- Department of Pediatric Neurosurgery, McGovern Medical School, University of Texas, Houston and Children’s Memorial Hermann Hospital,
- Department of Neurosurgery, Indiana University,
- Department of Pediatric Neurology, McGovern Medical School at UTHouston and Children’s Memorial Hermann Hospital,
- Department of Neurology, University of Texas Health Science Center at Houston,
- Department of Radiology, McGovern Medical School at UTHouston and Children’s Memorial Hermann Hospital, Houston, Texas, United States.
Correspondence Address:
Ahmed Belal, Department of Pediatric Neurosurgery, McGovern Medical School, University of Texas, Houston and Children’s Memorial Hermann Hospital, Houston, Texas, United States.
DOI:10.25259/SNI_1188_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Belal1,2, Gretchen Von Allmen3, Indira Kommuru3, Jeremy Lankford3, John C. Mosher4, Manish Shah1, Michael Funke3, Michael Watkins3, Rajan Patel5. Complete corpus callosotomy using a frameless navigation probe through a minicraniotomy in children with medically refractory epilepsy: A case series and technical note. 23-Dec-2022;13:585
How to cite this URL: Ahmed Belal1,2, Gretchen Von Allmen3, Indira Kommuru3, Jeremy Lankford3, John C. Mosher4, Manish Shah1, Michael Funke3, Michael Watkins3, Rajan Patel5. Complete corpus callosotomy using a frameless navigation probe through a minicraniotomy in children with medically refractory epilepsy: A case series and technical note. 23-Dec-2022;13:585. Available from: https://surgicalneurologyint.com/surgicalint-articles/12077/
Abstract
Background: Medically refractory epilepsy constitutes up to one-third of the epilepsy pediatric patients. Corpus callosotomy (CC) has been used for the treatment of medically refractory epilepsy in children with atonic seizures and generalized tonic–clonic (GTC) seizures. In this case series study, we are describing a novel technique for CC using the frameless navigation probe through a minicraniotomy.
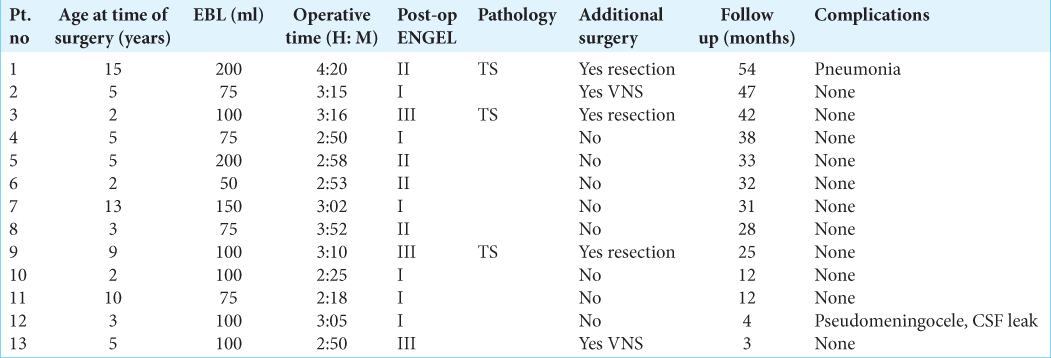
Methods: Thirteen pediatric patients with the diagnosis of medically refractory epilepsy predominantly GTC with drop attack who underwent extensive Phase I. An L-shape was done, then through a 4 × 3 cm craniotomy, we were able to open the interhemispheric fissure until the corpus callosum is visualized. The Stealth probe is then used to go down to the midline raphe which is followed anteriorly then traced posteriorly to the anterior border of the vein of Galen. Finally, the Stealth probe is used to confirm the completeness of the callosotomy.
Results: The procedure was accomplished successfully with no intraoperative complications; mean surgical time is 3 h:07 m. The mean follow-up was 31.5 months. All patients achieved significant seizure control. No patients experienced worsening of their atonic seizures after surgery compared with their preoperative state; however, six patients achieved Engel Class I, four patients achieved Engel Class II, and three patients achieved Engel Class III.
