- Department of Neurosurgery, Bezmialem Vakif University Medical School, Istanbul, Turkey,
- Department of Oncology, North Middlesex University Hospital, London, United Kingdom,
- Department of Oncology, Oxford University Hospitals NHS Trust, Churchill Hospital, Oxford, United Kingdom.
Correspondence Address:
Georges Sinclair
Department of Neurosurgery, Bezmialem Vakif University Medical School, Istanbul, Turkey,
DOI:10.25259/SNI_191_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Georges Sinclair1,2, Philippa Johnstone3, Mustafa Aziz Hatiboglu1. Considerations for future novel human-infecting coronavirus outbreaks. 29-Aug-2020;11:260
How to cite this URL: Georges Sinclair1,2, Philippa Johnstone3, Mustafa Aziz Hatiboglu1. Considerations for future novel human-infecting coronavirus outbreaks. 29-Aug-2020;11:260. Available from: https://surgicalneurologyint.com/surgicalint-articles/10234/
Abstract
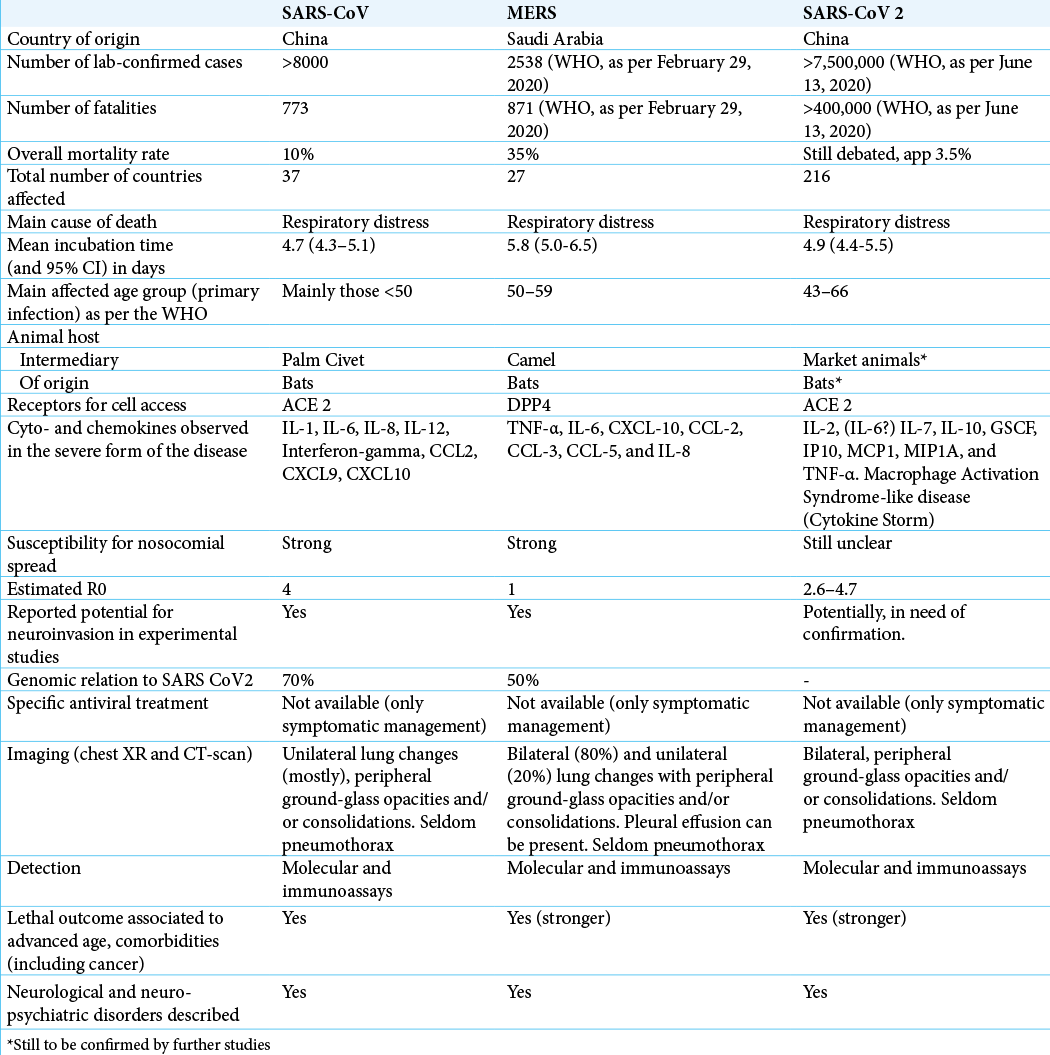
Up until, June 13, 2020, >7,500,000 cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and >400,000 deaths, across 216 countries, have been confirmed by the World Health Organization (WHO). With reference to the two previous beta-CoV outbreaks (SARS-CoV and middle east respiratory syndrome [MERS]), this paper examines the pathophysiological and clinical similarities seen across all three CoVs, with a special interest in the neuroinvasive capability and subsequent consequences for patients with primary or metastatic brain tumors. More widely, we examine the lessons learned from the management of such large-scale crises in the past, specifically looking at the South Korean experience of MERS and the subsequent shift in disaster management response to SARS-CoV-2, based on prior knowledge gained. We assess the strategies with which infection prevention and control can, or perhaps should, be implemented to best contain the spread of such viruses in the event of a further likely outbreak in the future.
