- Department of Anesthesia, Indian Spinal Injuries Center, New Delhi, India.
- Spine Services, Indian Spinal Injuries Centre, Vasant Kunj, New Delhi, India.
- Department of Anesthesia Seth GS Medical College and KEM Hospital, Mumbai, Seth Gordhandas Sunderdas Medical College, Mumbai, Maharashtra, India.
- Department of Orthopaedics, Seth GS Medical College and KEM Hospital, Mumbai, Seth Gordhandas Sunderdas Medical College, Mumbai, Maharashtra, India.
Correspondence Address:
Rupanwita Sen
Department of Orthopaedics, Seth GS Medical College and KEM Hospital, Mumbai, Seth Gordhandas Sunderdas Medical College, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_638_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rupanwita Sen1, Abhinandan Reddy Mallepally2, Gayatri Sakrikar3, Nandan Marathe2, Tushar Rathod4. Comparison of TruView and King Vision video laryngoscopes in subaxial cervical spine injury: A randomized controlled trial. 06-Nov-2020;11:375
How to cite this URL: Rupanwita Sen1, Abhinandan Reddy Mallepally2, Gayatri Sakrikar3, Nandan Marathe2, Tushar Rathod4. Comparison of TruView and King Vision video laryngoscopes in subaxial cervical spine injury: A randomized controlled trial. 06-Nov-2020;11:375. Available from: https://surgicalneurologyint.com/surgicalint-articles/10374/
Abstract
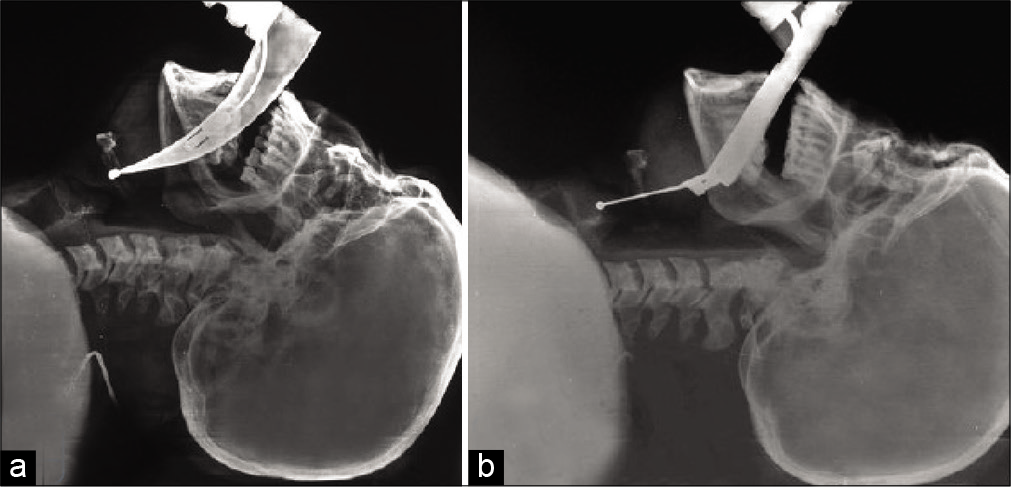
Background: Airway management with cervical spine immobilization poses a particular challenge for intubation in the absence of neck extension and risks neurological damage in cases of unstable cervical spine injuries. Here, with manual inline stabilization (MILS) in patients with cervical spine injuries, we compared the safety/efficacy of intubation utilizing the TruView versus King Vision video laryngoscopes.
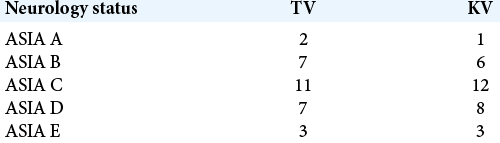
Methods: This prospective, single-blind, comparative study was conducted over a 3-year period. The study population included 60 American Society of Anesthesiologists (ASA) Grade I-III patients, aged 18–65 years, who underwent subaxial cervical spine surgery utilizing two intubation techniques; TruView (TV) versus King Vision (KV). For both groups, relative intubation difficulty scores (IDS), total duration of intubation, hemodynamic changes, and other complications (e.g., soft-tissue injury and neurological deterioration) were recorded.
