- Department of Neurosurgery, Faculty of Medicine, Zagazig University, Zagazig, Egypt.
Correspondence Address:
Mohamed M. Arnaout, Department of Neurosurgery, Faculty of Medicine, Zagazig University, Zagazig, Egypt. / mmarnaout@zu.edu.eg
DOI:10.25259/SNI_290_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed M. Arnaout1, Magdy O. ElSheikh1, Mansour A. Makia1. Confirmation of accuracy/inaccuracy of lumbar pedicle screw placement using postoperative computed tomography. 11-Oct-2021;12:518
How to cite this URL: Mohamed M. Arnaout1, Magdy O. ElSheikh1, Mansour A. Makia1. Confirmation of accuracy/inaccuracy of lumbar pedicle screw placement using postoperative computed tomography. 11-Oct-2021;12:518. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11165
Abstract
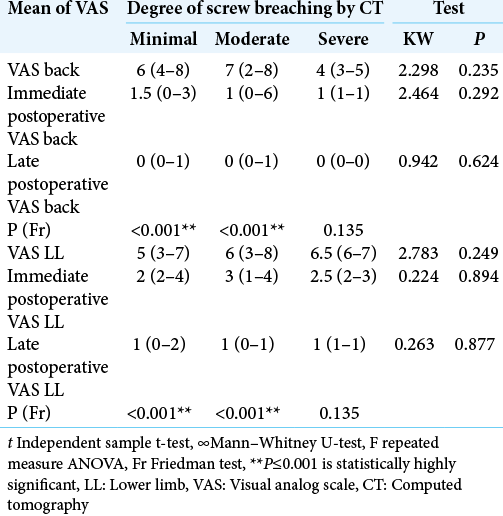
Background: Transpedicular screws are extensively utilized in lumbar spine surgery. The placement of these screws is typically guided by anatomical landmarks and intraoperative fluoroscopy. Here, we utilized 2-week postoperative computed tomography (CT) studies to confirm the accuracy/inaccuracy of lumbar pedicle screw placement in 145 patients and correlated these findings with clinical outcomes.
Methods: Over 6 months, we prospectively evaluated the location of 612 pedicle screws placed in 145 patients undergoing instrumented lumbar fusions addressing diverse pathology with instability. Routine anteroposterior and lateral plain radiographs were obtained 48 h after the surgery, while CT scans were obtained at 2 postoperative weeks (i.e., ideally these should have been performed intraoperatively or within 24–48 h of surgery).
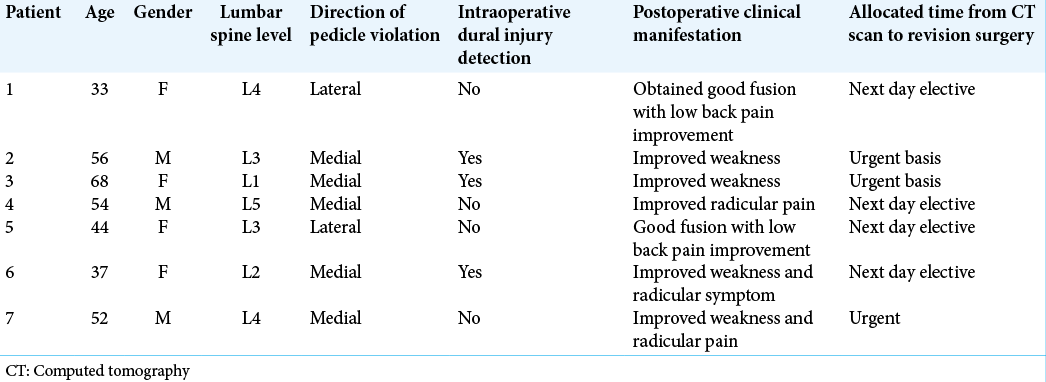
Results: Of the 612 screws, minor misplacement of screws (≤2 mm) was seen in 104 patients, moderate misplacement in 34 patients (2–4 mm), and severe misplacement in 7 patients (>4 mm). Notably, all the latter 7 (4.8% of the 145) patients required repeated operative intervention.