Keywords: Infection control and prevention, Middle East respiratory syndrome, Neuroinvasion, Severe acute respiratory syndrome coronavirus 2, Severe acute respiratory syndrome coronavirus
BACKGROUND
Up until, June 13, 2020, >7,500,000 cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and >400,000 deaths, across 216 countries, have been confirmed by the World Health Organization (WHO).[
While SARS-CoV-2 associated disease (also known as coronavirus disease or COVID 19) continued to spreading in most continents, East-Asian countries were the first to bring hope, with reports of small numbers of confirmed cases and low fatality rate 3–4 months following the outbreak in China.[
COVS: THE “BASICS” IN RETROSPECT
The first human infecting CoV presenting with respiratory symptoms was reported in the Lancet as early as 1966 by Gosain et al.[
1. The SARS-CoV
Emanating from an animal market in Guangdong (China), the virus spread to 37 countries, infecting >8000 persons; 774 casualties were reported between 2002 and 2003, setting the mortality rate at around 10%.[
2. The MERS-CoV
Initially identified in Saudi Arabia in 2012, this beta-CoV managed to spread to 27 countries.[
3. The SARS-CoV-2
With its epicenter in the city of Wuhan (China), this novel form of human-infecting betaCoV was first reported in late December 2019.[
Although SARS-CoV-2 appears to affect male and female patients equally in numbers, the fatality rate is seemingly higher in men, possibly due to a difference in immunological responses surrogate to gender itself and gender-associated social behavior, such as smoking.[
SARS-COV-2: FURTHER CLINICAL AND PATHOPHYSIOLOGICAL CONSIDERATIONS
With an incubation time stretching from 1 to 14 days (commonly 3–7 days), the clinical management of SARS- Cov-2 remains structured on symptomatic care, dynamically hinging on the severity, and complexity of the clinical evolution. Non-neurologic symptoms from SARS-CoV-2 are often diffuse; pyrexia, shivers, fatigue, loss appetite, nasal congestion, sneezing, sore throat, cough, shortness of breath, nausea, vomiting, diarrhea, coagulopathies, skin rashes, and myalgia have been reported.[
MAS, also known as secondary hemophagocytic lymphohistiocytosis, has been commonly linked to viral infections, autoimmune disorders, and malignancy; although the pathogenesis is still poorly understood, it is thought that the cytokine storm results in activation of macrophages, causing hemophagocytosis and contributing to disseminated intravascular coagulation, as well as contributing to multi- organ dysfunction.[
Finally, the differential diagnosis can include bacterial infections (e.g., L. pneumophila, and S. pneumoniae), other viral infections (rhinovirus, adenovirus, influenza, parainfluenza, human metapneumovirus, and respiratory syncytial virus) and other non-infectious etiology, such as malignancies, pulmonary embolism, vasculitis, and dermatomyositis.[
Ramifications of neurotropism
Of interest, neurological symptoms such as headaches, nausea, anosmia, loss of taste, acute cerebrovascular complications, diplopia, ataxia, seizures, drowsiness, consciousness deficit, depression, anxiety, delirium, posttraumatic stress, and cortisone-free subthreshold of mania have also been reported.[
Therefore, in view of the genomic/phylogenetic, pathophysiological, and clinical traits shared among the above- mentioned human-infecting beta-CoVs, we hypothesize that, until proven otherwise, SARS-CoV-2 may well utilize similar mechanisms as those employed by MERS and SARS-CoV to effectively invade host neural cells and safely replicate in the CNS, ultimately leading to peripheral and central neurologic injury as well as extracranial symptomatology, including severe respiratory failure. Furthermore, considering the increased risk of COVID-19 in cancer patients,[
TREATMENTS AND TRIALS
