- Department of Minimal Invasive Neurosurgery, National Centre for Neurosurgery, Astana, Kazakhstan.
- Department of Brain Neurosurgery, National Centre for Neurosurgery, Astana, Kazakhstan.
Correspondence Address:
Iroda Zukhritdinkyzy Mammadinova, Department of Minimal Invasive Neurosurgery, National Centre for Neurosurgery, Astana, Kazakhstan.
DOI:10.25259/SNI_1027_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nurali Nurzhanovich Ashirov1, Iroda Zukhritdinkyzy Mammadinova1, Aidoc Yessimkhanuly Moldabekov2, Dinara Turgunbaevna Berdibayeva2, Daniyar Kerimkulovich Teltayev1, Nurzhan Amirbekovich Ryskeldiyev2, Serik Kuandykovich Akshulakov1,2. Combined supracerebellar infratentorial and right occipital interhemispheric approach to falcotentorial junction meningioma: A case report. 27-Jan-2023;14:26
How to cite this URL: Nurali Nurzhanovich Ashirov1, Iroda Zukhritdinkyzy Mammadinova1, Aidoc Yessimkhanuly Moldabekov2, Dinara Turgunbaevna Berdibayeva2, Daniyar Kerimkulovich Teltayev1, Nurzhan Amirbekovich Ryskeldiyev2, Serik Kuandykovich Akshulakov1,2. Combined supracerebellar infratentorial and right occipital interhemispheric approach to falcotentorial junction meningioma: A case report. 27-Jan-2023;14:26. Available from: https://surgicalneurologyint.com/surgicalint-articles/12130/
Abstract
Background: Falcotentorial meningioma is a rare tumor of pineal region, arising from the dural folds where the tentorium and falx meet. Due to the deep location and near closeness to significant neurovascular structures, gross-total tumor resection in this area can be complicated. Pineal meningiomas can be resected using a variety of approaches; however, all these approaches are associated with a significant risk of postoperative complications.
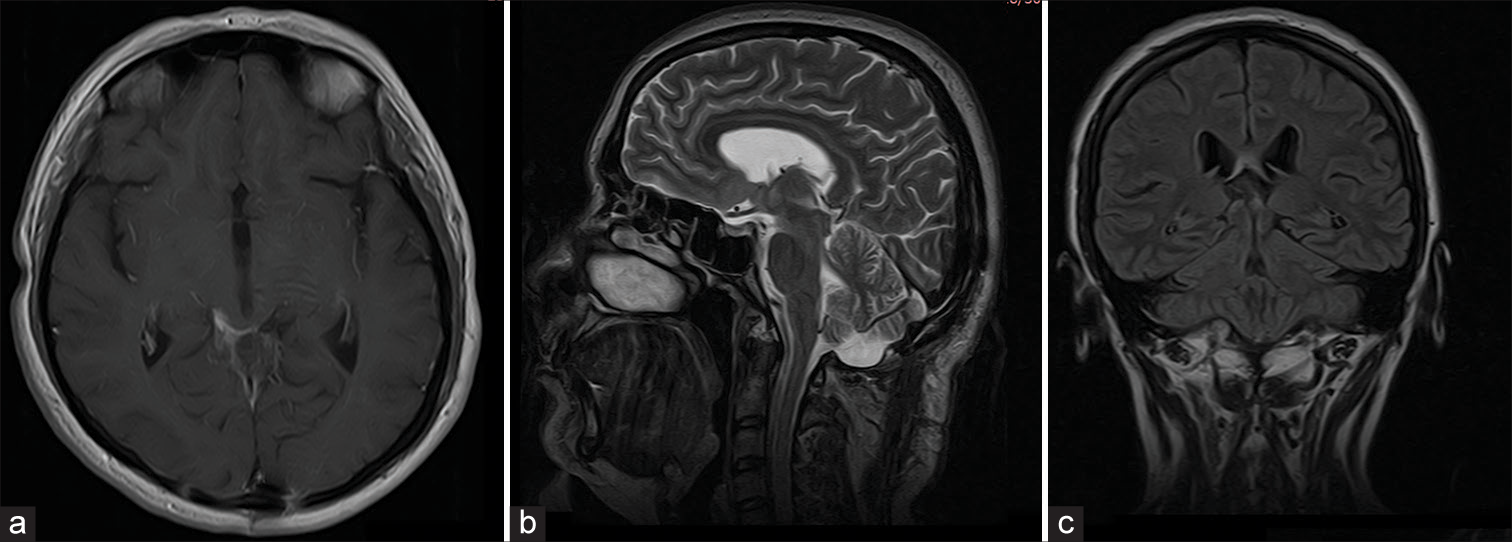
Case Description: A 50-year-old female patient who presented with several headaches and visual field defect and diagnosed with pineal region tumor is discussed in the case report. Patient was successfully managed surgically by combined supracerebellar infratentorial and right occipital interhemispheric approach. Cerebrospinal fluid circulation was restored after surgery and neurological defects were regressed.
