- Department of Neurosurgery, Suzuka General Hospital, Suzuka,
- Department of Neurosurgery, Mie University Graduate School of Medicine, Tsu, Mie, Japan.
Correspondence Address:
Hideki Nakajima, Department of Neurosurgery, Suzuka General Hospital, Suzuka, Mie, Japan.
DOI:10.25259/SNI_713_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hideki Nakajima1, Takuro Tsuchiya1, Shigetoshi Shimizu1, Hidenori Suzuki2. Contrast extravasation from basilar artery without aneurysm formation on digital subtraction angiography in computed tomography angiogram-negative subarachnoid hemorrhage: A case report. 06-Oct-2021;12:498
How to cite this URL: Hideki Nakajima1, Takuro Tsuchiya1, Shigetoshi Shimizu1, Hidenori Suzuki2. Contrast extravasation from basilar artery without aneurysm formation on digital subtraction angiography in computed tomography angiogram-negative subarachnoid hemorrhage: A case report. 06-Oct-2021;12:498. Available from: https://surgicalneurologyint.com/surgicalint-articles/11163/
Abstract
Background: The causes of angiogram-negative subarachnoid hemorrhage (SAH) on initial angiography, which accounts for 10–30% of spontaneous SAH, are heterogeneous and still unclear. We report a case of nonaneurysmal SAH, in which initial computed tomographic angiography (CTA) showed no source of bleeding, but the subsequent digital subtraction angiography (DSA) revealed contrast extravasation from the basilar artery without aneurysms.
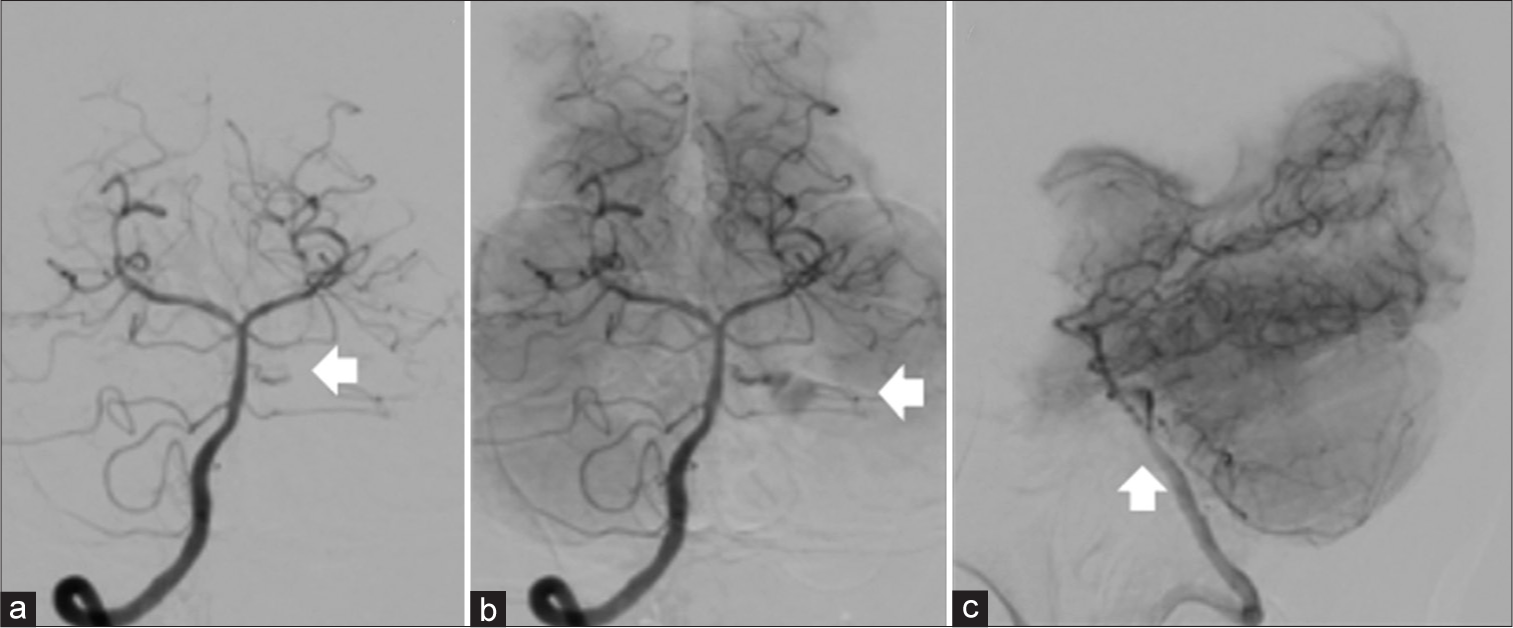
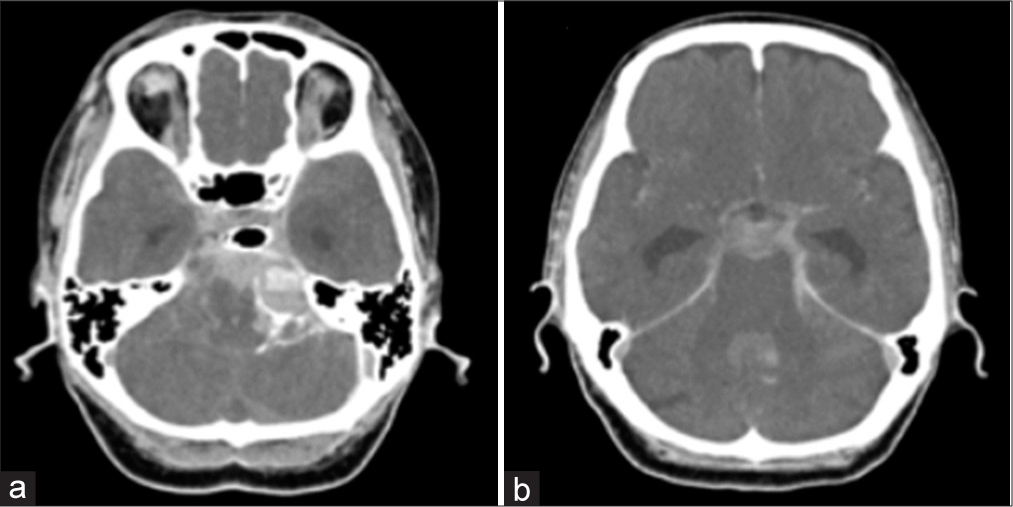
Case Description: A 67-year-old woman with a medical history of hypertension presented as SAH of World Federation of Neurological Surgeons Grade II. CTA on admission did not show any cause of bleeding and DSA was subsequently performed to show contrast extravasation from a perforator of the middle third of the basilar artery without aneurysms during the subsequent DSA, resulting in profound deterioration SAH and neurological status. The patient was conservatively treated. Follow-up DSAs on days 2 and 16 showed no source of bleeding as well.
Conclusion: Although the precise cause of bleeding in this case is uncertain, SAH might be caused by local dissection of the basilar artery perforator, and the bleeding site might heal spontaneously without forming of a pseudoaneurysm.
