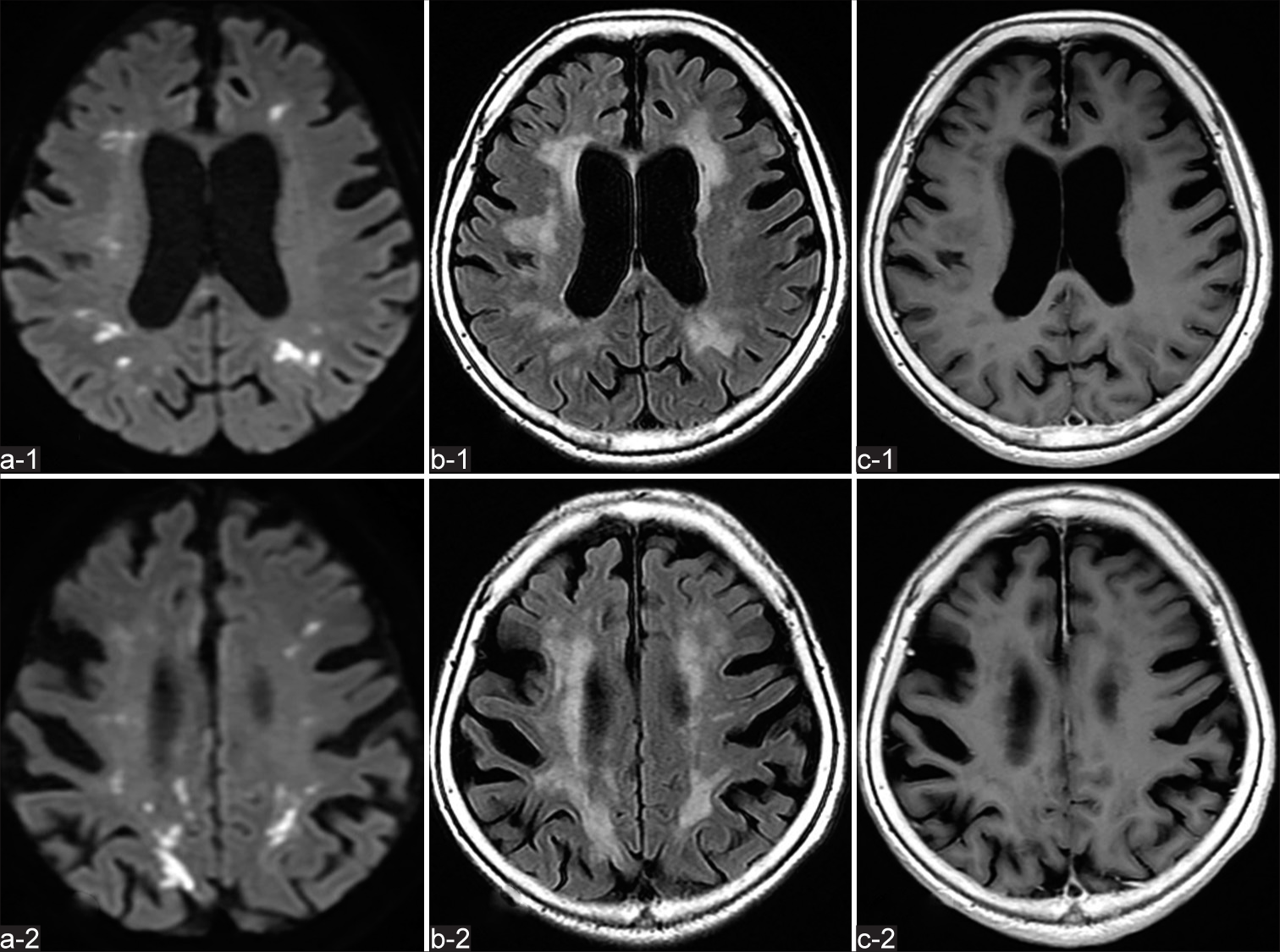
Figure 1:
Magnetic resonance imaging findings of the brain. Axial diffusion-weighted imaging (a-1 - a-2) and fluid-attenuated inversion recovery imaging (b-1 - b-2) obtained at admission reveal multiple hyperintense lesions bilaterally in the periventricular white matter, centrum semiovale, and corpus callosum. T1-weighted imaging (c-1 - c-2) acquired after injection of gadolinium contrast medium shows no enhancement of the lesions.