Conclusion: Transpedicular screw insertion in the lumbar spine carries the risks of pedicle medial/lateral violation that is best confirmed on CT rather than X-rays/fluoroscopy alone. Here, we additional found 7 patients (4.8%) who with severe medial/lateral pedicle breach who warranting repeated operative intervention. In the future, CT studies should be performed intraoperatively or within 24–48 h of surgery to confirm the location of pedicle screws and rule in our out medial or lateral pedicle breaches.
Keywords: Computed tomography, Fixation, Lumbar spine, Outcome, Pedicle screw
INTRODUCTION
Transpedicle screws are extensively utilized in the lumbar spine to address instability (i.e., degenerative lumbar spondylolisthesis/deformity, infection, tumors, and other).[
Routine intraoperative conventional fluoroscopy used for pedicle screw placement has been associated with up to a 40% rate of iatrogenic neural/vascular/other injury, in some cases warranting surgical revision.[
Here, we compared the utility of 24–48 h postoperative X-rays versus 2-week postoperative CT scans in confirming the adequacy of pedicle screw placement or the documentation of/extent of medial/lateral pedicle breaches.
MATERIALS AND METHODS
Over a period of 6 months, a consecutive series of 612 pedicle screws were primarily or secondarily placed from L1-L5 in 145 patients. Lumbar fusions were performed for degenerative lumbar disease, degenerative spondylolisthesis, spinal deformity, trauma, or neoplastic lesions [
Surgery
Intraoperatively, pedicle screws were placed utilizing fluoroscopy alone. Routine anteroposterior and lateral plain radiographs were then obtained within 48 h postoperatively, while CT studies were performed at 2 postoperative weeks (i.e., the time of postoperative visits) CT grades for pedicle screw