Unfortunately, as pointed out above, there are no specific antiviral treatments or vaccines against SARS-CoV-2 at present; symptomatic care remains the foundation of hospital management. Oxygen therapy, continuous positive airways pressure (CPAP) support, and mechanical ventilation are effective at different stages of the infection, hinging on the degree of severity of respiratory problems; thorough guidelines and indications have been developed in the context of SARS-CoV-2-associated ARDS and can be found in more detail elsewhere.[
Several SARS-CoV-2 trials are in pipeline across the US, Europe, and Asia, covering the fields of epidemiology, detection, treatment, and vaccination.[
PREVENTION AND CONTROL OF SARS-COV-2: WHERE ARE WE TODAY?
Infection prevention and control (IPC) measures remain the cornerstone of SARS-Cov-2 management in many countries;[
Trying to understand the reasons as to how we failed to avoid the current situation remains complex from a geopolitical and world economics perspective. However, in the face of this type of outbreak, medical professionals across different disciplines have recognized the need for early measures such as (i) the systematic distribution and time-effective use of respiratory masks (e.g., FFP3 and N95 masks) and other personal protective equipment (PPE) for the directly exposed health-care staff, (ii) the sustainability of the medical supply chain, and (iii) the supply of equipment allowing non- invasive and invasive ventilation (such as oxygen supply, CPAP machines, and mechanical ventilators).
Furthermore, in view of the basic reproduction number of SARS-CoV-2 combined with factors such an aging population, restricted hospital resources (particularly in some Emergency departments and Intensive Care Units), and lack of specific anti-SARS-CoV-2 treatment (or vaccine), medical professionals stressed from the early stages of COVID-19, the need to bring the effective reproduction number <1 through unrestricted, “targeted” testing of all symptomatic cases. The benefits of upfront testing using the reverse transcriptase- polymerase chain reaction (RT-PCR) test on collected saliva and mucus samples have been widely documented;[
VALUABLE LESSONS FOR FUTURE OUTBREAKS: THE SOUTH KOREAN EXPERIENCE
Following the outbreak of SARS-CoV in China, South Korea implemented a series of restrictive measures, which ultimately led to three confirmed cases of SARS-CoV with no fatalities. Already then, the WHO acknowledged South Korea as a model nation for its effective fight against SARS-CoV.[
From an early stage, experts identified a series of dysfunctions in terms of disaster management and communication capability; experts also recognized the importance of a short window between the identification of cases and the activation of control measures to restrain the spread of MERS or other agents with similar behavioral patterns.[
On January 20, 2020, the first individual with SARS- CoV-2 was identified in South Korea; the number of cases rapidly increased during the following few weeks, with its epicenter in Daegu.[
In terms of governmental action, after confirming their first case, the South Korean authorities escalated the crisis level from blue to yellow, establishing a Korean CDC COVID-19 rapid response team. A week later (January 27), the crisis level was further elevated to orange, and the Ministry of Health and Welfare Central Accident Management Headquarters for the COVID-19 was established.[
In addition to the above, the benefits of incorporating cutting edge technology to public control measures cannot be underestimated; for example, from an early stage, the South Korean Ministry of Interior and Safety developed a smartphone application (app) to allow those infected or in isolation to keep in contact with case workers with positive results, allowing local authorities to keep track of “superspreaders,” among others. Another app, the “Co100,” was also rapidly developed from governmental data to inform users when they come within 100 m of a site visited by someone infected. Alike the latter mentioned apps, a third app was produced to specifically inform citizens of possible shortage and supply of masks at specific sites such as pharmacies.