Conclusion: Complete CC using a frameless navigation probe is a novel and effective technique for the treatment of medically refractory epilepsy with a very good surgical and seizure outcomes, minimal neurological morbidity, minimal blood loss, and short OR time.
Keywords: Case series, Corpus callosotomy, Epilepsy, Frameless navigator probe, Navigator
INTRODUCTION
Epilepsy is a neurological disorder affecting about 0.5–1% of the population. Most cases are controlled with medication; however, up to one-third of patients continue to seize despite the best medical management or have debilitating side effects of anticonvulsant medications and may be defined as medically refractory.[
Disconnective procedures such as CC and hemispherotomy are keystones in the surgical treatment of medically refractory epilepsy in children. Children who have nonlocalizing or generalized epilepsy based on seizure semiology, ictal electroencephalography (EEG), and neuroimaging findings are not candidates for resective surgery, and therefore, palliative surgical options should be explored.[
CC is a commonly performed procedure, Dandy operated on a congenital cyst of a cavum septum pellucidum and cavum vergae in a 4.5-year-old boy in 1931 by sectioning the corpus callosum.[
Children who have been reported to respond favorably to CC are those with frequent atonic seizures, also known as “drop attacks,” atypical absence, generalized tonic–clonic (GTC) seizures, and tonic seizures in particular, seizures with generalized inter-ictal and ictal EEG abnormalities with multifocal spike–slow wave activity, as do patients displaying generalized seizures with rapid secondary bisynchronous EEG activity.[
CC has been performed using microsurgery, complete callosotomy is carried through the splenium to the arachnoid of the quadrigeminal cistern, and the vein of Galen may usually be seen through this arachnoid. Spencer et al. showed a 68% seizure control rate after complete callosotomy for tonic–clonic seizures and a 57% seizure control rate for tonic seizures.[
Image-guided frameless stereotaxy has been demonstrated to be an important adjunct in the planning and performing of the procedure. The side of the approach and size of the craniotomy may be determined on the basis of favorability of the bridging veins with respect to the extent of the callosotomy.[
MATERIALS AND METHODS
The committee for the Protection of Human Subjects has approved the conduction of this research study in accordance with its guidelines and with the methods agreed on by the principal investigator and approved by the committee (HSC-MS-17-0092). Consent was not required for the study.
This was a prospective case series study, single-center experience, and nonconsecutive. We present a series of 13 children diagnosed with medically refractory epilepsy who underwent extensive Phase I workup including video EEG, magnetic resonance imaging (MRI), magnetoencephalogram, and positron emission tomography scan before being considered candidates for CC. The patient’s population consisted of 13 children with a mean age of 6.1 years. Seizure disorder was predominantly GTC with drop attacks.
