- Department of Neurosurgery, Neurosurgery Unit, IRCCS Galeazzi Hospital, Milan, Italy
Correspondence Address:
Edvin Zekaj
Department of Neurosurgery, Neurosurgery Unit, IRCCS Galeazzi Hospital, Milan, Italy
DOI:10.4103/2152-7806.191024
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zekaj E, Menghetti C, Saleh C, Isidori A, Bona AR, Aimar E, Servello D. Contralateral interlaminar approach for intraforaminal lumbar degenerative disease with special emphasis on L5-S1 level: A technical note. Surg Neurol Int 21-Sep-2016;7:88
How to cite this URL: Zekaj E, Menghetti C, Saleh C, Isidori A, Bona AR, Aimar E, Servello D. Contralateral interlaminar approach for intraforaminal lumbar degenerative disease with special emphasis on L5-S1 level: A technical note. Surg Neurol Int 21-Sep-2016;7:88. Available from: http://surgicalneurologyint.com/surgicalint_articles/contralateral-interlaminar-approach-intraforaminal-lumbar-degenerative-disease-special-emphasis-l5%e2%80%91s1-level-technical-note/
Abstract
Background:Intraforaminal disc herniations at the L5-S1 level are extremely surgically challenging lesions. Intracanal approaches frequently require partial or total facetectomy, which may lead to instability. Solely extraforaminal approaches may offer limited visualization of the more medial superiorly exiting and inferiorly exiting nerve roots; this approach is also more complicated at L5-S1 due to the often large L5 transverse process and the iliac wing.
Methods:Nine patients with intraforaminal L5-S1 disc herniations, foraminal stenosis, or synovial cysts underwent contralateral interlaminar approaches for lesion resection. Preoperative and postoperative visual analog scale scores were evaluated, and complications were reviewed.
Results:All 9 patients demonstrated immediate postoperative clinical improvement. None of the patients exhibited complications and none developed instability or neuropathic disorders.
Conclusions:Although the number of cases in our sample was very small (9 in total), the contralateral interlaminar approach appeared to effectively address multiple degenerative L5-S1 foraminal pathologies. Large studies are needed to further evaluate the pros and cons of this approach.
Keywords: Contralateral approach, intraforaminal lumbar disc herniation, mini-invasive spine surgery, spinal stability
INTRODUCTION
Intra and or extraforaminal lumbar disc herniations (IELDH) account for 7-12 % of all disc herniations.[
Several surgical approaches to IELDH and other degenerative foraminal diseases include the ipsilateral interlaminar approach with differing degrees of facet joint removal, the contralateral interlaminar approach, the transmuscular extraforaminal approach, the endoscopic approach, and the endoscopic transiliac approaches.[
MATERIALS AND METHODS
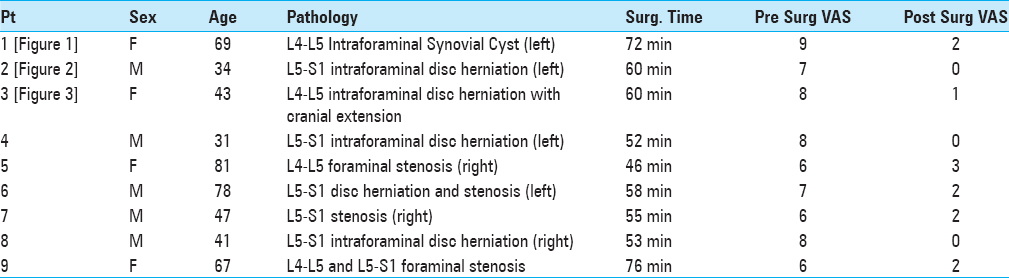
Nine patients underwent contralateral interlaminar approaches for compressive foraminal disease at L4-L5 and L5-S1 levels. There were 5 males and 4 females, with an average age of 54 years. Foraminal pathologies included synovial cysts (1 patient), lumbar discs (5 patients), and stenosis (3 patients) [
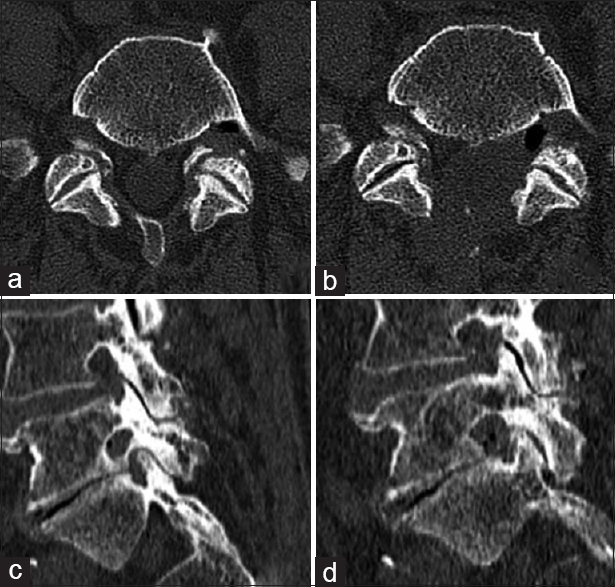
Figure 2
(a) Axial lumbosacral computed tomography (CT) scan showing foraminal stenosis at L5-S1 on the left. (c) Sagittal reconstruction of CT scan showing osteophytes in the lower part of the foramen. (b, d) Postsurgical axial and sagittal CT scan showing removal of the osteophytes and decompression of foramen with preservation of facet joints