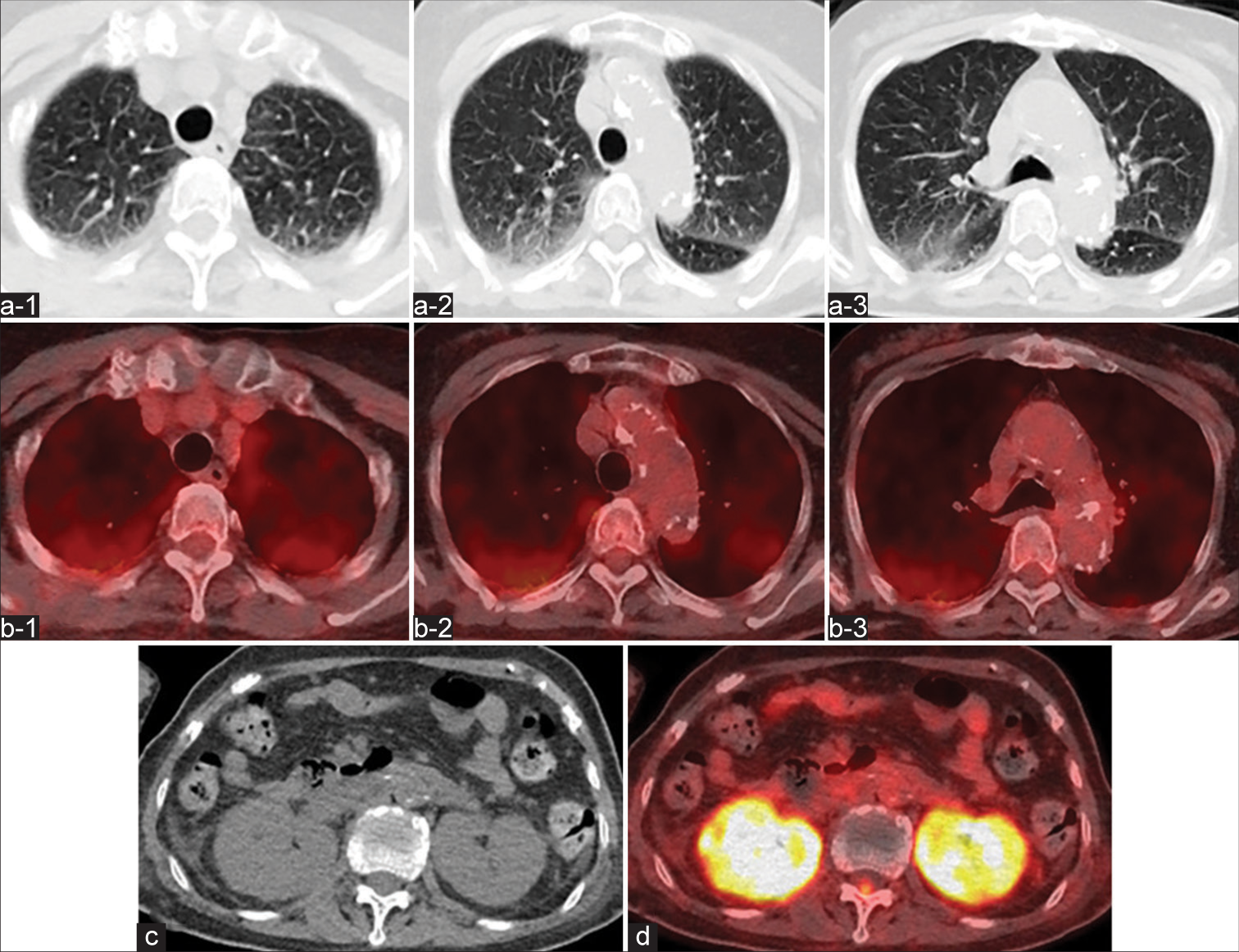
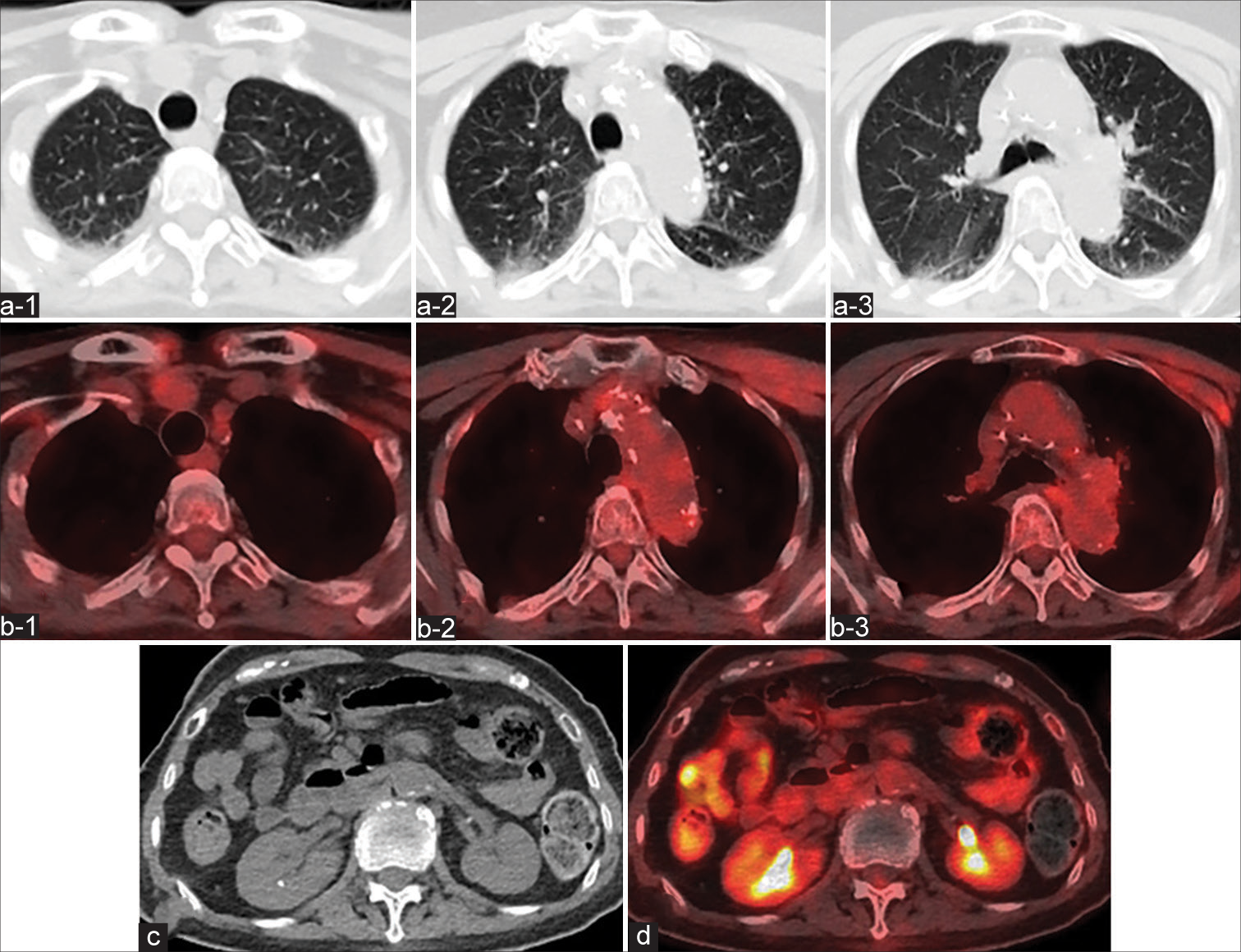
Figure 2:
Axial computed tomography (CT) of the chest (a-1 - a-3) shows faint diffuse ground glass opacities in the upper and middle lung fields bilaterally. 18 F-fluorodeoxyglucose (FDG)-positron emission tomography (PET) (b-1 - b-3) reveals slightly diffuse FDG uptake in the upper and middle lung fields bilaterally without uptake by lymph nodes. CT of the abdomen (c) demonstrates diffuse enlargement of both kidneys without lymph node swelling. FDG-PET (d) shows remarkably high FDG uptake in both kidneys.