Finally, despite South Korea’s proximity to China and not launching a total “lockdown” as in the case of many European countries, the WHO and South Korean authorities have reported a sustained, stable number of infected cases with low fatality cases following the escalation and implementation of these measures (12,051 confirmed cases and 277 deaths up to June 13, despite a population >50,000,000 ); similar results in Taiwan, Japan, Singapore, and Germany further support an approach comparable to that seen in South Korea.[
CONCLUSION
This is the third outbreak by a novel human-infecting beta- CoVs in 18 years, with worldwide consequences; this should be taken as sign of warning, as it unlikely to be the last. SARS- CoV, MERS, and SARS-CoV-2 all share common and complex clinical, genomic, and pathophysiologic characteristics with potentially lethal outcomes. Of these three aforementioned CoVs, SARS-CoV-2 has the highest mortality rate due to an inherent high R0 value and an ability to master both animal- to-animal and animal-to-human transmission. Due to several factors, not least including a lack of current targeted treatment, infection control, and preventive measures remain the cornerstone of the management of these types of agents. As proven by the South Korean model, prompt, large-scale testing of suspected individuals, contact tracing and isolation are critical steps in early crisis management aiming to avoid irrational ‘full’ lockdown measures with ensuing detrimental outcomes in the short- and long term. As such, transparent international cooperation between governments and health- institutions based on strict guidelines and obligatory crisis- oriented health-care resources ought to be implemented to prevent further global crises related to novel infectious agents.[
References
1. Adhikari SP, Meng S, Wu Y, Mao YP, Ye RX, Wang QZ. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020. 9: 29
2. Almendros A. Can companion animals become infected with Covid-19?. Vet Rec. 2020. 186: 388-9
3. Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: An international collaborative group. Oncologist. 2020. 25: e936-45
4. Alsolamy S, Arabi YM. Infection with Middle East respiratory syndrome coronavirus. Can J Respir Ther. 2015. 51: 102
5. Berger JR. COVID-19 and the nervous system. J Neurovirol. 2020. 26: 143-8
6. Carr AC. A new clinical trial to test high-dose Vitamin C in patients with COVID-19. Crit Care. 2020. 24: 133
7. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R.editors. Features, Evaluation and Treatment Coronavirus (COVID-19). Treasure Island, FL: Stat Pearls Publishing; 2020. p.
8. COVID-19 Pandemic Planning Scenarios. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html [Last accessed on 2020 Jul 10].
9. Channappanavar R, Fett C, Mack M, Eyck PP, Meyerholz DK, Perlman S. Sex-based differences in susceptibility to SARS-CoV infection. J Immunol. 2017. 198: 4046-53
10. Chan-Yeung M, Xu RH. SARS: Epidemiology. Respirology. 2003. 8: S9-14
11. Chen X, Chughtai AA, Dyda A, MacIntyre CR. Comparative epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia and South Korea. Emerg Microbes Infect. 2017. 6: e51
12. Cheng RZ. Can early and high intravenous dose of Vitamin C prevent and treat coronavirus disease 2019 (COVID-19)?. Med Drug Discov. 2020. 5: 100028
13. Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: An epidemiological outbreak study. Lancet. 2016. 388: 994-1001
14. . COVID-19 National Emergency Response Center; Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention. Early epidemiological and clinical characteristics of 28 Cases of coronavirus disease in South Korea. Osong Public Health Res Perspect. 2020. 11: 8-14
15. Crayne CB, Albeituni S, Nichols KE, Cron RQ. The immunology of macrophage activation syndrome. Front Immunol. 2019. 10: 119
16. .editors. Tackling COVID-19: Health, Quarantine and Economic Measures of South Korea. New Delhi: Ministry of Economy and Finance; 2020. p.
17. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z. Epidemiology of COVID-19 among children in China. Pediatrics. 2020. 145: e20200702
18. FIND Evaluation Update: SARS-CO-2 Molecular Diagnostics. Available from: https://www.finddx.org/covid-19/sarscov2-eval-molecular [Last accessed on 2020 Apr 16].