Technique description
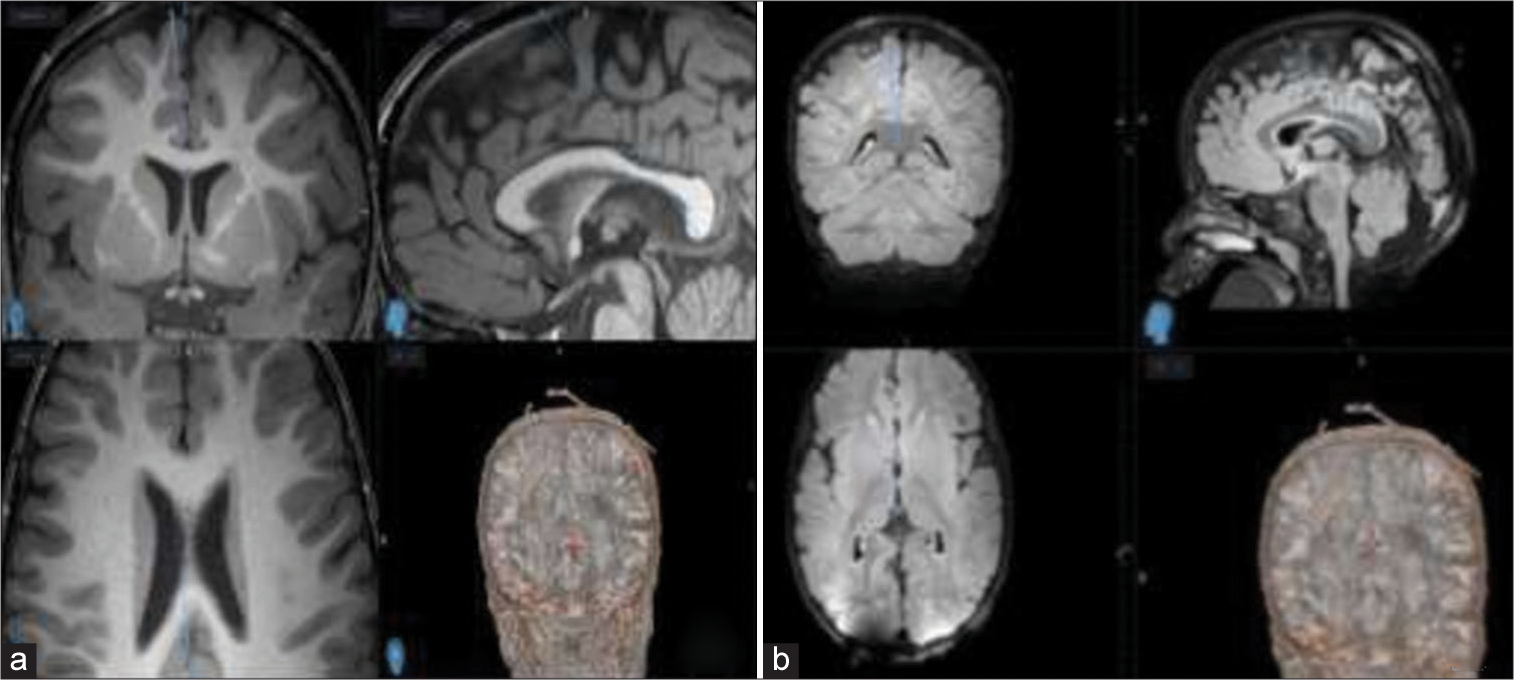
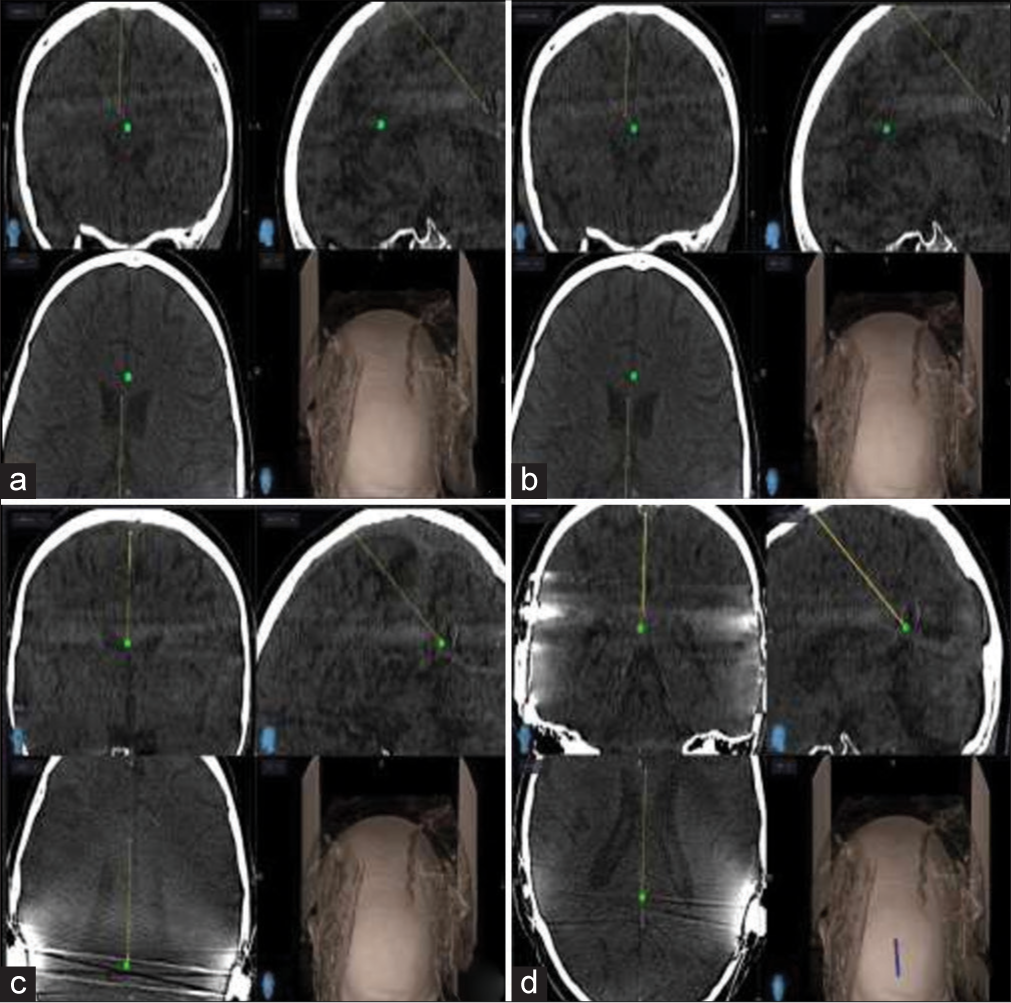
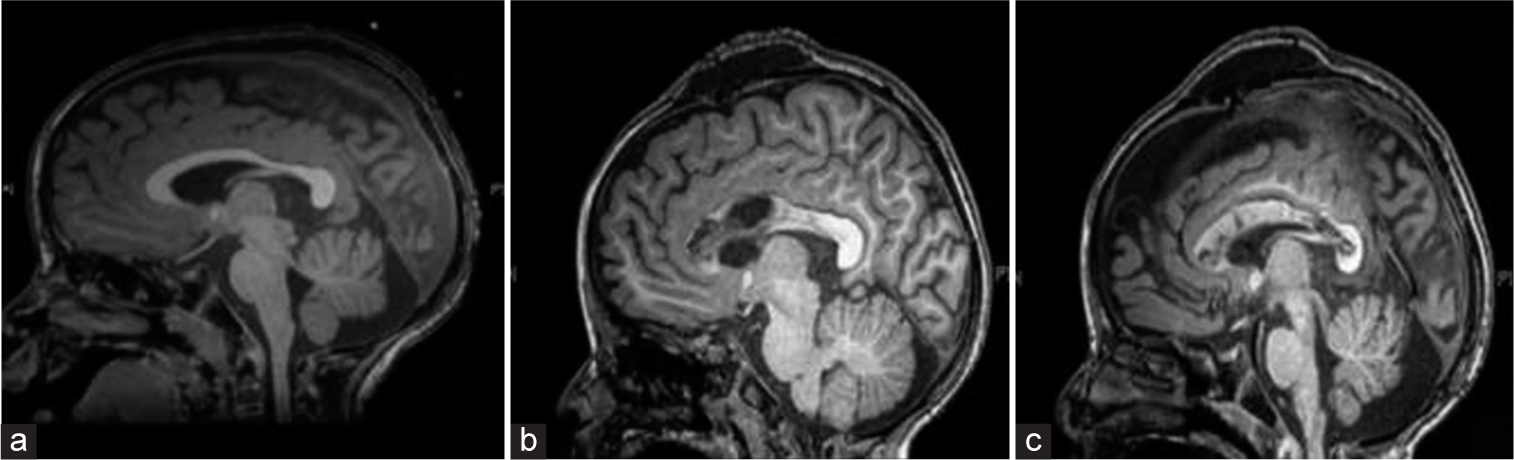
Preoperative MRI is coregistered to the scalp and used for frameless stereotactic navigation [
Position
The patient is positioned supine on the operating table with the head positioned laterally with the right side down, to allow for gravity-assisted retraction of the frontal lobe.
