- Department of Neurosurgery, Jinnah Postgraduate Medical Centre, Karachi, Pakistan.
Correspondence Address:
Farrukh Javeed, Department of Neurosurgery, Jinnah Postgraduate Medical Centre, Karachi, Pakistan.
DOI:10.25259/SNI_73_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sehrish Altaf, Lal Rehman, Farrukh Javeed, Anas Ahmed, Yousra Hatif. Comparison of the accuracy of intraoperative lateral fluoroscopy versus postoperative computed tomography in spinal fusions. 24-Feb-2023;14:71
How to cite this URL: Sehrish Altaf, Lal Rehman, Farrukh Javeed, Anas Ahmed, Yousra Hatif. Comparison of the accuracy of intraoperative lateral fluoroscopy versus postoperative computed tomography in spinal fusions. 24-Feb-2023;14:71. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12167
Abstract
Background: This study compared the accuracy of intraoperative lateral fluoroscopic images versus postoperative computed tomography (CT) 3D studies in the treatment of thoracolumbar spinal fusions.
Methods: In a tertiary care hospital (study duration 6 months), we compared the use of lateral fluoroscopic images with the postoperative CT scans in 64 patients with thoracic or lumbar fractures undergoing spinal fusions.
Results: Out of the 64 patients, 61% were lumbar followed by 39% thoracic fractures. In the lumbar spine, the accuracy of screw placement utilizing lateral fluoroscopy versus postoperative CT 3D was 97.4%, while in thoracic spine, accuracy was reduced to 84.4%. Of the 64 patients, just 4 (6.2%) patients demonstrated lateral pedicle cortex penetration, 1 (1.5%) patient had a medial pedicle cortex breach, while none exhibited anterior vertebral body cortex penetration.
Conclusion: This study documented the efficacy of lateral fluoroscopy in intraoperative thoracic and lumbar spinal fixation as confirmed by postoperative CT 3D studies. These findings support the continued use of fluoroscopy rather than CT intraoperatively to lower the risk of radiation exposure to both patients and surgeons.
Keywords: Computed tomography 3D, Lateral fluoroscopy, Spinal fixations, Transpedicular screws, Traumatic spinal injuries
INTRODUCTION
Traumatic spinal injuries are a common cause of morbidity and mortality in young adults, resulting in a major personal disability. Surgical approaches typically include spinal decompressions and transpedicular screw placement to address thoracic and/or lumbar fractures. Numerous navigation systems have been developed to improve the precision of pedicle screw placement and decrease the risk of neurovascular injury.[
MATERIALS AND METHODS
Study design
This prospective cross-sectional study performed over 6 months, looked at 64 patients with traumatic thoracic or lumbar fractures who underwent pedicle screw fixation utilizing intraoperative lateral fluoroscopy. Postoperatively, the accuracy of pedicle screw placement was evaluated with CT 3D studies.