19. Gosain R, Abdou Y, Singh A, Rana N, Puzanov I, Ernstoff M. COVID-19 and cancer: A comprehensive review. Curr Oncol Rep. 2020. 22: 53
20. Gralinski L, Menachery V. Return of the coronavirus: 2019-nCoV. Viruses. 2020. 12: 135
21. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL. Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020. 12: 988
22. Guarner J. Three emerging coronaviruses in two decades. Am J Clin Pathol. 2020. 153: 420-1
23. Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-an update on the status. Mil Med Res. 2020. 7: 11
24. Hatiboglu MA, Sinclair G. Coronavirus pandemic: How is neurosurgical-oncology practice affected?. Br J Neurosurg. 2020. p.
25. Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myers L. Radiology perspective of coronavirus disease 2019 (COVID-19): Lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. AJR Am J Roentgenol. 2020. 214: 1078-82
26. Hsih WH, Cheng MY, Ho MW, Chou CH, Lin PC, Chi CY. Featuring COVID-19 cases via screening symptomatic patients with epidemiologic link during flu season in a medical center of Central Taiwan. J Microbiol Immunol Infect. 2020. 53: 459-66
27. Ilie PC, Stefanescu S, Smith L. The role of Vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. 2020. 32: 1195-8
28. Iwasaki A and Grubaugh ND. Why does Japan have so few cases of COVID-19?. EMBO Mol Med. 2020. 12: e12481
29. Jakovac H. COVID-19 and vitamin D-is there a link and an opportunity for intervention?. Am J Physiol Endocrinol Metab. 2020. 318: E589
30. Jeon MH, Kim TH. Institutional preparedness to prevent future Middle East respiratory syndrome coronavirus-like outbreaks in republic of Korea. Infect Chemother. 2016. 48: 75-80
31. Jiang X, Rayner S, Luo MH. Does SARS-CoV-2 has a longer incubation period than SARS and MERS?. J Med Virol. 2020. 92: 476-8
32. Karakike E, Giamarellos-Bourboulis EJ. Macrophage activation-like syndrome: A distinct entity leading to early death in Sepsis. Front Immunol. 2019. 10: 55
33. Khan A, Farooqui A, Guan Y, Kelvin DJ. Lessons to learn from MERS-CoV outbreak in South Korea. J Infect Dev Ctries. 2015. 9: 543-6
34. Kickbusch I, Leung GM, Bhutta ZA, Matsoso MP, Ihekweazu C, Abbasi K. Covid-19: How a virus is turning the world upside down. BMJ. 2020. 369: m1336
35. Kim KH, Tandi TE, Choi JW, Moon JM, Kim MS. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: Epidemiology, characteristics and public health implications. J Hosp Infect. 2017. 95: 207-13
36. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020. 55: 105924
37. Lau SK, Chan JF. Coronaviruses: Emerging and re-emerging pathogens in humans and animals. Virol J. 2015. 12: 209
38. Lee J, Rapid Response Team, Kim WJ. Collaborative intervention of Middle East respiratory syndrome: Rapid response team. Infect Chemother. 2016. 48: 71-4
39. Lee KM, Jung K. Factors influencing the response to infectious diseases: Focusing on the case of SARS and MERS in South Korea. Int J Environ Res Public Health. 2019. 16: 1432
40. Li K, Wohlford-Lenane C, Perlman S, Zhao J, Jewell AK, Reznikov LR. Middle East respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J Infect Dis. 2016. 213: 712-22
41. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020. 92: 552-5
42. Li YC, Bai WZ, Hirano N, Hayashida T, Hashikawa T. Coronavirus infection of rat dorsal root ganglia: Ultrastructural characterization of viral replication, transfer, and the early response of satellite cells. Virus Res. 2012. 163: 628-35
43. Li YC, Bai WZ, Hirano N, Hayashida T, Taniguchi T, Sugita Y. Neurotropic virus tracing suggests a membranous-coating-mediated mechanism for transsynaptic communication. J Comp Neurol. 2013. 521: 203-12
44. Liu J, Zheng X, Tong Q, Li W, Wang B, Sutter K. Overlapping and discrete aspects of the pathology and pathogenesis of the emerging human pathogenic coronaviruses SARS-CoV, MERS-CoV, and 2019-nCoV. J Med Virol. 2020. 92: 491-4
45. Liu R, Han H, Liu F, Lv Z, Wu K, Liu Y. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 Cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin Chim Acta. 2020. 505: 172-5
46. Liu Z, Ying Y. The inhibitory effect of curcumin on virus-induced cytokine storm and its potential use in the associated severe pneumonia. Front Cell Dev Biol. 2020. 8: 479
47. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020. 395: 565-74
48. Malik YS, Sircar S, Bhat S, Sharun K, Dhama K, Dadar M. Emerging novel coronavirus. (2019-nCoV)-current scenario, evolutionary perspective based on genome analysis and recent developments. Vet Q. 2020. 40: 68-76
49. Mao L, Wang M, Chen S, He Q, Chang J, Hong C. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study. Med Rxiv. 2020. p.
50. McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020. 19: 102537
51. Memish Z, Perlman S, Van Kerkhove MD, Zumla A. Middle East respiratory syndrome. Lancet. 2020. 395: 1063-77
52. Meo SA, Alhowikan AM, Al-Khlaiwi T, Meo IM, Halepoto DM, Iqbal M. Novel coronavirus 2019-nCoV: Prevalence, biological and clinical characteristics comparison with SARS-CoV and MERS-CoV. Eur Rev Med Pharmacol Sci. 2020. 24: 2012-9
53. National Institutes of Health: US National Library of Medicine. Available from: https://www.clinicaltrials.gov/ct2/results?cond=COVID+19&term=&cntry=&state=&city=&dist=. [Last accessed on 2020 Apr 06].
54. Nicastri E, Petrosillo N, Bartoli TA, Lepore L, Mondi A, Palmieri F. National institute for the infectious diseases L. Spallanzani IRCCS. Recommendations for COVID-19 clinical management. Infect Dis Rep. 2020. 12: 8543
55. Oh MD, Park WB, Park SW, Choe PG, Bang JH, Song K. Middle East respiratory syndrome: What we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018. 33: 233-46
56. Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020. 323: 1-9
57. Patel R, Park J, Shah A, Saif MW. COVID-19 and cancer patients. Cancer Med J. 2020. 3: 40-8
58. Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir Med. 2020. 8: 506-17
59. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020. 7: 611-27
60. Shim E, Tariq A, Choi W, Lee Y, Chowell G. Transmission potential and severity of COVID 19 in South Korea. Int J Infect Dis. 2020. 93: 339-44
61. Silberstein M. Vitamin D: A simpler alternative to tocilizumab for trial in COVID-19?. Med Hypotheses. 2020. 140: 109767
62. Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020. 87: 281-6
63. Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020. 76: 71-6
64. Vellingiri B, Jayaramayya K, Iyer M, Narayanasamy A, Govindasamy V, Giridharan B. COVID-19: A promising cure for the global panic. Sci Total Environ. 2020. 725: 138277
65. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020. 92: 568-76
66. Wenham C, Smith J, Morgan R. COVID-19: The gendered impacts of the outbreak. Lancet. 2020. 395: 846-8
67. .editors. Coronavirus Disease 2019 (COVID-19) Situation Report-77. Geneva: World Health Organization; 2020. p.
68. Middle East Respiratory Syndrome: MERS Situation. Available from: http://www.emro.who.int/health-topics/mers-cov/mers-outbreaks.html [Last accessed on 2020 Jun 15].
69. Consensus Document on the Epidemiology of Severe Acute Respiratory Syndrome (SARS). Available from: https://www.who.int/csr/sars/en/whoconsensus.pdf [Last accessed on 2020 Apr 16].
70. Wu R, Wang L, Kuo HD, Shannar A, Peter R, Chou PJ. An update on current therapeutic drugs treating COVID-19. Curr Pharmacol Rep. 2020. p. 1-15
71. Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 Cases from the Chinese center for disease control and prevention. JAMA. 2020. 323: 1239-42
72. Yin Y, Wunderink R. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018. 23: 130-7
73. Zhang T, Cui X, Zhao X, Wang J, Zheng J, Zheng G. Detectable SARS-CoV-2 viral RNA in feces of three children during recovery period of COVID-19 pneumonia. Med Virol. 2020. 92: 909-14