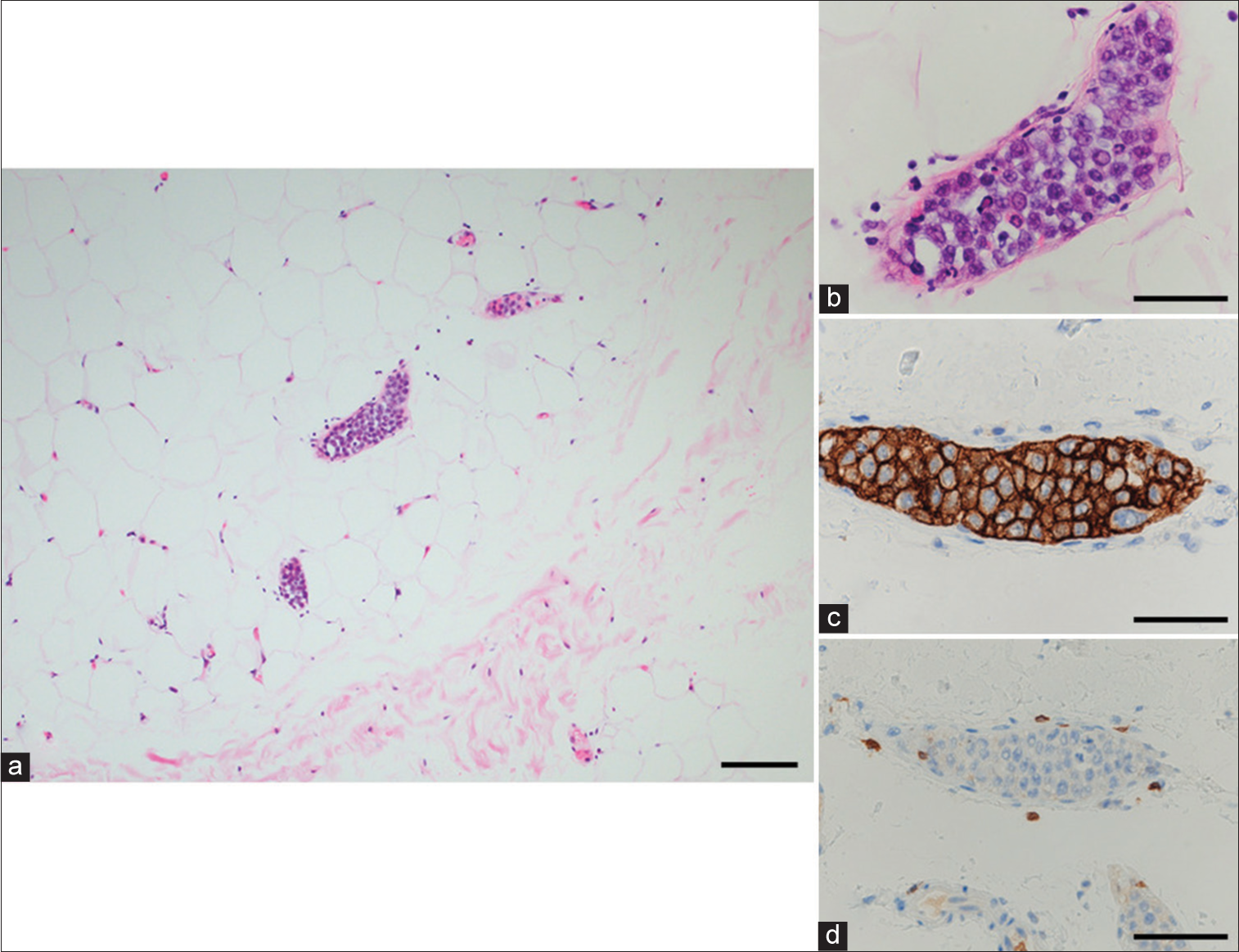
Figure 3:
Histopathology of the resected lesion by random skin biopsy. Pathologic specimen (a and b) shows occlusion of small vessels by neoplastic cells with prominent nucleoli within subcutaneous adipose tissue. Tumor cells show positive staining for CD20 (c) and negative staining for CD3 (d). Magnification: (a) ×200; (b-d) ×400. Scale bars, 100 μm.
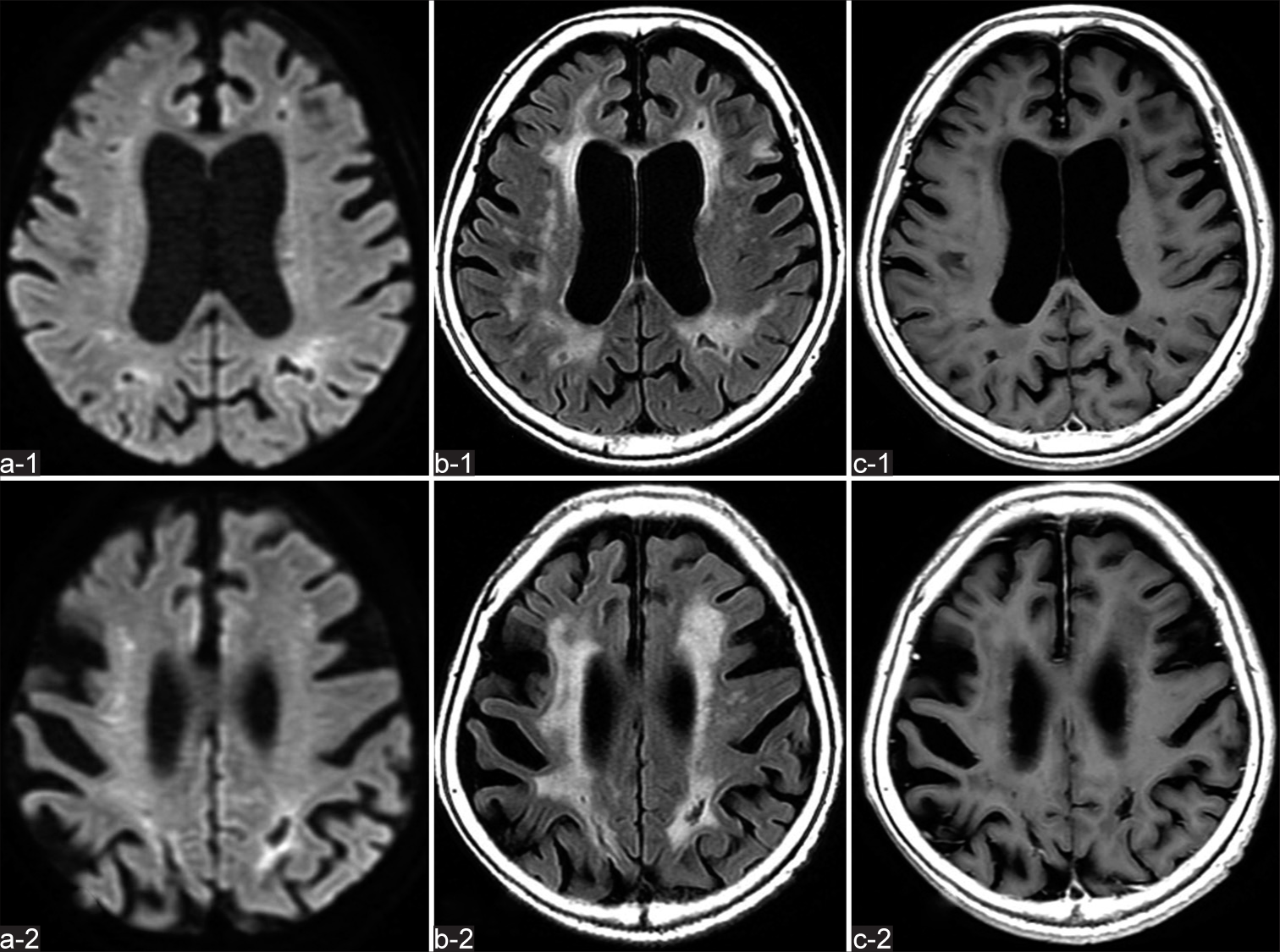
Figure 4:
Brain magnetic resonance imaging (MRI) findings at 1 month after admission. The multiple high-intensity lesions apparent on MRI obtained at admission have decreased on diffusion-weighted imaging (a-1 - a-2), and no new lesions are identified on fluid-attenuated inversion recovery imaging (b-1 - b-2) and gadolinium-enhanced T1-weighted imaging (c-1 - c-2).
Figure 5:
Whole body computed tomography (a-1 - a-3 and c) and 18F-fluorodeoxyglucose (FDG)-positron emission tomography (b-1 - b-3 and d) obtained after three cycles of chemotherapy show complete disappearance of the abnormal signs and FDG accumulation identified on admission, indicating achievement of complete remission.
