- Department of Neurosurgery, Pt. B. D. Sharma University of Health Sciences, Rohtak, Haryana, India
- Department of Radiodiagnosis, Pt. B. D. Sharma University of Health Sciences, Rohtak, Haryana, India
- Department of Anaesthesiology and Critical Care, Pt. B. D. Sharma University of Health Sciences, Rohtak, Haryana, India
Correspondence Address:
Ishwar Singh
Department of Neurosurgery, Pt. B. D. Sharma University of Health Sciences, Rohtak, Haryana, India
DOI:10.4103/sni.sni_392_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ishwar Singh, Seema Rohilla, Prashant Kumar, Gopal Krishana. Combined microsurgical and endoscopic technique for removal of extensive intracranial epidermoids. 14-Feb-2018;9:36
How to cite this URL: Ishwar Singh, Seema Rohilla, Prashant Kumar, Gopal Krishana. Combined microsurgical and endoscopic technique for removal of extensive intracranial epidermoids. 14-Feb-2018;9:36. Available from: http://surgicalneurologyint.com/surgicalint-articles/combined-microsurgical-and-endoscopic-technique-for-removal-of-extensive-intracranial-epidermoids/
Abstract
Background:Intracranial epidermoid tumors are challenging lesions because they grow along the subarachnoid spaces around delicate neurovascular structures and often extend from one compartment to another. The purpose of this study was to determine the usefulness of endoscopic assistance in the microsurgical resection of these lesions, in which total resection is therapy of choice.
Methods:A total of 48 cases of intracranial epidermoids were treated by combined microscopic and endoscopic techniques. Initially, the tumor was removed under the microscope and after ensuring maximum excision, the endoscope was used to find out and excise any residual tumor.
Results:Out of these 48 cases complete excision was achieved in 44 cases and subtotal excision in four patients. Postoperative complications were seen in 17 patients, but none of the complications was attributed to the use of endoscope. Overall use of endoscope benefited 79% of cases.