Clinical data
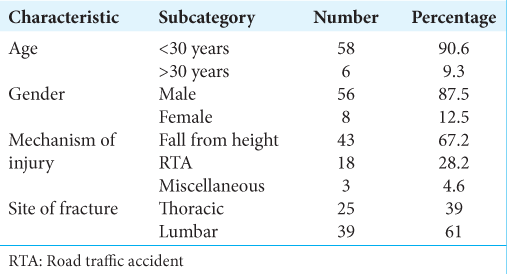
There were 64 patients included in our study; 87.5% were male (n = 56) while 12.5% were female (n = 8), with ages predominantly <30 years (90.6%) [
Radiological evaluation
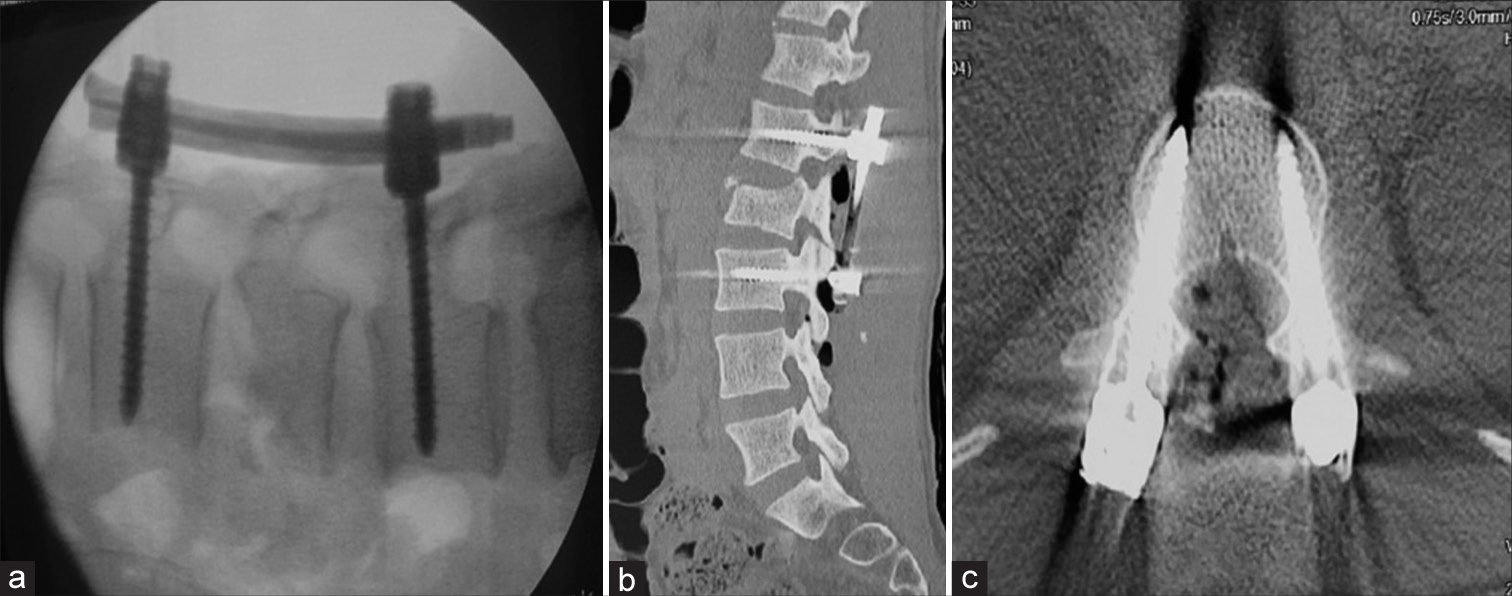
Anteroposterior, lateral radiographs of the spine, computed tomography (CT) 3D scans, and magnetic resonance imaging were done in all patients preoperatively. Intraoperatively, only lateral fluoroscopic guided screw fixation was performed with a C-arm [
Statistical analysis
Statistical analysis was performed using SPSS version 23.
RESULTS
Accuracy of screw placement
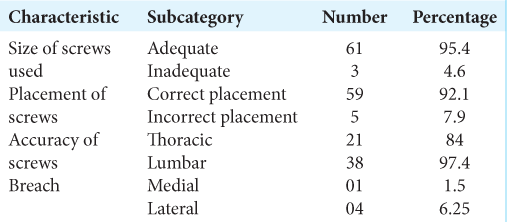
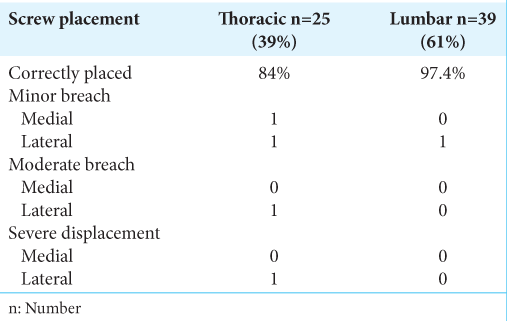
Comparison of lateral fluoroscopic screw placement versus postoperative CT 3D showed that accuracy in lumbar region was 97.4%, while it was 84% in the thoracic region [
CT 3D Documentation of operative pedicle breaches
While evaluating pedicle screw placement according to the classification system described by Gertzbein and Robbins using postoperative CT 3D, 95.5% of patients had adequate screw placement under lateral fluoroscopic guidance, while 4.6% had inadequate screw placement. In the thoracic spine, two of 25 (8%) had minor breaches, one of 25 (4%) had moderate displacement, and one out of 25 (4%) had severe displacement. In lumbar region, 39 (2.5%) had a minor perforation, while there were no moderate or severe screw displacements.