DISCUSSION
IVLBCL is a rare and fatal subtype of extranodal B cell lymphoma characterized by the selective growth of lymphoma cells, particularly in capillaries, in multiple organs.[
Suspicion of IVLBCL is a crucial first step in the treatment process because IVLBCL has a poor prognosis when therapeutic intervention is delayed. The prognosis of IVLBCL patients will be greatly improved when they obtain a timely and accurate diagnosis and appropriate treatment. Accordingly, further investigations should be performed particularly in the presence of unexplained fever, skin rash, or neurologic manifestations. The laboratory findings of high serum LDH, CRP, and sIL2-R levels, anemia, and thrombocytopenia due to tumor infiltration of the bone marrow and hemophagocytosis are common in IVLBCL. Regarding CSF analysis, a previous study has reported that C-X-C motif chemokine ligand 13, IL-10, sIL-2R, and β2-MG have excellent diagnostic ability for primary CNS lymphoma.[
When IVLBCL is suspected based on the aforementioned symptoms and laboratory findings, pathological confirmation of tumor cells is the gold standard for diagnosis.[
There are several important observations and findings in the present case. First, IVLBCL should be considered in patients who present with rapid progressive dementia and cerebral infarction with elevated serum LDH, CRP and sIL2-R, and CSF β2-MG. Second, because IVLBCL is a systemic disease, FDG-PET may be very useful for obtaining an early and accurate diagnosis, even if only neurologic symptoms are present. Third, because appropriate treatment can improve outcomes, a timely and accurate diagnosis is crucial for patients with IVLBCL. Therefore, early random skin biopsy should be considered if IVLBCL is suspected. Further experience with this therapy and longer patient follow-up is required.