Conclusion:We recommend combined microsurgical and endoscopic approach to achieve complete/maximum resection of extensive intracranial epidermoid tumors.
Keywords: Epidermoid, microsurgery, neuroendoscopy, skull base
INTRODUCTION
Epidermoid tumors are fairly common and comprise approximately 0.2–1% of all intracranial tumors.[
MATERIAL AND METHODS
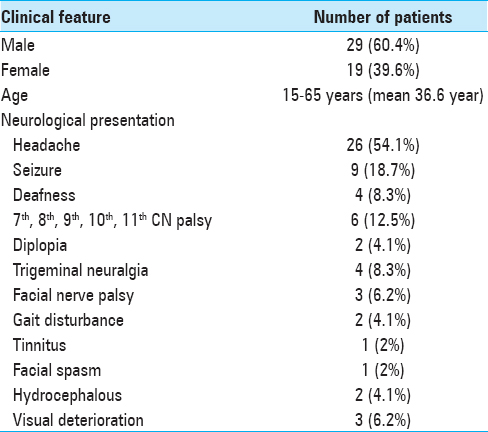
This is a prospective study done at the Post Graduate Institute of Medical Sciences, Rohtak, India and included 48 consecutive patients with intracranial epidermoids who underwent surgical resection of the tumor using combined microscopic and endoscopic techniques between January, 2010 and June, 2017. The clinical characteristics of these patients are mentioned in
Surgical procedure
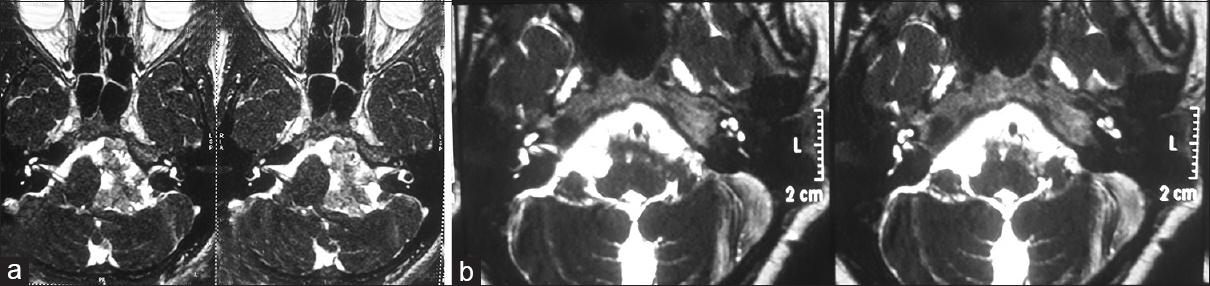
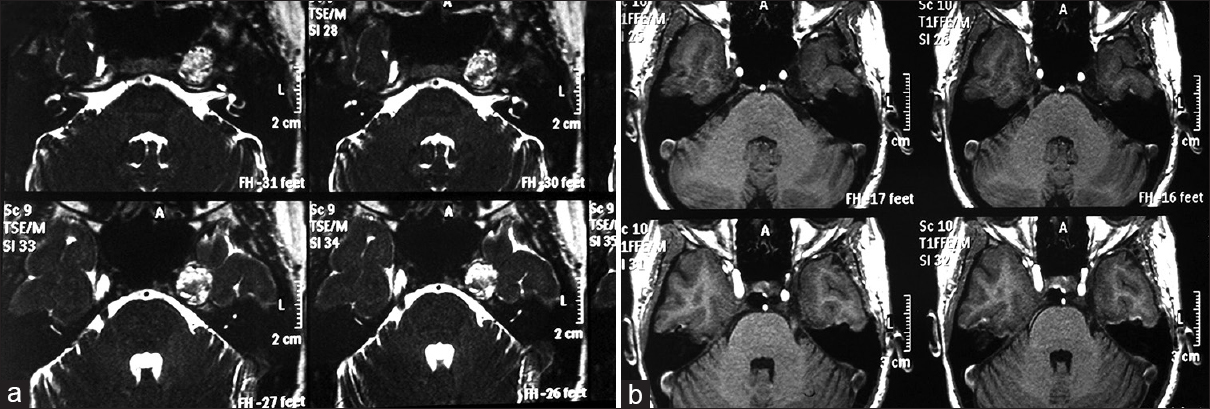
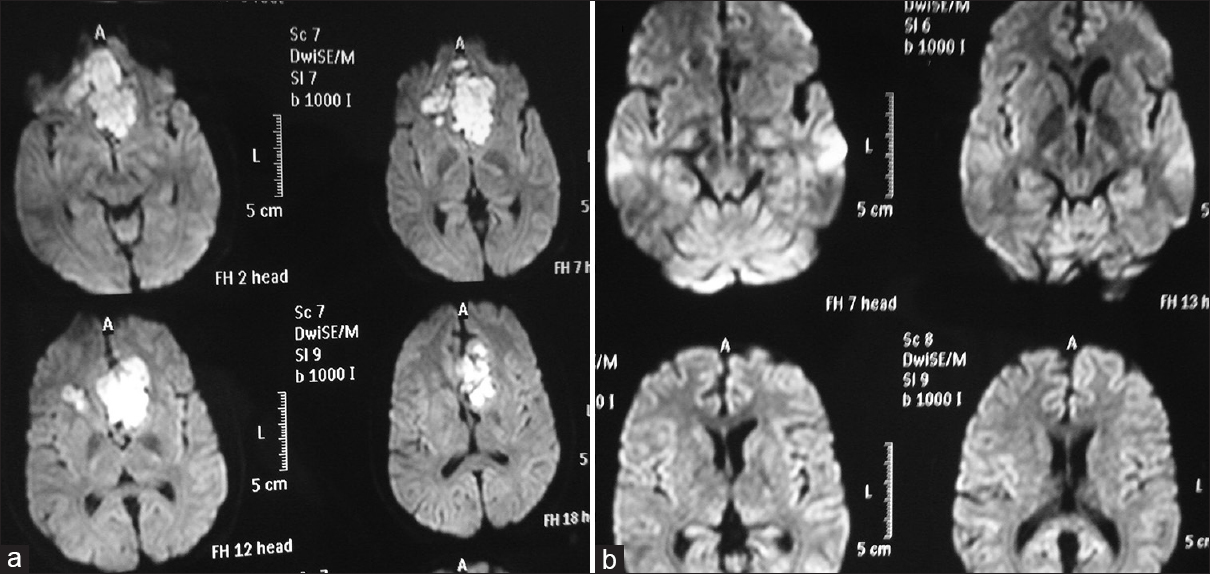
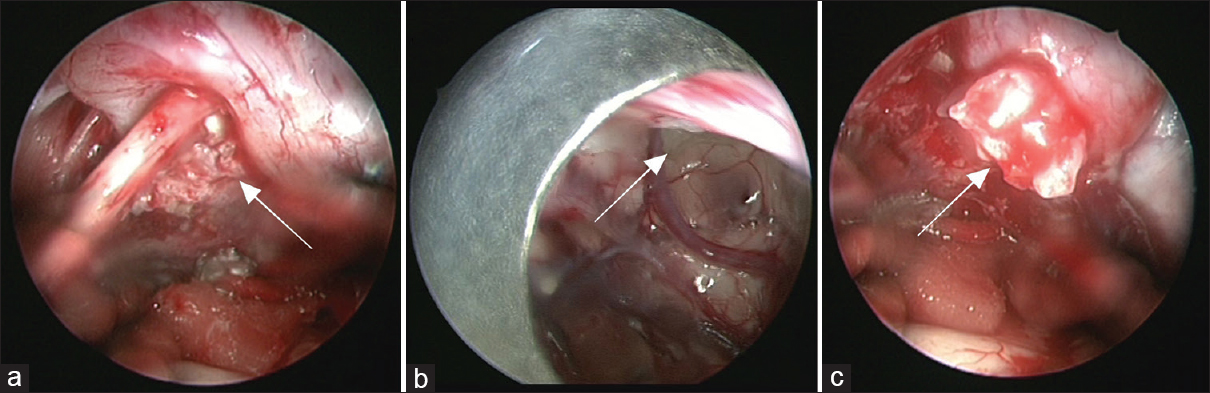
Surgical approach was decided based on tumor location; retromastoid approach for CPA tumors, subfrontal for parasellar tumors, midline transvermian for fourth ventricular lesions, parasagittal interhemispheric for interhemispheric, and anterior petrosal approach for Meckel's cave tumors. Patient of quadrigeminal cistern was operated in sitting position via supracerebellar infratentorial (SCIT) approach. Just before start of operation, each patient received a bolus dose of 8 mg dexamethasone and then 4 mg 6 hourly in postoperative period, gradually tapered over next 4 days. Craniotomy was performed in the standard fashion and the tumor was microscopically exposed. After developing a plane between the overlying arachnoid and the shiny white tumor capsule, the capsule was incised and most of the tumor was removed in a piecemeal fashion with the aid of an operating microscope. An attempt was made to resect the tumor completely by microscope. After no visible tumor was seen under microscope, endoscopic inspection was done