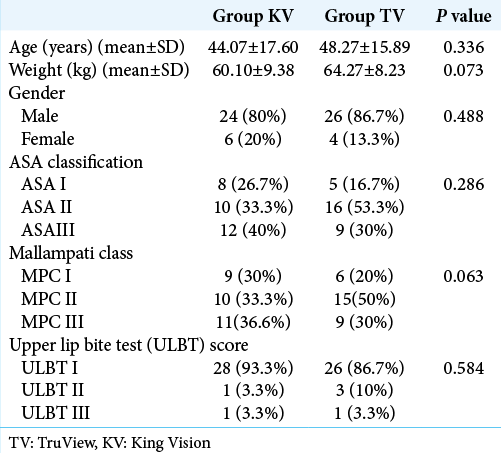
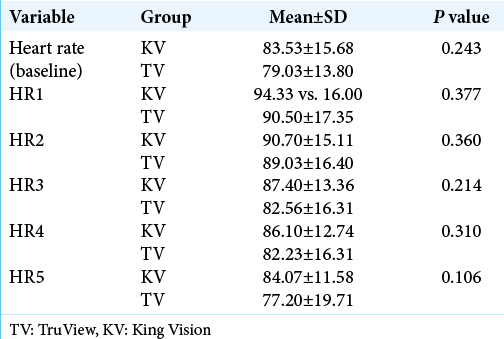
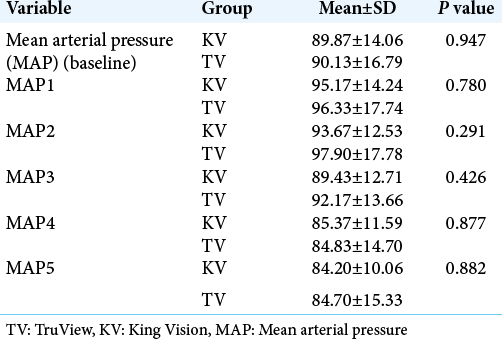
Results: With MILS, patients in the KV group had statistically significant lower IDS (0.70 ± 1.02) and significantly shorter duration of intubation as compared to the TV group (1.67 ± 1.27) with MILS (P = 0.0010); notably, the glottic exposure was similar in both groups. The complication rate (e.g., soft-tissue injury) was lower for the KV group, but this was not statistically significant. Interestingly, no patient from either group exhibited increased neurological deterioration attributable to the method of intubation.
Conclusion: King Vision has several advantages over TruView for intubating patients who have sustained cervical spine trauma. Nevertheless, both laryngoscopes afford comparable glottic views and safety profiles with similar alterations in hemodynamics.
Keywords: Airway management, Cervical spine, Intubation, Video laryngoscope
INTRODUCTION
Manual in-line axial stabilization (MILS) is used for airway management where other stabilization methods are inappropriate.[
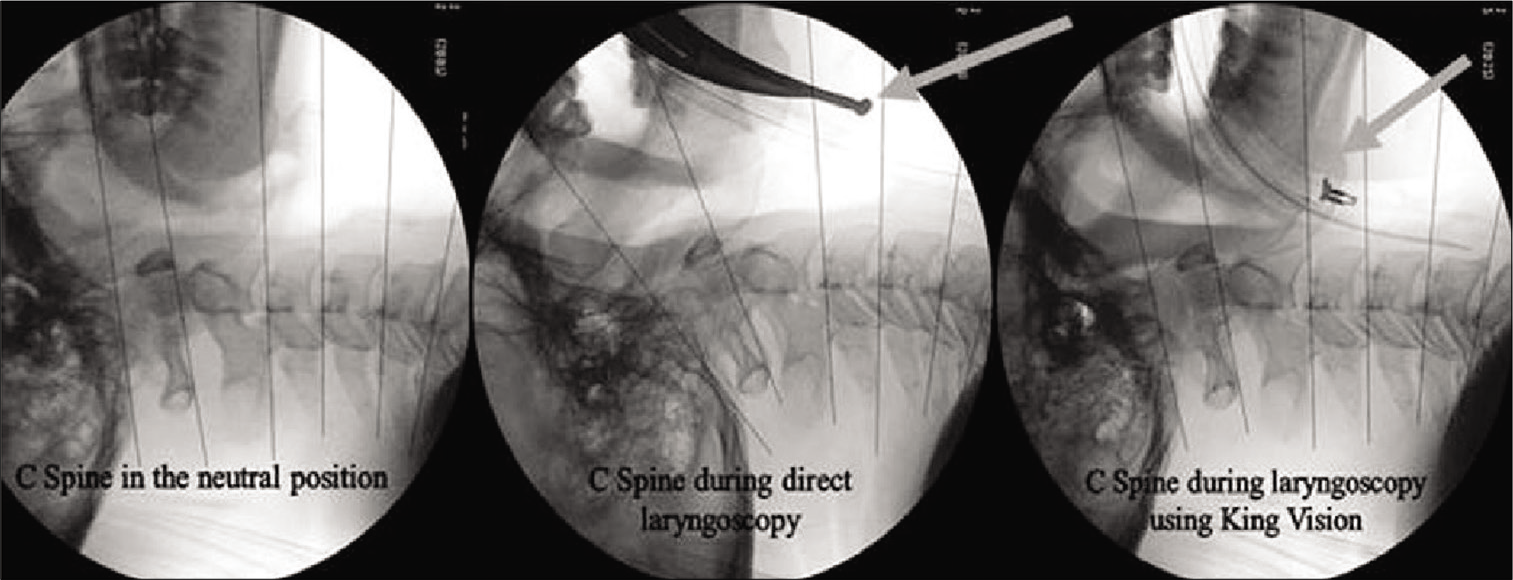