CONCLUSION
As IVLBCL is a very rare entity and often has a poor prognosis, it is necessary to quickly identify the possibility of IVLBCL based on the laboratory findings followed by appropriate biopsy to enable early therapeutic intervention. In the present patient, FDG-PET supported the diagnosis of IVLBCL when clinical suspicion was high. In aged patients with progressive cerebral infarction as well as cognitive decline and recurrent epileptic seizures, it may be important to perform whole-body FDG-PET in addition to analysis of serum sIL-2R and CSF β2-MG, considering the possibility of IVLBCL.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chapin JE, Davis LE, Kornfeld M, Mandler RN. Neurologic manifestations of intravascular lymphomatosis. Acta Neurol Scand. 1995. 91: 494-9
2. Enzan N, Kitadate A, Tanaka A, Matsue K. Incisional random skin biopsy, not punch biopsy, is an appropriate method for diagnosis of intravascular large B-cell lymphoma: A clinicopathological study of 25 patients. Br J Dermatol. 2019. 181: 200-1
3. Glass J, Hochberg FH, Miller DC. Intravascular lymphomatosis. A systemic disease with neurologic manifestations. Cancer. 1993. 71: 3156-64
4. Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004. 103: 275-82
5. Maeyama M, Sasayama T, Tanaka K, Nakamizo S, Tanaka H, Nishihara M. Multi-marker algorithms based on CXCL13, IL-10, sIL-2 receptor, and β2-microglobulin in cerebrospinal fluid to diagnose CNS lymphoma. Cancer Med. 2020. 9: 4114-25
6. Ponzoni M, Ferreri AJ, Campo E, Facchetti F, Mazzucchelli L, Yoshino T. Definition, diagnosis, and management of intravascular large B-cell lymphoma: Proposals and perspectives from an international consensus meeting. J Clin Oncol. 2007. 25: 3168-73
7. Ponzoni M, Campo E, Nakamura S. Intravascular large B-cell lymphoma: A chameleon with multiple faces and many masks. Blood. 2018. 132: 1561-7
8. Porzionato A, Pelletti G, Barzon L, Contran M, Emmi A, Arminio A. Intravascular large B-cell lymphoma affecting multiple cranial nerves: A histopathological study. Neuropathology. 2021. 41: 396-405
9. Shiiba M, Izutsu K, Ishihara M. Early detection of intravascular large B-cell lymphoma by (18) FDG-PET/CT with diffuse FDG uptake in the lung without respiratory symptoms or chest CT abnormalities. Asia Ocean J Nucl Med Biol. 2014. 2: 65-8
10. Shimada K, Kinoshita T, Naoe T, Nakamura S. Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol. 2009. 10: 895-902
11. Tahsili-Fahadan P, Rashidi A, Cimino PJ, Bucelli RC, Keyrouz SG. Neurologic manifestations of intravascular large B-cell lymphoma. Neurol Clin Pract. 2016. 6: 55-60
12. Tobin-Vealey K, Jain S, Al Diffalha S, Sohn A, Henry E, Czerlanis C. Use of fluorodeoxyglucose-positron emission tomography in the diagnosis of intravascular diffuse large B-cell lymphoma. Fed Pract. 2016. 33: 32S-6
13. Tsuji M, Kondo M, Onizawa F, Shishime O, Muramatsu S, Matsuo Y. A case of lung intravascular large B cell lymphoma developed with respiratory failure rescued by corticosteroid prior to definite diagnosis. Respir Med Case Rep. 2022. 37: 101625
14. Wu M, Lin Y, Huang X, Zhang B. Intravascular large B-cell lymphoma presenting as rapidly progressive dementia and stroke: A case report. Medicine (Baltimore). 2021. 100: e27996
15. Zhu D, Shen Y, Huang J, Zhao L. Intravascular large B-cell lymphoma with diffuse ground glass lesion on chest computed tomography diagnosed using transbronchial lung cryobiopsy: A case report. Transl Cancer Res. 2021. 10: 4571-6