with the rigid rod-lens endoscope (outer diameter 4 mm) (Karl Storz GmbH & Co. Tuttlingen, Germany). On endoscopic inspection if no residual tumor was seen, we considered the case as not benefited by endoscopy. If residual tumor was seen and it was possible to further remove the tumor, we considered the case as benefited by endoscopy and tried to remove small bits of tumor using the endoscope. However, if large residual tumor was seen or the tumor was adherent to critical neurovascular structures, we reintroduced the microscope and tried to remove the tumor. Repeated endoscopic inspection was done in such cases to ensure complete excision. Endoscope was used in free hand manner and tumor was removed with conventional microsurgical instruments advanced and manipulated alongside the endoscope but was guided by video images provided by the endoscope (endoscopic controlled microsurgery). 0°, 30°, 45°, and 70° straight endoscopes were used which we are using for pituitary surgery. Intermittent irrigation was done with normal saline to avoid thermal injury. After ensuring complete excision, the subarachnoid space was copiously irrigated with normal saline to remove any epidermoid remnants and to prevent aseptic meningitis. After watertight closure of dura, the bone flap was replaced and wound closed in layers. We attempted to remove whole tumor using operating microscope and endoscope. Nevertheless, where it was firmly adherent to neurovascular structures, a small part of the capsule was left behind to avoid any postoperative neurological deficit. These cases were included in the subtotal resection group even though the postoperative MRI showed no residual tumor. We defined total resection as complete removal of the tumor capsule during surgery and nonvisualization of residual tumor in the postoperative MRI. The patients were followed regularly for a period ranging from 3 months to 72 months (mean 40.06 months). The histopathological examination revealed epidermoid in all cases.