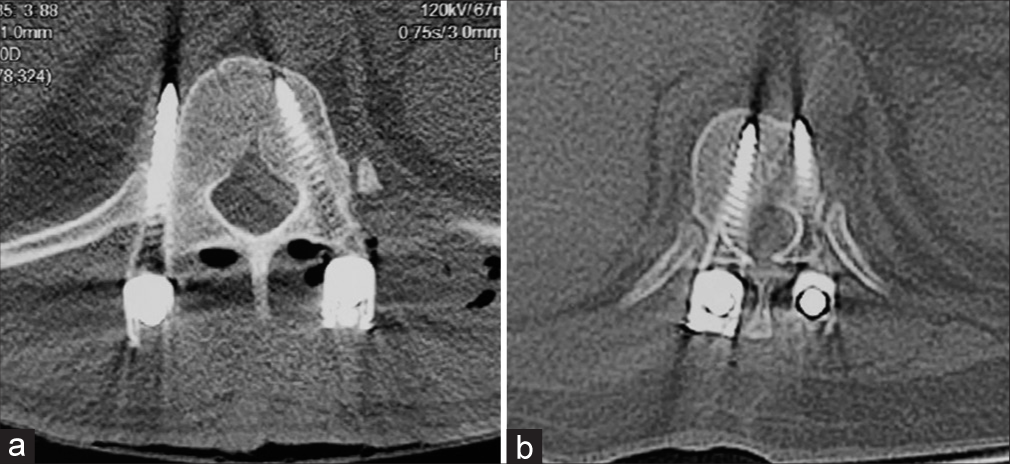
Locations of breaches
The total number of cases with any breach was 5 (7.8%); 1 (1.5%) had a medial wall breach while 4 (6.25%) had lateral wall breaches [
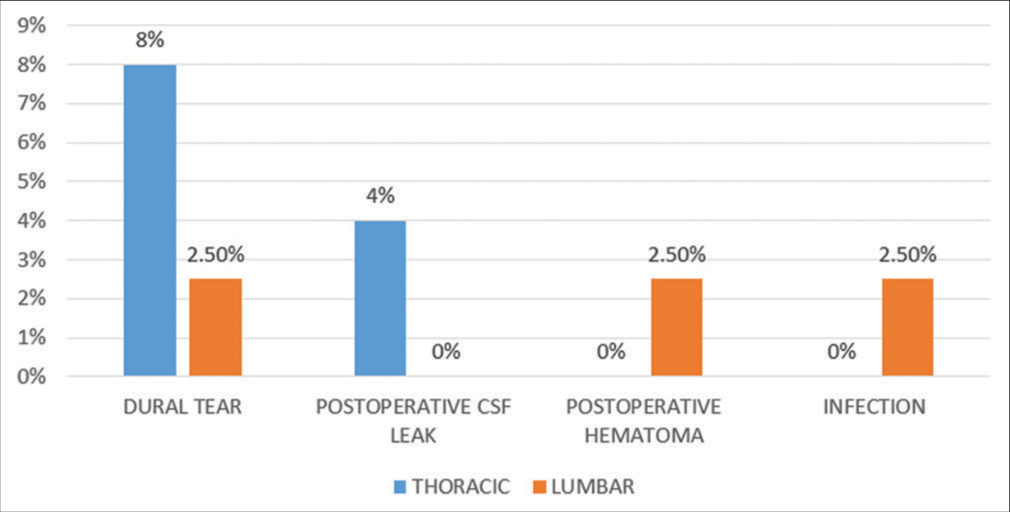
Surgical complications
There were few surgical complications encountered in our studied patients [
DISCUSSION
Our study showed a trend of better accuracy for pedicle screw placement in the lumbar (97.4%) versus thoracic spine (84%). Jing et al., using the Gertzbein-Robbins scale grade, found that 90% of screws in the freehand group and 95.8% of the screws in the navigation group were accurately placed.[
Nevertheless, Jing et al. evaluated the placement of thoracolumbar screws using O-arm-based navigation versus conventional freehand technique and found that in the thoracic spine only 2 (2.3%) of 86 screws in the navigation group versus ten of 87 (11.4%) screws in the freehand group were inaccurately placed.[
Pedicle breaches
We found 6.25% patients had lateral breach, all of them in the thoracic region (12%). Rampersaud et al. reported pedicle breaches in 31.6% (25 out of 79 screws) of all 2D-guided thoracic screw placement with 72% of pedicle breaches being lateral.[
CONCLUSION
For 64 patients with thoracic or lumbar fractures undergoing intraoperative placement of pedicle screws, fluoroscopic guidance proved highly accurate (i.e., lumbar [97.4%] and thoracic [84%]) as corroborated on postoperative CT 3D studies.
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Arnaout MM, ElSheikh MO, Makia MA. Confirmation of accuracy/inaccuracy of lumbar pedicle screw placement using postoperative computed tomography. Surg Neurol Int. 2021. 12: 518
