- Department of Neurosurgery, Slotervaart Hospital, Louwesweg 6 1066 EC Amsterdam, The Netherlands
- Current Work Address: Department of Neurology, Saint Lucas Andreas Hospital, Jan Tooropstraat 164 1061 AE Amsterdam, The Netherlands
- Department of Neurosurgery, Medical Center Haaglanden, Leyweg 275, 2545 CH The Hague, The Netherlands
- Department of Neurology, Slotervaart Hospital, Louwesweg 6 1066 EC Amsterdam, The Netherlands
- Current Work Address: Department of Neurology, Leiden University Medical Center, Albinusdreef 2, 2333 ZA 2300 RC Leiden, The Netherlands
Correspondence Address:
Nyika D. Kruyt
Department of Neurology, Slotervaart Hospital, Louwesweg 6 1066 EC Amsterdam, The Netherlands
Current Work Address: Department of Neurology, Leiden University Medical Center, Albinusdreef 2, 2333 ZA 2300 RC Leiden, The Netherlands
DOI:10.4103/2152-7806.156544
Copyright: © 2015 Oudeman EA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Oudeman EA, Nandoe Tewarie RD S, G. Joost Jöbsis, Arts MP, Kruyt ND. Complications corner: Anterior thoracic disc surgery with dural tear/CSF fistula and low-pressure pleural drain led to severe intracranial hypotension. Surg Neurol Int 07-May-2015;6:
How to cite this URL: Oudeman EA, Nandoe Tewarie RD S, G. Joost Jöbsis, Arts MP, Kruyt ND. Complications corner: Anterior thoracic disc surgery with dural tear/CSF fistula and low-pressure pleural drain led to severe intracranial hypotension. Surg Neurol Int 07-May-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/complications-corner-anterior-thoracic-disc-surgery-dural/
Abstract
Background:Thoracic disc surgery can lead to a life-threatening complication: intracranial hypotension due to a subarachnoid-pleural fistula.
Case Description:We report a 63-year-old male with paraparesis due to multiple herniated thoracic discs, with compressive myelopathy. The patient required a circumferential procedure including a laminectomy/fusion followed by an anterior thoracic decompression to address both diffuse idiopathic skeletal hyperostosis (DISH) anteriorly and posterior stenosis. The postoperative course was complicated by severe intracranial hypotension attributed to the erroneous placement of a low-pressure drain placed in the pleural cavity instead of a lumbar drain; this resulted in subdural hematoma's necessitating subsequent surgery.
Conclusion:Severe neurological deterioration occurring after thoracic decompressive surgery may rarely be attributed to intracranial hypotension due to a subarachnoid-pleural fistula. Patients should be treated with external lumbar drainage of cerebrospinal fluid for 3–5 days rather than a low-pressure pleural drain to avoid the onset of intracranial hypotension leading to symptomatic subdural hematomas.
Keywords: Cerebrospinal fluid leak, herniated disc, intracranial hypotension, subarachnoid-pleural fistula, spine, surgery
INTRODUCTION
History and examination
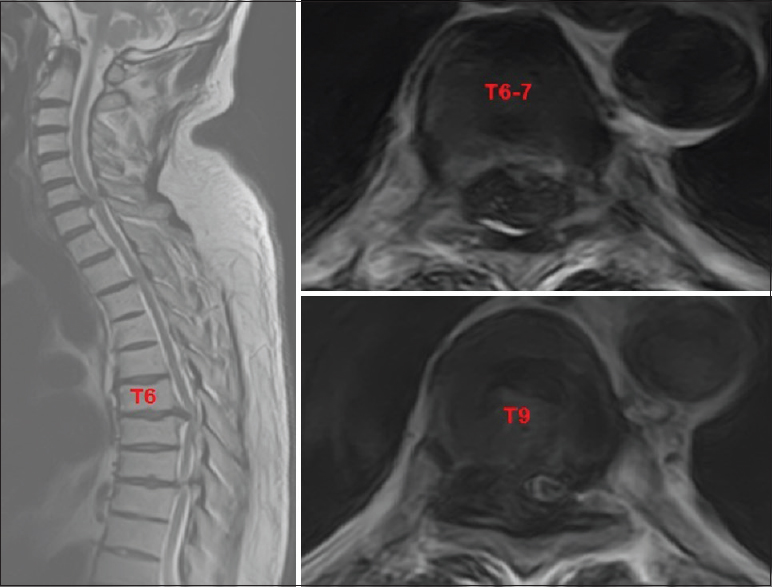
A 63-year-old obese male, presented with a progressive paraparesis. Magnetic resonance imaging (MRI) and computed tomography (CT) studies documented severe T5-T9 diffuse idiopathic skeletal hyperostosis (DISH) resulting in marked circumferential cord compression attributed to multiple anterior ossified disc herniations and posterior ossification of the ligamentum flavum (OYL)/facet arthrosis. The most marked cord compression was seen at the T6-T7 and T8-T9 levels [Figures
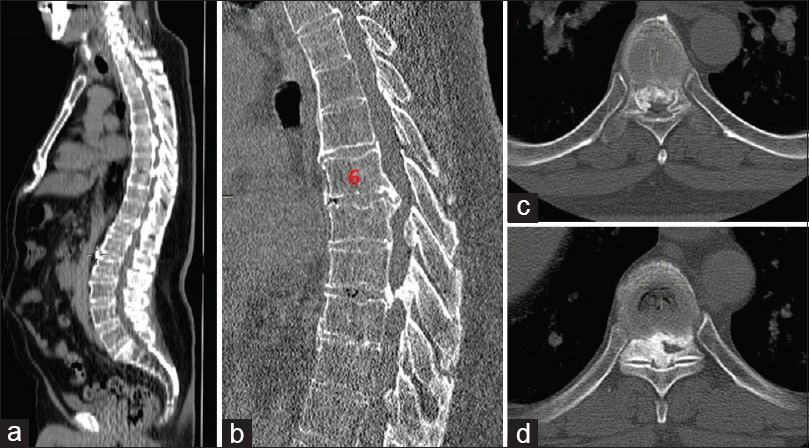
Figure 2
a and b: Sagittal (detailed) CT image demonstrating calcified herniated discs and diffuse ossification over larger parts of the spinal column. c and d: detailed axial CT image at the T6-7 and T8-9 levels showing ossification of the posterior longitudinal ligament, ligamentum flavum and facet joint with subsequent severe spinal stenosis
Surgical procedure
A decompressive laminectomy T5-T9/pedicle instrumented fusion revealed severe OYL. Dural adhesions led to a cerebrospinal fluid (CSF) fistula at the T6-T7 level primarily closed with Prolene, and covered with Tachosil and tissucol (e.g. both sealants). The patient then immediately underwent an additional anterior transthoracic right-sided T6-T7 discectomy. After opening the ossified anterior longitudinal ligament (OALL), the large calcified T6-T7 disc was mobilized and removed; at this point, the posterior positioned fibrin patch was visible, and was supplemented with an anterior patch of Tachosil. As the Valsalva maneuver revealed no residual CSF leak, an intrapleural low-pressure drain (e.g. to promote lung reexpansion) but no external lumbar CSF drain was placed.