placement included: adequate screw location, or minor (<2 mm), moderate (>2 and <4 mm), or severe (>4 mm) misplacement. In addition, screw positions were correlated with outcomes (i.e., using visual analogue scale [VAS] scores) and with back/lower extremity pain lower limb (LL), both immediately, at 48 h, and 6 months postoperatively.
Data analysis
Data were analyzed using the Statistical Package for the Social Sciences, version 20.0 (SPSS Inc., Chicago, Illinois, USA), and P <0.05 was considered statistically significant.
RESULTS
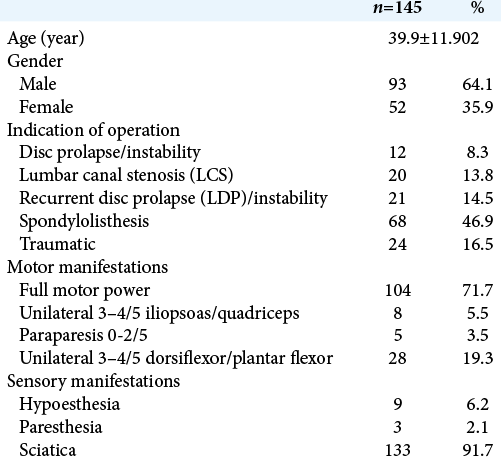
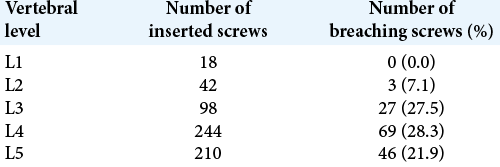
We found that 467 (76.3% of total) pedicle screws were adequately placed, while 104 (16.9%) had minor, 34 (5.6%) had moderate pedicle breaches; none required repeated surgery. The most common level for a breach was at the L4 level (i.e., 28.3% of L4 screws were misplaced) [
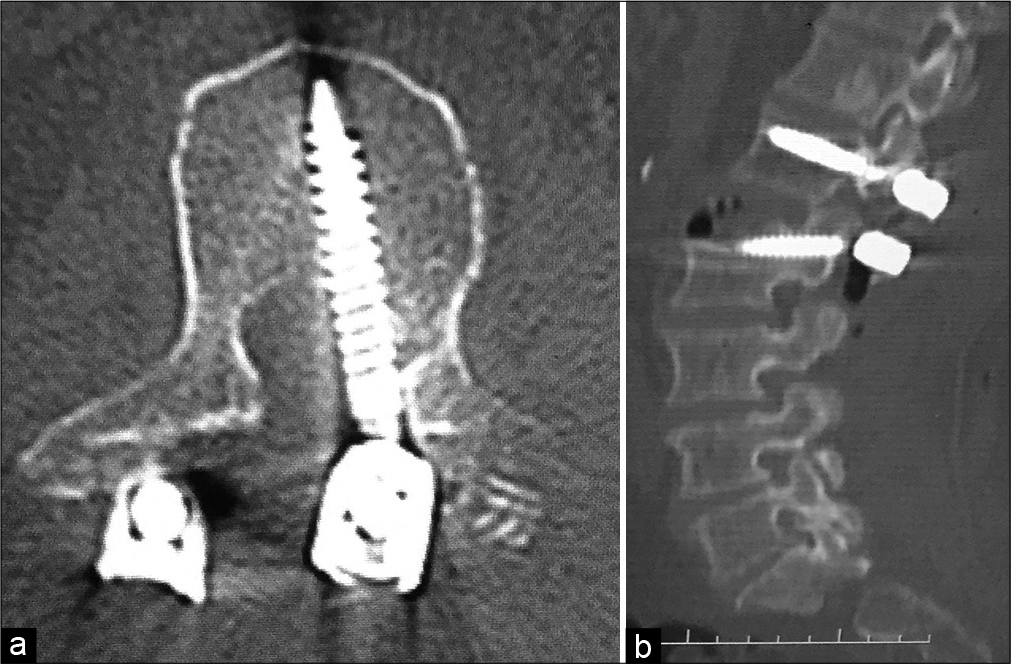
Figure 1:
(a and b) Images of two axial cuts of computed tomography (CT) scan at L4 level in a case of transpedicle screws fixation from L1 to L5 due to lumbar canal stenosis with instability. Although the medial breach was located in the right pedicle, the patient was clinically silent. An anterior vertebral body breach with protrusion of the screws through cortical bone >4 mm at the left screw. (c) Sagittal reconstruction of CT scan with reasonable screws locations in the lateral view. (d) Intraoperative fluoroscopy image with good alignment of screws in the lateral plane.
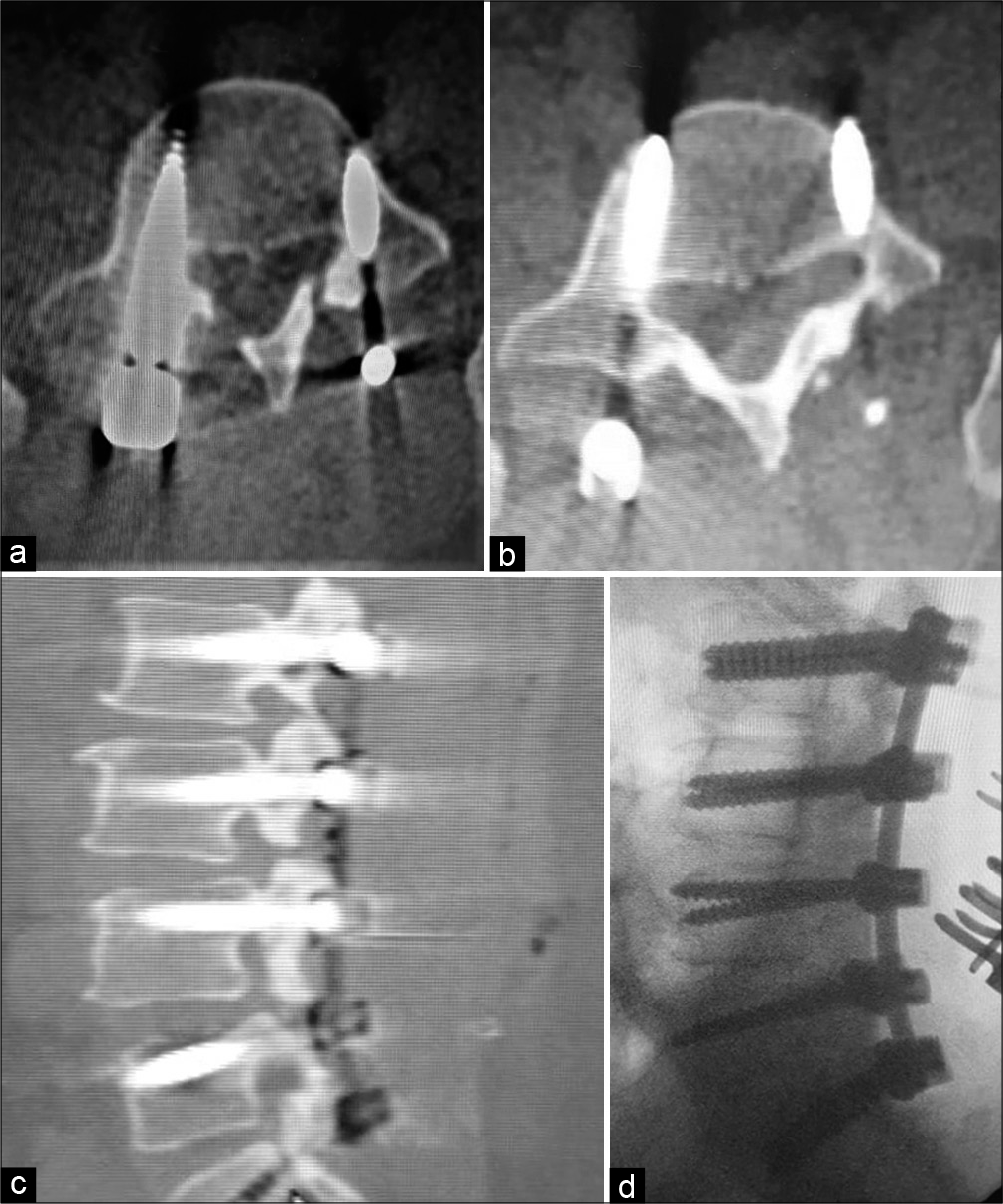
Figure 2:
(a) Representative image of an axial computed tomography (CT) scan at L1 spine in a patient operated for fracture dislocation at L1-L2 with complete loss of function below level. Revision surgery was indicated because of direct contact of the hardware with neural elements in the spinal canal. (b) Sagittal reconstruction image of the aforementioned patient.