RESULTS
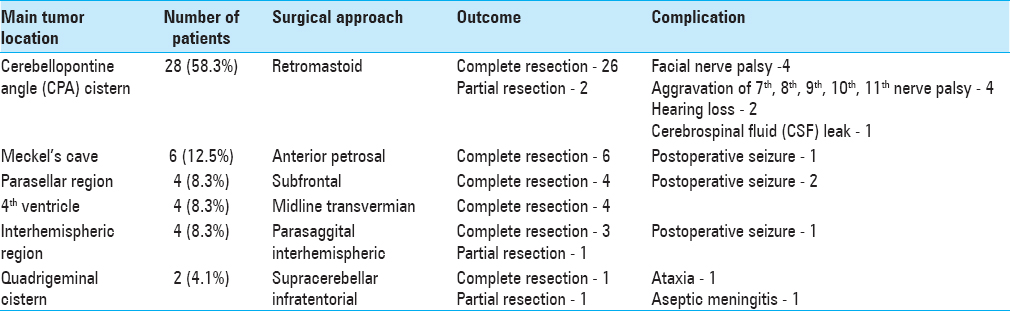
Patient outcome is presented in
DISCUSSION
Epidermoids are congenital neoplasms that grow through desquamation of keratin, cholesterol, and cellular debris.[
Epidermoids frequently spread along the basal cisterns and have considerable extensions along the skull base. The extent of resection is not only influenced by the tumor's adhesion to surrounding structures but also by its pattern of extension.[
The benefits of using endoscope for microsurgical resection of epidermoids have been previously reported.[
However, we have selected the combined microscopic and endoscopic approach because the dissection of capsule from neurovascular structures demands accurate procedure. Moreover, only endoscopic removal in such extensive epidermoids is time consuming and may lead to neurovascular injury due to frequent in and out movement of endoscope. Also, the high fat content of the tumor can disturb clear endoscopic visualization.[
Combined microscopic and endoscopic removal of intracranial epidermoids has also been described previously.[
The rates of radical removal have ranged from 0% to 97%.[
CONCLUSIONS
We conclude that combined microsurgical and endoscopic resection is ideal to achieve maximum resection of epidermoid tumors extending to multiple cranial fossae. The endoscope is a safe and effective adjunct to the microscope in the resection of epidermoid tumors, and facilitates further inspection and resection in most patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adachi K, Inamasu J, Hirose Y, Fujisawa H. Cerebellopontine angle epidermoid cysts: Clinical presentations and surgical outcome. Neurosurg Rev. 2016. 39: 259-66
2. Berger MS, Wilson CB. Epidermoid cysts of the posterior fossa. J Neurosurg. 1985. 62: 214-9
3. Chowdhury FH, Haque MR, Sarker MH. Intracranial epidermoid tumor; microneurosurgical management: An experience of 23 cases. Asian J Neurosurg. 2013. 8: 21-8
4. Chowdhury FH, Haque MR. Endoscopic assisted microsurgical removal of cerebello-pontine angle and prepontine epidermoid. J Neurosci Rural Pract. 2012. 3: 414-9
5. De Divitiis O, Cavallo LM, Fabbro MD, Elefante A, Cappabianca P. Freehand dynamic endoscopic resection of an epidermoid tumor of the cerebellopontine angle. Neurosurgery. 2007. 61: 239-40
6. Ebner FH, Roser F, Thaher F, Schittenhelm J, Tatagiba M. Balancing the shortcomings of microscope and endoscope: Endoscope-assisted technique in microsurgical removal of recurrent epidermoid cysts in the posterior fossa. Minim Invasive Neurosurg. 2010. 53: 218-22
7. Esposito F, Becker DP, Villablanca JP, Kelly DF. Endonasal transsphenoidal transclival removal of prepontine epidermoid tumors: Technical note. Neurosurgery. 2005. 56: 443-
8. Goel A, Muzumdar D, Desai A. Anterior tentorium-based epidermoid tumours: Results of radical surgical treatment in 96 cases. Br J Neurosurg. 2006. 20: 139-45
9. Hamlat A, Hua ZF, Saikali S, Laurent JF, Gedouin D, Ben-Hassel M, Gugan Y. Malignant transformation of intracranial cyst: Systemic article review. J Neurooncol. 2005. 74: 187-95
10. Hu Z, Guan F, Kang T, Huang H, Dai B. Whole Course Neuroendoscopic Resection of Cerebellopontine Angle Epidermoid Cysts. J Neurol Surg A Cent Eur Neurosurg. 2016. 77: 381-8