Postoperative course
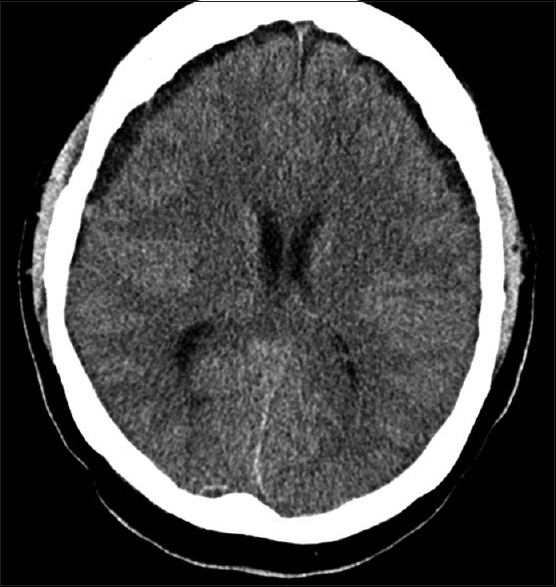
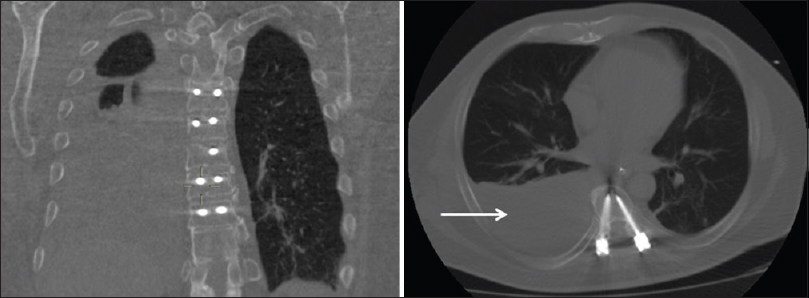
Postoperatively, he became paraplegic. The postoperative MR showed no hemorrhage. The intrapleural drain was removed on postoperative day 2. As he continued to experience orthostatic headache, bed rest was originally prescribed; however, 3 days later he was found unresponsive. When the brain CT showed bilateral subdural hematomas, bilateral burr holes were placed and the clot was evacuated [
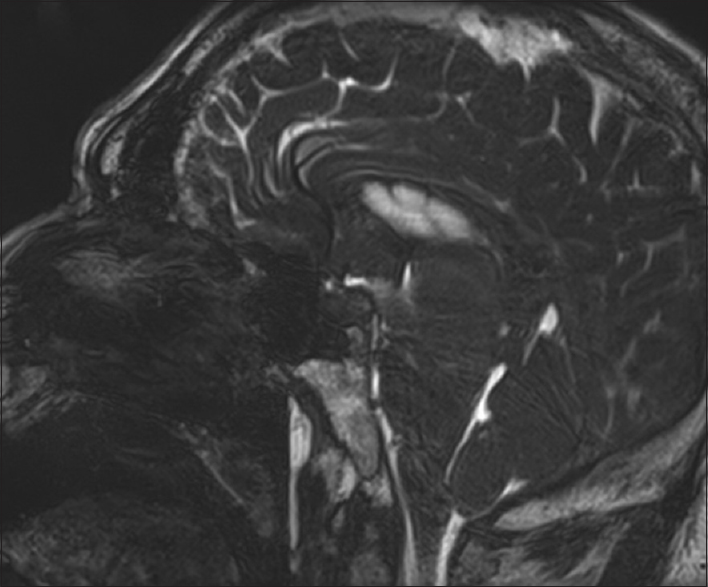
When chest X-rays showed a large right-sided pleural fistula attributed to a persistent CSF leak, repeated anterior exploration (posterior had failed to show a fistula) allowed the dural/pleural fistula to be closed and covered by Tachosil [
CONCLUSION
Intrapleural low-pressure drains placed following transthoracic procedures to facilitate lung reexpansion may potentiate subarachnoid-pleural fistulas that may result in life-threatening intracranial hypotension.