Severe pedicle breaches were all requiring urgent/emergent surgical correction. At these latter reoperations, the entry points were rechecked with biplanar intraoperative fluoroscopy [
Postoperative neurological improvement
Nearly 87% of the patients showed immediate postoperative improvement in sensory function that increased to 100% at 6 postoperative months. Motor recovery was immediately seen in 70% of patients, with only minimal additional improvement (73.1%) at 6 postoperative months.
DISCUSSION
CT grading of screw placement and safety zones
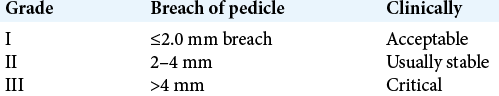
In this study, we grade pedicle screw position as adequate (within the pedicle), or minor (< 2 mm), moderate (>2–< 4 mm), and severe (>4 mm) [
Notably, there is a “safe zone of 4 mm,” comprised 2 mm of epidural space and 2 mm of subarachnoid space (i.e., which can accommodate part of a misplaced screw). If the infringement is more than 4 mm, it should be considered critical and revision should be planned.[
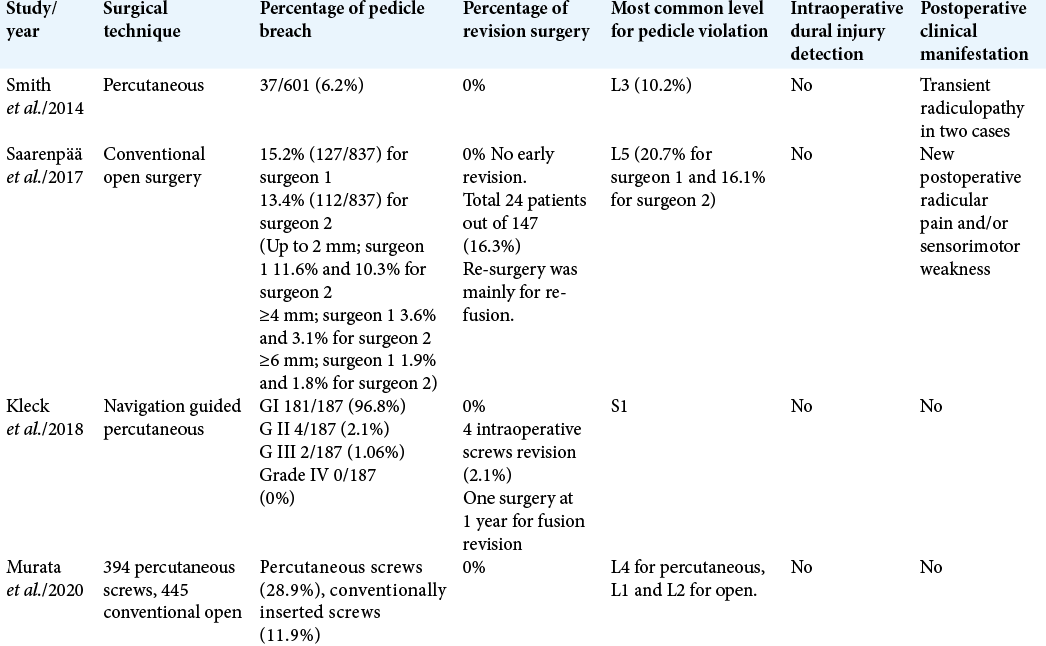
In a study by Kleck et al., numbers of pedicle breach by transpedicular screws were as follows: Grade I 181/187 (96.8%), Grade II 4/187 (2.1%), Grade III 2/187 (1.06%), and Grade IV 0/187 [
CONCLUSION
In our series, transpedicular screw insertion in the lumbar spine carried up to 1.1% be risk of pedicle violation/ misplacement as best confirmed on CT scans. In the future, CT studies should ideally be performed intraoperatively or no later than 24–48 h postoperatively so that necessary revision surgery may be performed in a more timely fashion to offer patients optimal outcomes.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdelbary TH, Arnaout MM. Bone graft alone versus cage with bone graft in lumbar spine interbody fusion. Zagazig Univ Med J. 2019. 68: 85