Exposure
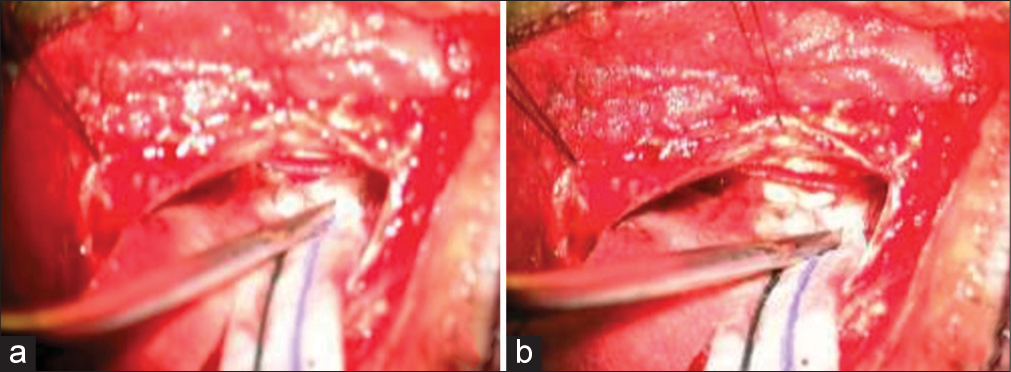
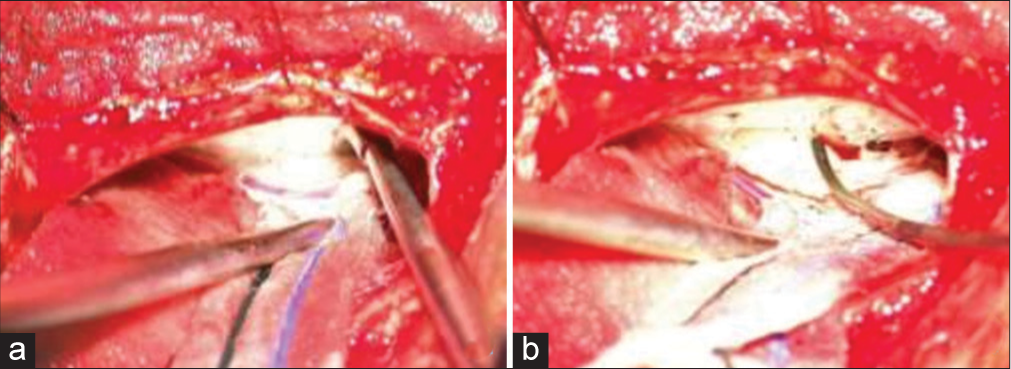
A limited hair shave is performed around the planned incision, then an L-shape incision along the midline and then to the temporal line using the Stealth to get a good window to the anterior two-thirds of the corpus callosum. Once this was done, a myocutaneous flap is reflected anterolaterally. The Stealth navigation is again confirmed to be accurate. A 4 cm anteroposterior by 3 cm lateral craniotomy is made to include the sagittal sinus. The dura is then opened in an U-shaped fashion and reflected toward the superior sagittal sinus, until the interhemispheric fissure is exposed. Care is taken to preserve all cortical veins that are at or posterior to the coronal suture. Using a surgical microscope to open the interhemispheric fissure, the arachnoid is dissected down to the pericallosal arteries [
RESULTS
Patient characteristics and results
Between April 2016 and December 2020, 13 patients with a mean age of 6 years underwent complete CC using a frameless navigation probe at our institution [
DISCUSSION
This study presents our initial experience of 13 patients with completion of CC using the navigator probe through a minicraniotomy in children with medically refractory epilepsy. Overall, completion of CC was performed with a reasonable safety profile and minimal complications. We had one patient developed that pseudomeningocele was managed conservatively with aspiration of the fluid collection followed by head wrapping and prophylactic antibiotics. Another baseline disabled patient developed pneumonia during the hospital admission who recovered after a course of antibiotics. CC is traditionally offered as a palliative therapy for drug-resistant epilepsy aiming to prevent epileptic discharges from spreading between hemispheres and thereby preventing generalization of seizures, particularly drop attacks. Our institution has also found it helpful to lateralize epilepsy for further potentially curative surgery.