Conclusion: Our case shows that it is possible to completely remove giant falcotentorial meningiomas with minimal brain retraction, preserve the straight sinus and vein of Galen, and prevent neurological impairments by combining two approaches.
Keywords: Case report, Combined approach, Falcotentorial meningioma, Occipital interhemispheric approach, Pineal region, Supracerebellar infratentorial approach
INTRODUCTION
The pineal region is an unusual location for meningiomas, accounting for 3–8% of tumors in this region.[
CASE PRESENTATION
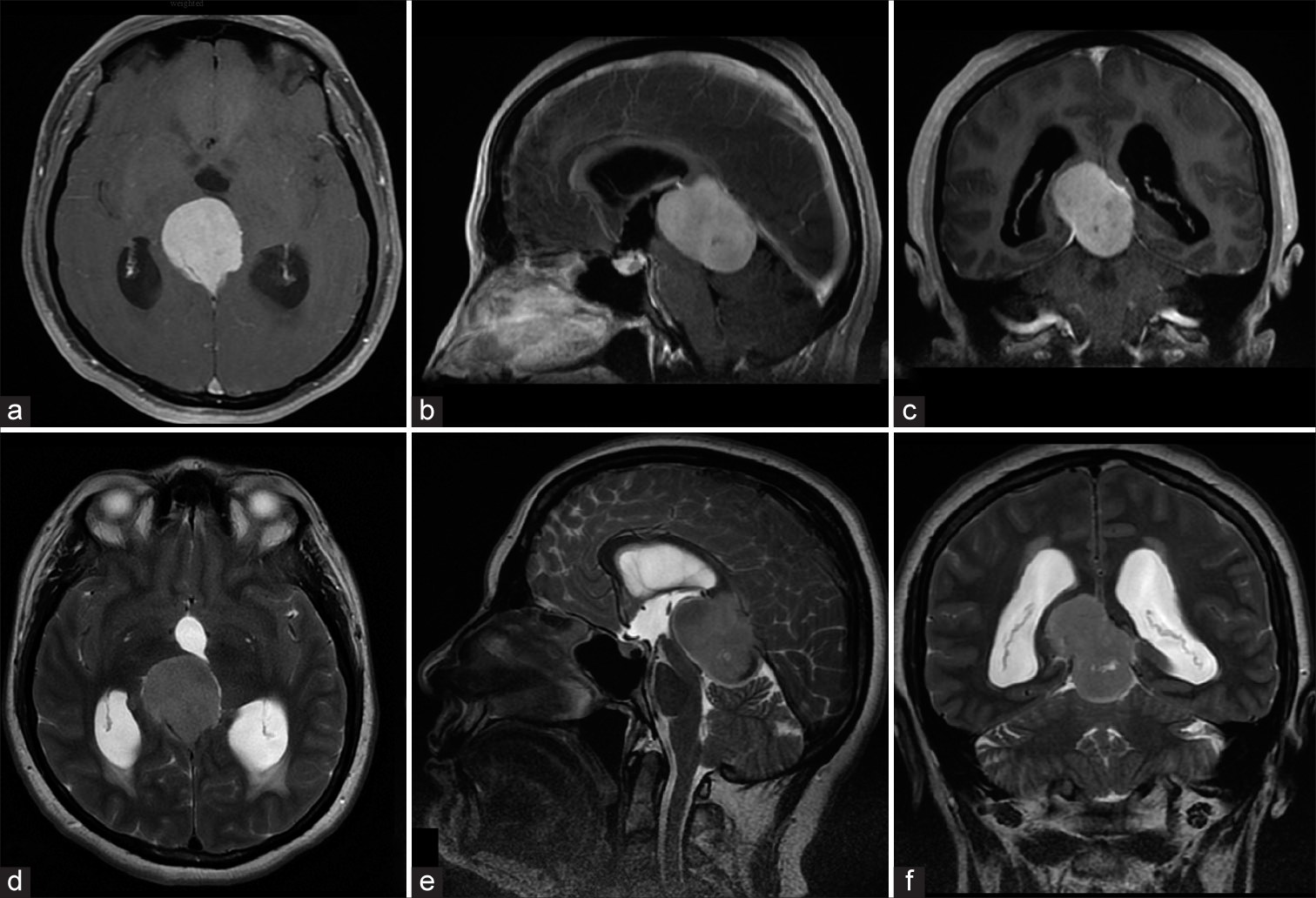
A 50-year-old right-handed woman presented with a 4-month history of headaches, a progressive decrease in vision, a gait disorder, and sleep disturbances. Neurological examination revealed cerebellar ataxia; eye examination showed papilledema and right inferior quadrantanopia. Contrast brain MRI showed a large smooth, oval, well circumscribed mass (43 × 36 × 35 mm) in the pineal region, mass effect, and ventricular enlargement [
Figure 1:
Brain magnetic resonance imaging (MRI). Preoperative axial (a), sagittal (b), and frontal (c) contrast T1-weighted image and axial (d), sagittal (e), and frontal (f) T2-weighted images demonstrates a large (43 × 36 × 35 mm) and homogenously enhancing tumor in the pineal region, occluding the aqueduct, and results in the hydrocephalus.