This pilot study compared the safety/efficacy of tracheal intubation utilizing the TV and KV when combined with MILS in patients with subaxial cervical spine trauma [
MATERIALS AND METHODS
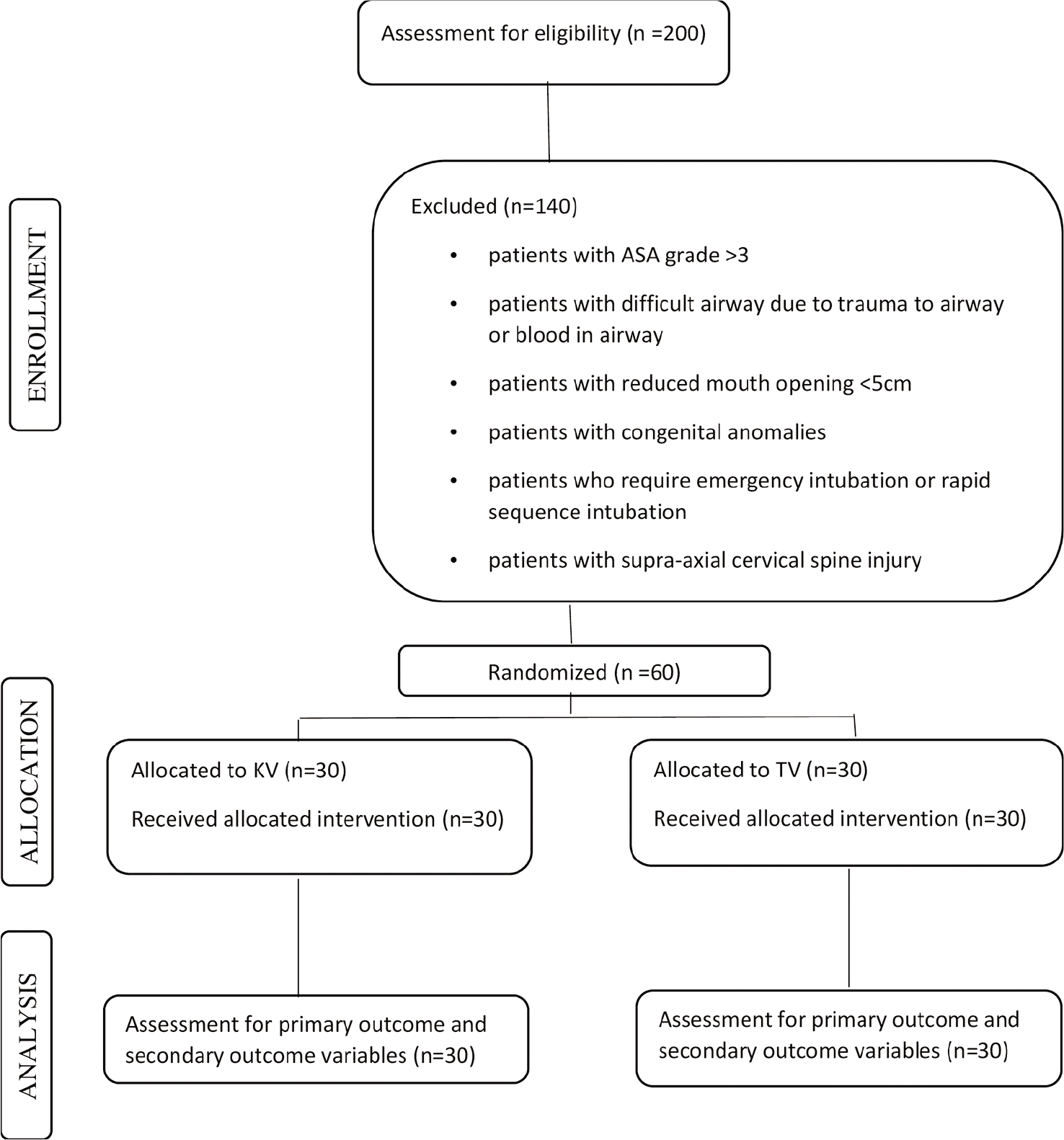
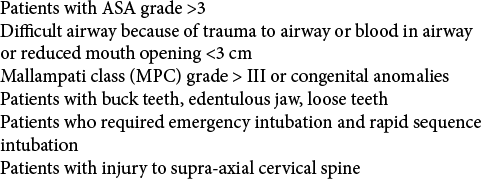
This was an IRB approved, randomized prospective, single-blind, comparative study conducted over a 3-year period (January 2017–December 2019) at tertiary care spinal injuries center [
Anesthetic techniques
Routine induction was performed in both population groups. MILS was applied to hold the mastoid process and side of the neck in position preventing any movement (flexion, extension, or rotation) of the neck. After mask ventilation for 2 min, laryngoscopy and orotracheal intubation were performed by an experienced anesthetist (at least 5 years) utilizing the TV or KV instruments. All intubations were carried out with size 3 blade for both the laryngoscopes. The total duration of intubation was visually confirmed by the anesthetist, and successful tube placement was confirmed utilizing routine modalities (e.g., capnography/end-tidal CO2). Complications during intubation including soft-tissue injuries were recorded.