Our technical innovation involves using the electromagnetic navigation probe, in which registration accuracy is confirmed again after dissecting down to the midline raphe, allows for a very limited interhemispheric window. Careful study of the venous anatomy helps in meticulous planning of the skin incision, bone flap, and dural opening using the navigation probe to trace the bridging veins, hence minimizing the risk of venous injury and venous infarction. Complications associated with a large open craniotomy and vessel dissection include meningitis, venous or arterial infarctions, subgaleal fluid collection, and hydrocephalus. Hemiparesis and speech delay have also been reported after callosotomy with microsurgical dissection. The reported technique may potentially decrease the risk of large open craniotomy complications.[
Hemispheric edema and supplemental motor area syndromes are avoided by minimizing brain retraction using a minicraniotomy and minimal interhemispheric dissection using the navigation probe to perform the callosotomy using the navigation system. As only a small amount of the midline callosum needs exposure to find the raphe and confirm the Stealth accuracy, using the AXIEM probe critically avoids dissection injury to the bilateral, often adherent cingulate gyri anteriorly and posteriorly in the setting of antiepileptic medications that induce platelet dysfunction, such as valproate and lacosamide. This was especially true for cases 1, 3, and 9 in whom substantial bilateral tuber burden made dissection challenging with nonexistent brain relaxation.
Maintaining the callosotomy to the midline raphe can be easily achieved under navigation, so avoiding lateral deviation and injury to the fornix or corona radiata thus avoiding possible memory disturbance or weakness, respectively. Avoiding violation of the ependyma and accidental entry into the ventricles is a great advantage of using the navigator probe, thus avoiding CSF leak, intraventricular bleed, or hydrocephalus.
Using an endoscope for CC has been described by many surgeons. The main disadvantage is that the ability to dissect is limited by the movement of the instrument only in the axial direction. Furthermore, bleeding may be difficult to control due to limitation of the endoscopic cautery instruments.[
MR-guided laser interstitial thermal therapy (LITT) is a treatment option that was first described by Curry et al. for medically refractory epilepsy in 2012.[
Stereotactic radiosurgery (SRS) for CC was first reported in 1999.[
The efficacy of our technique is comparable to that demonstrated in other published series of completion CC. In an earlier study by Fuiks et al., open completion surgeries resulted in improvement in five out of 10 patients, with response to the initial partial CC being predictive of outcome following completion.[
CONCLUSION
Complete CC using a frameless navigation probe through a minicraniotomy in children with medically refractory epilepsy is an alternative option to open, endoscopic, stereotactic laser, and stereotactic radio surgery for disconnection of the corpus callosum for the treatment of drop attacks in patients with epilepsy. In this study, we report good surgical outcomes (seizure outcome Classes I-III) in 100% of patients with minimal neurological morbidity, minimal blood loss, and short OR time. Future work should include more patients to better evaluate the efficacy of this novel technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bower RS, Wirrell E, Nwojo M, Wetjen NM, Marsh WR, Meyer FB. Seizure outcomes after corpus callosotomy for drop attacks. Neurosurgery. 2013. 73: 993-1000