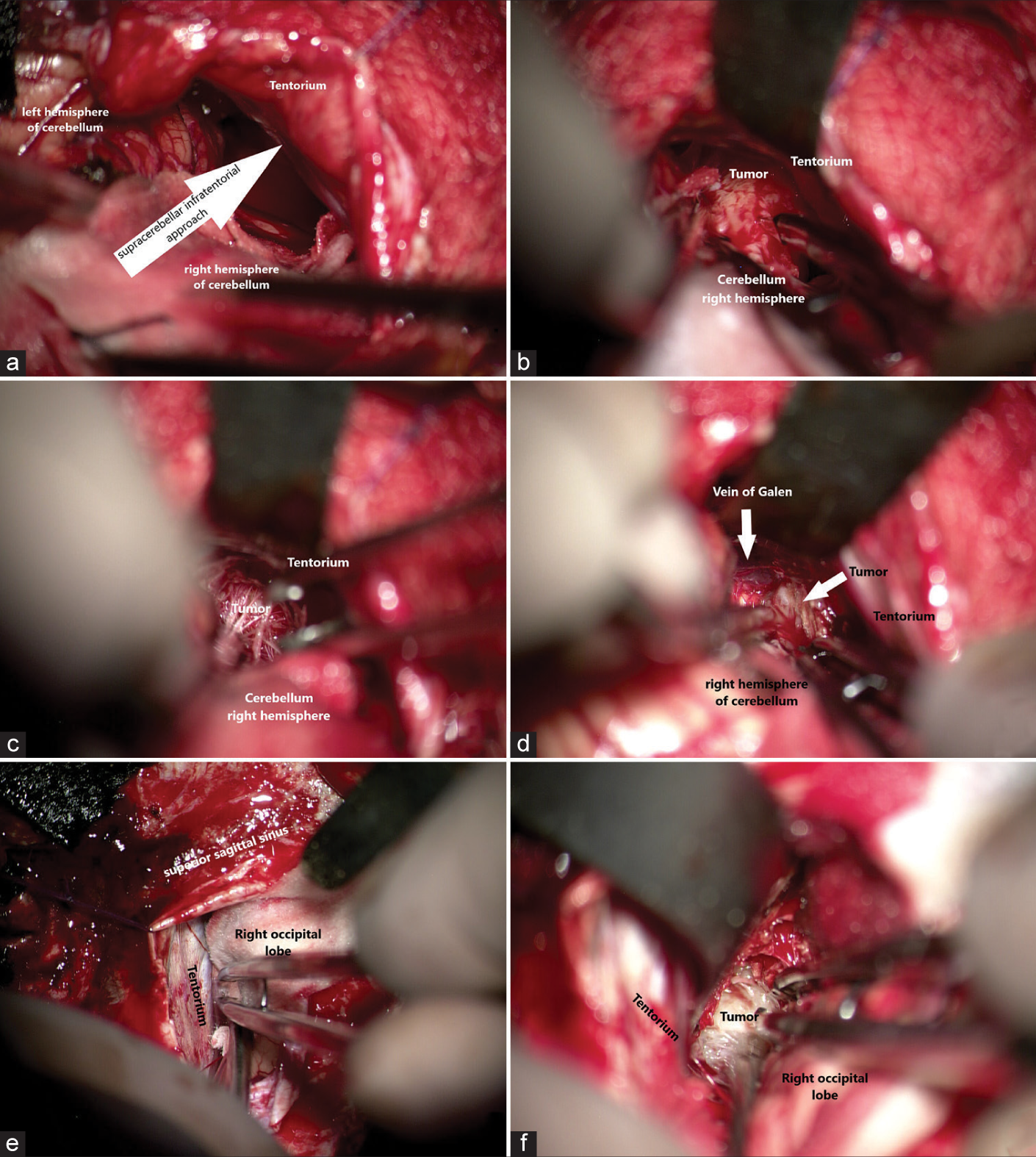
Resection of the lesion was performed through an occipital craniotomy in combination with a suboccipital craniotomy. The patient was in the three-quarter prone position with the neck flexed and the torso elevated about 30° [
Figure 3:
Intraoperative view. (a) Surgical corridor via supracerebellar infratentorial approach. (b and c) The pineal region tumor visualization. (d) Identifying the Vein of Galen. (e) Surgical corridor via right occipital interhemispheric approach. (f) visualization of the superior part of the tumor. (OPMI PENTERO 900 ×6).