Radiological evaluation
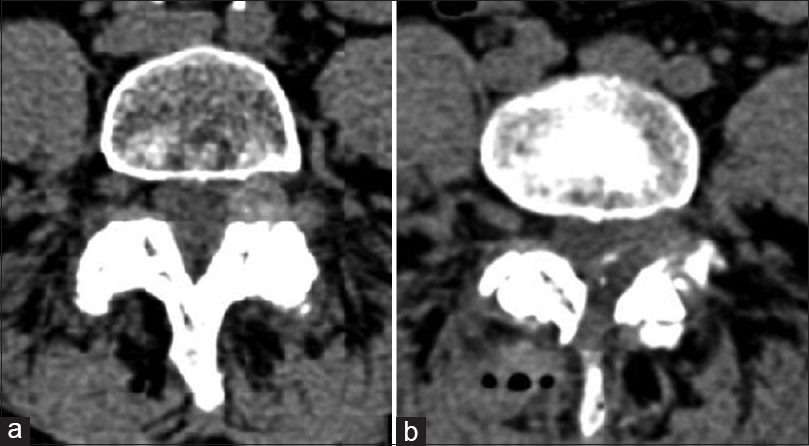
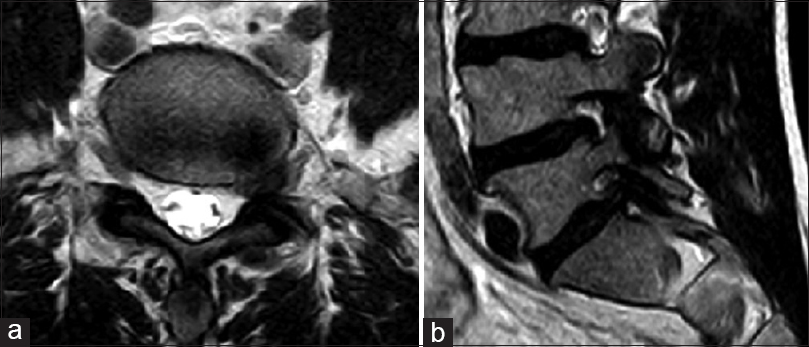
All but 1 patient with a cardiac pacemaker underwent magnetic resonance (MR) studies documenting foraminal compression at the L5-S1 level. Four with foraminal stenosis additionally underwent computed tomography (CT) assessment.
Surgical techniques
Under fluoroscopic guidance, a longitudinal 3-4 cm skin incision off the midline (1-2 cm) opposite to the foraminal degenerative disease was made. A Caspar retractor was utilized to expose the interlaminar space. The operating table was tilted 20–30° away from the operating surgeon, and the Caspar retractor was similarly directed toward the contralateral foramen. Under microscopic visualization, the base of the spinous process and the inferior part of the contralateral lamina were drilled with a 4 mm diamond high speed drill. Part of the contralateral ligamentum flavum was removed with a Kerrison punch to allow for exposure of the dural sac and a contralateral nerve root that were gently retracted, allowing for resection of the disc or other foraminal pathology. In some patients especially those with foraminal stenosis we also used a 2 mm diamond high speed drill to achieve foraminal decompression. Postoperatively, all 9 patients exhibited immediate improvement in sciatic pain, whereas visual analog scale (VAS) scores improved from the preoperative 7, 22 ± 1.03 to postoperative 1, 33 ± 1.05. Notably, all patients returned to work within 45 days from surgery, without significant complications.
DISCUSSION
The contralateral interlaminar approach effectively addressed 9 cases of IELDH, foraminal stenosis, or synovial cyst at L4-L5 and L5-S1 level in this series. This approach minimized the risks of extensive facet joint removal/instability and transient neuropathic pain (e.g., due to manipulation of the dorsal root ganglion) associated with other approaches.
Disadvantages of contralateral approach
Possible disadvantages; first in obese patients the distance from the foramen to skin incision maybe to long rendering surgical maneuvers difficult. The second disadvantage is that this procedure needs two surgeons as the assistant angulates the retractor and protecs the dura mater.
CONCLUSIONS
Although further studies are warranted, the minimally invasive contralateral interlaminar approach appears to be suitable for resecting degenerative intraforaminal pathology at the L5-S1 level.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Epstein NE. Evaluation of various surgical approaches used in the management of 170 far-lateral lumbar disc herniations: Indications and results. J Neurosurg. 1995. 83: 648-56
2. Epstein NE, Epstein JA, Carras R, Hyman RA. Far lateral lumbar disc herniations and associated structural abnormalities: an evaluation in 60 patients of the comparative value of CT, MRI, and myelo-CT in diagnosis and management. Spine. 1990. 15: 534-9
3. Osman SG, Sherlekar S, Malik A, Winters C, Grewal PK, Narayanan M. Endoscopic trans-iliac approach to L5-S1 disc and foramen-A report on clinical experience. Int J Spine Surg. 2014. p. 8-
4. Tessitore E, De Tribolet N. Far-lateral lumbar disc herniation: The microsurgical transmuscular approach. Neurosurgery. 2004. 54: 939-42
5. Yue JJ, Scott DL, Han X, Yacob A. The surgical treatment of single level multi-focal subarticular and paracentral and/or far-lateral lumbar disc herniations: The single incision full endoscopic approach. Int J Spine Surg. 2014. p. 8-