Statistical analysis
The sample size was measured with the pooled standard deviation of IDS from the past studies as 2.75 and two-sample t-tests were applied using the formula (μ1–μ2)/SD = 0.88. Using the following cutoff values of α as 0.05 and ß as 0.20 (or 80% power), a minimum required sample of 30 in each group was estimated. Quantitative variables (e.g., airway examination, IDS, number of attempts, and complications) were compared using Mann–Whitney test and Chi-square test. Hemodynamic alterations were compared using unpaired and paired t-tests. All results were analyzed using SPSS software version 23.0.
RESULTS
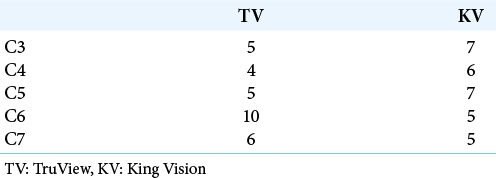
Our study included 60 subjects; 30 in either group, who had sustained subaxial cervical spine injuries resulting in comparable preoperative neurological deficits [
With MILS, patients in the KV group had statistically significant lower IDS (0.70 ± 1.02) and significantly shorter duration of intubation as compared to the TV group (1.67 ± 1.27) with MILS (p = 0.0010) [
DISCUSSION
Managing airway with MILS is very difficult task for an anesthesiologist in patients with cervical spine injuries during resuscitation, administration of general anesthesia, and respiratory support. The TV laryngoscope and KV video laryngoscope are two indirect laryngoscopes each with an advanced optical technology.
Bhardwaj et al.[
The more anatomically fitting design of the KV laryngoscope allowed lessor vertical force to achieve glottic alignment as compared to the TV, which resulted in lesser dental and soft-tissue injury versus TV. Further, the differences of rise in heart rate as well as MAP between the two groups were not statistically significant.
Although both the laryngoscopes provided good glottic view, the KV was slightly better (e.g., ease of insertion with MILS, shorter intubation time, less soft-tissue injury, and reduced hemodynamic changes). The KV further has a provision of disposable blade which removes the concerns of contagious infections.[
CONCLUSION
King Vision has several advantages over TruView for intubating patients who have sustained cervical spine trauma. Nevertheless, both laryngoscopes afford comparable glottic views and safety profiles with similar alterations in hemodynamics.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Ali Q, Amir SH, Ahmed S. A comparative evaluation of king vision video laryngoscope (channelled blade), McCoy, and Macintosh laryngoscopes for tracheal intubation in patients with immobilized cervical spine. Sri Lankan J Anaesthesiol. 2017. 25: 70-5
2. Bhardwaj N, Jain K, Rao M, Mandal AK. Assessment of cervical spine movement during laryngoscopy with Macintosh and truview laryngoscopes. J Anaesthesiol Clin Pharmacol. 2013. 29: 308
3. Bharti N, Arora S, Panda NB. A comparison of McCoy, TruView, and Macintosh laryngoscopes for tracheal intubation in patients with immobilized cervical spine. Saudi J Anaesth. 2014. 8: 188-92
4. Chhabra HS, Bagaraia V, Keny S, Kalidindi KK, Mallepally A, Dhillon MS. COVID-19: Current knowledge and best practices for orthopaedic surgeons. Indian J Orthop. 2020. 54: 1-15
5. El Tahan MR, Al Kenany S, Khidr AM, Al Ghamdi AA, Tawfik AM, Al Mulhim AS. Abstract PR537: Does king vision™ videolaryngoscope reduce cervical spine motion during endotracheal intubation? A crossover study. Anesth Analg. 2016. 123: 682-3
6. Priyanka A, Nag K, Kumar VR, Singh D, Kumar S, Sivashanmugam T. Comparison of king vision and truview laryngoscope for postextubation visualization of vocal cord mobility in patients undergoing thyroid and major neck surgeries: A randomized clinical trial. Anesth Essays Res. 2017. 101: 723-30
7. Rathod T, Garje V, Marathe N, Mohanty S, Shende C, Jogani A. Incidence and outcome analysis of vertebral artery injury in posttraumatic cervical spine. Asian J Neurosurg. 2020. 15: 644