2. Caelers IJ, Rijkers K, van Kuijk SM, van Santbrink H, de Bie RA, van Hemert WL. Neurological events due to pedicle screw malpositioning with lateral fluoroscopy-guided pedicle screw insertion. J Neurosurg Spine. 2020. 33: 806-11
3. Epstein NE. Commentary: Utility of the O-Arm in spinal surgery. Surg Neurol Int. 2014. 5: S517
4. Kleck CJ, Johnson C, Akiyama M, Burger EL, Cain CJ, Patel VV. One-step minimally invasive pedicle screw instrumentation using O-Arm and stealth navigation. Clin Spine Surg. 2018. 31: 197-202
5. Murata K, Fujibayashi S, Otsuki B, Shimizu T, Masamoto K, Matsuda S. Accuracy of fluoroscopic guidance with the coaxial view of the pedicle for percutaneous insertion of lumbar pedicle screws and risk factors for pedicle breach. J Neurosurg Spine. 2020. 34: 52-9
6. Saarenpää I, Laine T, Hirvonen J, Hurme S, Kotilainen E, Rinne J. Accuracy of 837 pedicle screw positions in degenerative lumbar spine with conventional open surgery evaluated by computed tomography. Acta Neurochir (Wien). 2017. 159: 2011-7
7. Scarone P, Vincenzo G, Distefano D, Del Grande F, Cianfoni A, Presilla S. Use of the Airo mobile intraoperative CT system versus the O-Arm for transpedicular screw fixation in the thoracic and lumbar spine: A retrospective cohort study of 263 patients. J Neurosurg Spine. 2018. 29: 397-406
8. Smith ZA, Sugimoto K, Lawton CD, Fessler RG. Incidence of lumbar spine pedicle breach after percutaneous screw fixation: A radiographic evaluation of 601 screws in 151 patients. Clin Spine Surg. 2014. 27: 358-63
9. Theologou M, Theologou T, Zevgaridis D, Skoulios N, Matejic S, Tsonidis C. Pedicle screw placement accuracy impact and comparison between grading systems. Surg Neurol Int. 2017. 8: 131