2. Curry DJ, Gowda A, McNichols RJ, Wilfong AA. MR-guided stereotactic laser ablation of epileptogenic foci in children. Epilepsy Behav. 2012. 24: 408-14
3. Dandy WE. Congenital cerebral cysts of the cavum septi pellucidi (fifth ventricle) and cavum vergae (sixth ventricle): Diagnosis and treatment. Arch Neurol Psychiatry. 1931. 25: 44-66
4. Fuiks KS, Wyler AR, Hermann BP, Somes G. Seizure outcome from anterior and complete corpus callosotomy. J Neurosurg. 1991. 74: 573-8
5. Graham D, Tisdall MM, Gill D. Corpus callosotomy outcomes in pediatric patients: A systematic review. Epilepsia. 2016. 57: 1053-68
6. Hong J, Desai A, Thadani VM, Roberts DW. Efficacy and safety of corpus callosotomy after vagal nerve stimulation in patients with drug-resistant epilepsy. J Neurosurg. 2017. 128: 277-86
7. Jalilian L, Limbrick DD, Steger-May K, Johnston J, Powers AK, Smyth MD. Complete versus anterior two-thirds corpus callosotomy in children: Analysis of outcome. J Neurosurg. 2010. 6: 257-66
8. Jea A, Vachhrajani S, Johnson KK, Rutka JT. Corpus callosotomy in children with intractable epilepsy using frameless stereotactic neuronavigation: 12-year experience at the Hospital for Sick Children in Toronto. Neurosurg Focus. 2008. 25: E7
9. Kasasbeh AS, Smyth MD, Steger-May K, Jalilian L, Bertrand M, Limbrick DD. Outcomes after anterior or complete corpus callosotomy in children. Neurosurgery. 2014. 74: 17-28
10. Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000. 342: 314-9
11. Palma AE, Wicks RT, Popli G, Couture DE. Corpus callosotomy via laser interstitial thermal therapy: A case series. J Neurosurg. 2018. 23: 303-7
12. Pendl G, Eder HG, Schroettner O, Leber KA. Corpus callosotomy with radiosurgery. Neurosurgery. 1999. 45: 303-7 discussion 307-8
13. Pruitt R, Gamble A, Black K, Schulder M, Mehta AD. Complication avoidance in laser interstitial thermal therapy: Lessons learned. J Neurosurg. 2017. 126: 1238-45
14. Rich CW, Fasano RE, Isbaine F, Saindane AM, Qiu D, Curry DJ. MRI-guided stereotactic laser corpus callosotomy for epilepsy: Distinct methods and outcomes. J Neurosurg. 2022. 135: 770-82
15. Roessler K, Hofmann A, Sommer B, Grummich P, Coras R, Kasper BS. Resective surgery for medically refractory epilepsy using intraoperative MRI and functional neuronavigation: The Erlangen experience of 415 patients. Neurosurg Focus. 2016. 40: E15
16. Sood S, Marupudi NI, Asano E, Haridas A, Ham SD. Endoscopic corpus callosotomy and hemispherotomy. J Neurosurg. 2015. 16: 681-6
17. Spencer S, Huh L. Outcomes of epilepsy surgery in adults and children. Lancet Neurol. 2008. 7: 525-37
18. Spencer SS, Spencer DD, Sass K, Westerveld M, Katz A, Mattson R. Anterior, total, and two-stage corpus callosum section: Differential and incremental seizure responses. Epilepsia. 1993. 34: 561-7
19. Valencia Calderón C, Cevallos AC, Valdiviezo AC, Dávila RE, Rosales FP, Alcocer JQ. Neuronavigation in the surgical planning of callosotomy. Neurocirugia (Astur). 2016. 27: 186-93
20. Van Wagenen WP, Herren RY. Surgical division of commissural pathways in the corpus callosum: Relation to spread of an epileptic attack. Arch Neurol Psychiatry. 1940. 44: 740-59
21. Wiebe S, Blume WT, Girvin JP, Eliasziw M. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001. 345: 311-8