11. Kato K, Ujiie H, Higa T, Hayashi M, Kubo O, Okada Y. Clinical presentation of intracranial epidermoids: A surgical series of 20 initial and four recurred cases. Asian J Neurosurg. 2010. 5: 32-40
12. Kobata H, Kondo A, Iwasaki K. Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: Pathogenesis and long-term surgical results in 30 patients. Neurosurgery. 2002. 50: 276-85
13. Lakhdar A, Sami A, Naja A, Achouri M, Ouboukhlik A, El Kamar A. Epidermoid cyst of the cerebellopontine angle: A surgical series of 10 cases and review of the literature. Neurochirurgie. 2003. 49: 13-24
14. Long DM, Apuzzo ML.editors. Intracranial epidermoid tumors. Brain Surgery: Complication Avoidance and Management. New York: Churchill Livingstone; 1993. p. 699-88
15. Lynch JC, Aversa A, Pereira C, Nogueira J, Gonçalves M, Lopes H. Surgical strategy for intracranial dermoid and epidermoid tumors: An experience with 33 Patients. Surg Neurol Int. 2014. 5: 163-
16. Mohanty A, Venkatrama SK, Rao BR, Chandramouli BA, Jayakumar PN, Das BS. Experience with cerebellopontine angle epidermoids. Neurosurgery. 1997. 40: 24-9
17. Peng Y, Yu L, Li Y, Fan J, Qiu M, Qi S. Pure endoscopic removal of epidermoid tumors of the cerebellopontine angle. Childs Nerv Syst. 2014. 30: 1261-7
18. Perneczky A, Fries G. Endoscope-assisted brain surgery: Part 1 – evolution, basic concept, and current technique. Neurosurgery. 1998. 42: 219-25
19. Perneczky A, Fries G. Endoscope-assisted brain surgery: Part 2 – Analysis of 380 procedures. Neurosurgery. 1998. 42: 226-32
20. Safavi-Abbasi S, Di Rocco F, Bambakidis N, Talley MC, Gharabaghi A, Luedemann W. Has management of epidermoid tumors of the cerebellopontine angle improved. A surgical synopsis of the past and present?. Skull Base. 2008. 18: 85-98
21. Samii M, Tatagiba M, Piquer J, Carvalho GA. Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg. 1996. 84: 14-9
22. Schroeder HW, Oertel J, Gaab MR. Endoscope-assisted microsurgical resection of epidermoid tumors of the cerebellopontine angle. J Neurosurg. 2004. 101: 227-32
23. Talacchi A, Sala F, Alessandrini F, Turazzi S, Bricolo A. Assessment and surgical management of posterior fossa epidermoid tumors: Report of 28 cases. Neurosurgery. 1998. 42: 242-51
24. Trivelato FP, Giannetti AV. Endoscope-controlled microneurosurgery to treat middle fossa epidermoid cyst. Neurosurgery. 2008. 62: 105-7
25. Tuchman A, Platt A, Winer J, Pham M, Giannotta S, Zada G. Endoscopic-Assisted Resection of Intracranial Epidermoid Tumors. World Neurosurg. 2014. 82: 450-4
26. Uschold T, Abla A, Fusco D, Bristol RE, Nakaji P. Supracerebellar infratentorial endoscopically controlled resection of pineal lesions: Case series and operative technique. J Neurosurg Pediatr. 2011. 8: 554-64
27. Watanabe T, Ito E, Sato T, Ichikawa M, Oda K, Ando H. Combined microsurgical and endoscopic removal of extensive suprasellar and prepontine epidermoid tumors. Neurol Med Chir. 2011. 51: 684-8
28. Yamakawa K, Shitara N, Genka S, Manaka S, Takakura K. Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurgery. 1989. 24: 568-73
29. Yan PX, Yu CJ. Minicraniotomy treatment of an intracerebral epidermoid cyst. Minim Invasive Neurosurg. 2004. 47: 245-8
30. Yasargil MG, Abernathey CD, Sarioglu AC. Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989. 24: 561-7