Keywords: Basilar artery perforator aneurysm, Contrast extravasation, Subarachnoid hemorrhage, Unknown etiology
INTRODUCTION
Approximately 10–30% of spontaneous subarachnoid hemorrhage (SAH) patients have unknown origin on initial angiographic imaging.[
CASE PRESENTATION
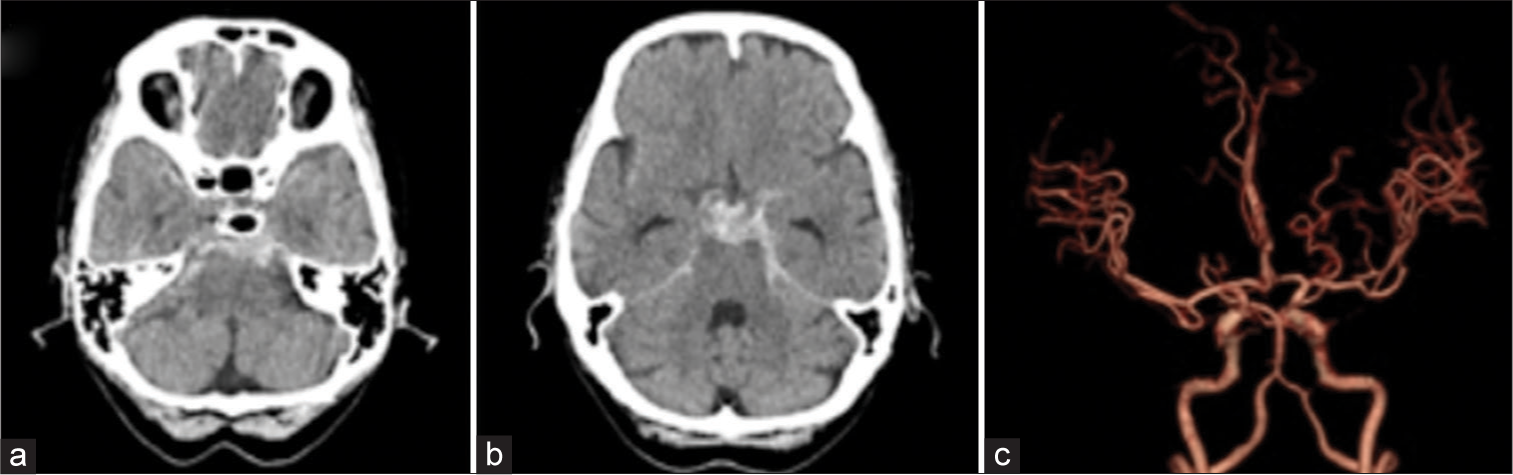
A 67-year-old woman with a medical history of hypertension presented to our hospital after sudden onset of headache with vomiting. On admission, she was drowsy, but there were no neurological deficits. The blood pressure and pulse rate were 197/111 mmHg and 84 beats/min, respectively. She was clinically judged World Federation of Neurological Surgeons Grade II. CT of the head showed SAH of Fisher Group 3, especially in the prepontine cistern, and CTA showed no source of bleeding [
Figure 4:
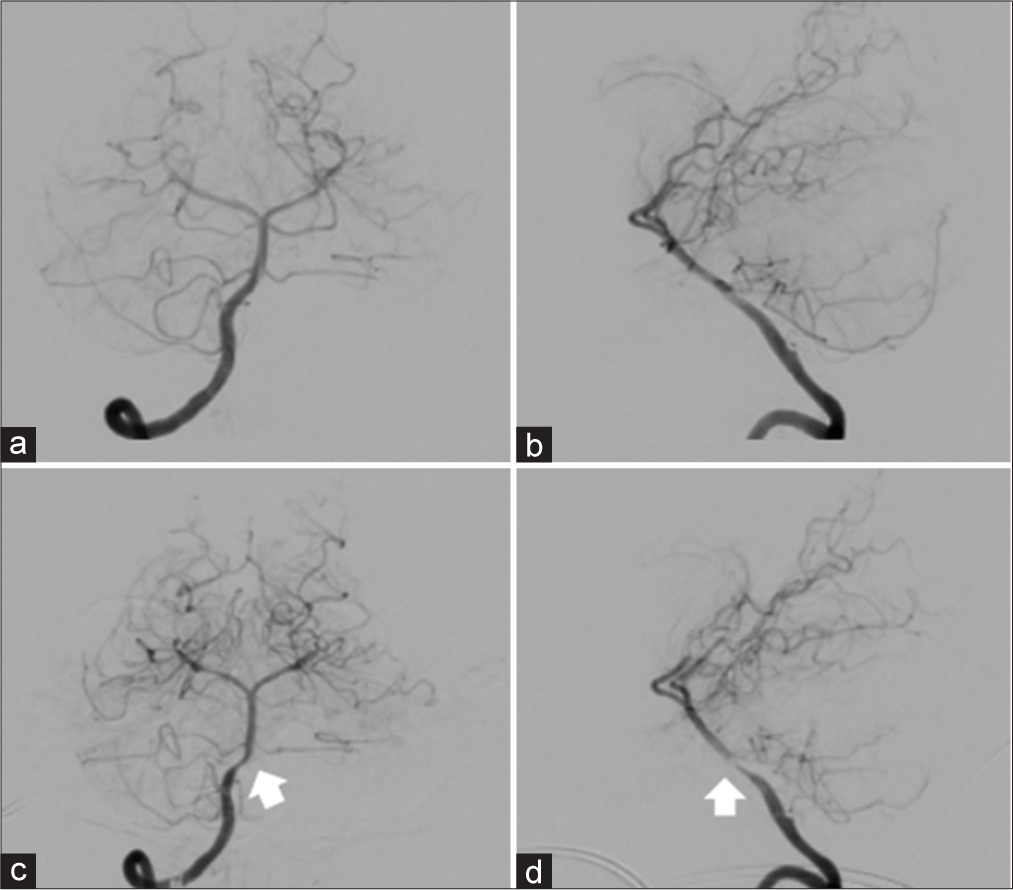
Right vertebral artery angiography on days 2 (a, anteroposterior view; b, lateral view) and 16 (c, anteroposterior view; d, lateral view). (a and b) No source of hemorrhage is shown, and the wall of the basilar artery is smooth. (c and d) No cause of hemorrhage is revealed, but vasospasm of the basilar artery (arrow) is shown.