Figure 4:
A histological specimen from the tumor resection demonstrates transitional meningioma, WHO Grade 1, ICD-O code 9537/0. Hematoxylin and eosin (×200). A pathological examination was carried out using an Axioskop 40 microscope by Carl Zeiss (Germany) and a panoramic MIDI scanning microscope, with a total magnification of ×200. The hematoxylin and eosin stained slides demonstrated meningothelial cells with bundles of elongated cells that form collagen and reticulin fibers. The nuclei are oval, round, spindle-shaped, and monomorphic.
DISCUSSION
The pineal region is located in the posterior part of the incisural space, consists of the pineal body within the quadrigeminal arachnoidal cistern, and is bordered by vital structures including the third ventricle, mesencephalic tectum, thalamus, corpus callosum, and vein of Galen.[
Treatment options for falcotentorial meningioma include supracerebellar infratentorial, occipital interhemispheric, occipital transtentorial, anterior interhemispheric transsplenial, or a combination of supra and infratentorial transsinus, midline occipital, and suboccipital approaches.[
Asari et al. classified the four types of falcotentorial meningiomas as anterior, inferior, posterior, and superior based on the direction of tumor extension.[
The supratentorial and infratentorial regions are both exposed by the occipital transtentorial/transfalcine approach and its modifications.[
For a superiorly located falcotentorial meningioma, endoscopic-assisted microsurgical excision could be performed using the posterior interhemispheric retrocallosal transfalcine approach. The combination bioccipital suboccipital transsinus transtentorial technique, which involves dividing the less dominant transverse sinus, was described by Liu and Cohen.[
In general, all these approaches are associated with a significant risk of postoperative complications (29%). A safe approach for giant and complicated falcotentorial meningiomas seems to be a combination of approaches. For patients with falcotentorial meningiomas, the choice of approach should be personalized to control tumor growth while preventing approach-related complications.[
Here, we present a case of successfully removing giant falcotentorial meningiomas using a combined supracerebellar infratentorial and interhemispheric occipital approach. Due to the blind spot, we think that a single supracerebellar infratentorial approach is inadequate for anterior type Assari meningiomas with galenic veins displaced contralaterally (Bassiouni Type III). While complete removal without tentorium resection is not achievable with an occipital interhemispheric approach. For this reason, in our case of a large falcotentorial meningioma, we decided to combine these two methods to minimize occipital lobe retraction and achieve maximally safe tumor resection. We preferred the three-quarter prone position because it is associated with low the risk of air embolism and pneumocephalus during the prolonged operation. In our case, a significant proportion of the tumor was found to be infratentorial, and the supracerebellar infratentorial approach was used first to aim to debulk the tumor and improve the visualization of the vein of Galen. Following that, a right occipital interhemispheric approach was used to remove the supratentorial residual tumor. While the supratentorial portion of the tumor can be completely resected by an occipital interhemispheric approach, the great cerebral vein is visible clearly from the supracerebellar infratentorial corridor.
CONCLUSION
Our case demonstrates that by combining two techniques, it is possible to totally remove large falcotentorial meningiomas without external ventricular drainage placement, and with minimal brain retraction, preserve the straight sinus and vein of Galen, and avoid neurological deficits.
Authors’ contributions
All authors contributed to the design and implementation of the article, to the analysis of the results and to the writing of the manuscript.
Ethics approval and consent to participate
The principles of the Declaration of Helsinki were followed in the article.