2. Fichtner J, Hofmann N, Rienmüller A, Buchmann N, Gempt J, Kirschke JS. Revision rate of misplaced pedicle screws of the thoracolumbar spine-comparison of three-dimensional fluoroscopy navigation with freehand placement: A systematic analysis and review of the literature. World Neurosurg. 2018. 109: e24-32
3. García-Fantini M, De Casas R. Three-dimensional fluoroscopic navigation versus fluoroscopy-guided placement of pedicle screws in L4-L5-S1 fixation: Single-centre experience of pedicular accuracy and S1 cortical fixation of 810 screws. J Spine Surg. 2018. 4: 736-43
4. Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990. 15: 11-4
5. Jing L, Wang Z, Sun Z, Zhang H, Wang J, Wang G. Accuracy of pedicle screw placement in the thoracic and lumbosacral spines using O-arm-based navigation versus conventional freehand technique. Chin Neurosurg J. 2019. 5: 6
6. Koktekir E, Ceylan D, Tatarli N, Karabagli H, Recber F, Akdemir G. Accuracy of fluoroscopically-assisted pedicle screw placement: Analysis of 1,218 screws in 198 patients. Spine J. 2014. 14: 1702-8
7. Kwan MK, Chiu CK, Chan CY, Zamani R, Hansen-Algenstaedt N. The use of fluoroscopic guided percutaneous pedicle screws in the upper thoracic spine (T1-T6): Is it safe?. J Orthop Surg (Hong Kong). 2017. 25: 2309499017722438
8. Liu H, Wang Y, Pi B, Qian Z, Zhu X, Yang H. Comparison of intraoperative O-arm-and conventional fluoroscopy (C-arm)-assisted insertion of pedicle screws in the treatment of fracture of thoracic vertebrae. J Orthopaedic Surg. 2017. 25: 1-6
9. Rampersaud YR, Simon DA, Foley KT. Accuracy requirements for image-guided spinal pedicle screw placement. Spine (Phila Pa 1976). 2001. 26: 352-9