Availability of data and material
Data openly available in a public repository that issues datasets with DOIs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We are thankful to the patient for his cooperation and allowing us to use his medical records in our case report.
References
1. Asari S, Maeshiro T, Tomita S, Kawauchi M, Yabuno N, Kinugasa K. Meningiomas arising from the falcotentorial junction. Clinical features, neuroimaging studies, and surgical treatment. J Neurosurg. 1995. 82: 726-38
2. Bassiouni H, Asgari S, König HJ, Stolke D. Meningiomas of the falcotentorial junction: Selection of the surgical approach according to the tumor type. Surg Neurol. 2008. 69: 339-49
3. de Andoain GB, Delgado-Fernández J, Cuesta JR, GilSimoes R, Frade-Porto N, Sánchez MP. Meningiomas originated at the falcotentorial region: Analysis of topographic and diagnostic features guiding an optimal surgical planning. World Neurosurg. 2019. 123: e723-33
4. Celtikci E, Nunez M, Liu JK, Gardner PA, Cohen-Gadol AA, Fernandez-Miranda JC. Interhemispheric precuneus retrosplenial transfalcine approach for falcotentorial meningiomas: Anatomic study and clinical series. Operative Neurosurg (Hagerstown). 2021. 21: 48-56
5. Ore CL, Magill ST, McDermott MW. Falcotentorial meningiomas. Handb Clin Neurol. 2020. 170: 107-14
6. Ding Y, Sun L, Hu Y, Zhai W, Zhang L, Yu Z. Combined microscopic and endoscopic surgery for pineal region meningiomas using the occipital-parietal transtentorial approach. Front Oncol. 2022. 12: 828361
7. Gendle C, Karthigeyan M, Salunke P. Pineal region meningioma in a very young child. Pediatr Neurosurg. 2021. 56: 73-8
8. Hong CK, Hong JB, Park H, Moon JH, Chang JH, Lee KS. Surgical treatment for falcotentorial meningiomas. Yonsei Med J. 2016. 57: 1022-8
9. Karas PJ, Gopakumar S, Lazaro TT, Lee S, Khan AB, Hadley CC. 3-Dimensional modeling in virtual reality for resection of a pineal region falcotentorial meningioma. World Neurosurg. 2022. 161: 110
10. Liu JK, Cohen MA. Endoscopic-assisted posterior interhemispheric retrocallosal transfalcine approach for microsurgical resection of a pineal region falcotentorial meningioma: Operative video and technical nuances. Neurosurg Focus. 2016. 40: 15453
11. Liu P, Wang X, Liu Y, Cai J, Yang Z, Quan K. Surgical management of falcotentorial junction tumors: A case series report. Front Oncol. 2022. 12: 866225
12. Mavridis IN, Pyrgelis ES, Agapiou E, Meliou M. Pineal region tumors: Pathophysiological mechanisms of presenting symptoms. Am J Transl Res. 2021. 13: 5758-66
13. Mendez-Rosito D. The supra/infra transtentorial transfalcine approach for the removal of a falcotentorial meningioma: 2-Dimensional video. Oper Neurosurg (Hagerstown). 2019. 16: E166-7
14. Nowak A, Dziedzic T, Czernicki T, Kunert P, Marchel A. Falcotentorial and velum interpositum meningiomas: Two distinct entities of the pineal region. Neurol Neurochir Pol. 2014. 48: 397-402
15. Okada T, Miyahara K, Tanino S, Suzuki K, Watanabe N, Tanaka Y. Parieto-occipital interhemispheric transfalcine, trans-bitentorial approach for radical resection of falcotentorial meningiomas. J Neurol Surg A Cent Eur Neurosurg. 2020. 81: 355-61
16. Pham C, McAlpine H, Tee JW. Successful resolution of the ophthalmic manifestations of a falcotentorial meningioma through Cerebrospinal fluid diversion. J Clin Neurosci. 2020. 71: 281-3
17. Simon E, Afif A, M’Baye M, Mertens P. Anatomy of the pineal region applied to its surgical approach. Neurochirurgie. 2015. 61: 70-6
18. Talacchi A, Biroli A, Hasanbelliu A, Locatelli F. Surgical management of medial tentorial meningioma: Falcotentorial and torcular. World Neurosurg. 2018. 115: e437-47
19. Zhao X, Belykh E, Przybylowski CJ, Moreira LB, Gandhi S, Meybodi AT. Surgical treatment of falcotentorial meningiomas: A retrospective review of a single-institution experience. J Neurosurg. 2019. 2: 1-12