DISCUSSION
Spontaneous SAH is caused by rupture of a cerebral aneurysm in 80–90% of patients.[
Possible sources of angiogram-negative SAH include vascular malformations, tumors, vasculitides, infections, venous thromboses, and nonvisualized aneurysms.[
DSA is the gold standard in terms of diagnosing the source of bleeding. However, CTA is more rapid and less invasive than DSA.[
Because there was no treatable aneurysm and it is difficult to explore the middle third basilar artery in a direct surgery, we performed conservative therapy in this case. DSA on days 2 and 16 showed neither contrast extravasation nor the source of bleeding, and no rebleeding occurred during the hospitalization. To the best of our knowledge, there were no cases of SAH in which there was only contrast extravasation without aneurysm shown on DSA following negative findings on CTA as in the present case. However, we found four cases of SAH in which there were negative findings on DSA following contrast extravasation without aneurysm on CTA.[
Although the precise cause of bleeding in this case is uncertain, the possibility of basilar artery perforator aneurysms (BAPAs) should be considered: BAPAs can cause angiogram-negative SAH and spontaneously disappear.[
CONCLUSION
SAH with no visualization of bleeding sources on CTA and contrast extravasation from a perforator of the basilar artery on DSA is extremely rare. Although thrombosis developed immediately after the initial bleeding, rebleeding occurred during the subsequent DSA and contrast extravasation from a perforator of the middle third of the basilar artery was observed, suggesting that the mechanism of bleeding might include a localized dissection like BAPAs. The present case suggests that there may be a group of diseases which cause the localized dissection of a perforator of the basilar artery and result in SAH without forming aneurysms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Catapano JS, Lang MJ, Koester SW, Wang DJ, DiDomenico JD, Fredrickson VL. Digital subtraction cerebral angiography after negative computed tomography angiography findings in non-traumatic subarachnoid hemorrhage. J Neurointerv Surg. 2020. 12: 526-30
2. Chavent A, Lefevre PH, Thouant P, Cao C, Kazemi A, Mourier K. Spontaneous resolution of perforator aneurysms of the posterior circulation. J Neurosurg. 2014. 121: 1107-11
3. Cho WH, Choi HJ, Nam KH, Lee JI. Contrast extravasation on computed tomography angiography imitating a basilar artery trunk aneurysm in subsequent conventional angiogram-negative subarachnoid hemorrhage: Report of two cases with different clinical courses. J Cerebrovasc Endovasc Neurosurg. 2015. 17: 20-6
4. Enomoto N, Shinno K, Tamura T, Shikata E, Shono K, Takase K. Ruptured basilar artery perforator aneurysm: A case report and review of the literature. NMC Case Rep J. 2020. 7: 93-100
5. Flaherty ML, Haverbusch M, Kissela B, Kleindorfer D, Schneider A, Sekar P. Perimesencephalic subarachnoid hemorrhage: Incidence, risk factors, and outcome. J Stroke Cerebrovasc Dis. 2005. 14: 267-71
6. Ghogowala Z, Shumacher JM, Ogilvy CS. Distal basilar perforator artery aneurysm: Case report. Neurosurgery. 1996. 39: 393-6
7. Goddard AJ, Tan G, Becker J. Computed tomography angiography for the detection and characterization of intra-cranial aneurysms: Current status. Clin Radiol. 2005. 60: 1221-36
8. Inamasu J, Nakamura Y, Saito R, Horiguchi T, Kuroshima Y, Mayanagi K. “Occult” ruptured cerebral aneurysms revealed by repeat angiography: Result from a large retrospective study. Clin Neurol Neurosurg. 2003. 106: 33-7
9. Kostić A, Stojanov D, Stefanović I, Novak V, Kostić E, Benedeto-Stojanov D. Complications after angiogram-negative subarachnoid haemorrhage: Comparative study of pretruncal and nonpretruncal hemorrhage patients. Srp Arh Celok Lek. 2012. 140: 8-13
10. Marcolini E, Hine J. Approach to the diagnosis and management of subarachnoid hemorrhage. West J Emerg Med. 2019. 20: 203-11
11. Marinković SV, Gibo H. The surgical anatomy of the perforating branches of the basilar artery. Neurosurgery. 1993. 33: 80-7
12. Mizutani T, Kojima H, Miki Y. Arterial dissections of penetrating cerebral arteries causing hypertension-induced cerebral hemorrhage. J Neurosurg. 2000. 93: 859-62
13. Mohan M, Islim AI, Rasul FT, Rominiyi O, deSouza RM, Poon MT. Subarachnoid haemorrhage with negative initial neurovascular imaging: A systematic review and meta-analysis. Acta Neurochir (Wien). 2019. 161: 2013-26
14. Rinkel GJ, Wijdicks EF, Vermeulen M, Ramos LM, Tanghe HL, Hasan D. Nonaneurysmal perimesencephalic subarachnoid hemorrhage: CT and MR patterns that differ from aneurysmal rupture. AJNR Am J Neuroradiol. 1991. 12: 829-34
15. Ronkainen A, Hernesniemi J. Subarachnoid haemorrhage of unknown aetiology. Acta Neurochir (Wien). 1992. 119: 29-34
16. Schwartz TH, Solomon RA. Perimesencephalic nonaneurysmal subarachnoid hemorrhage: Review of the literature. Neurosurgery. 1996. 39: 433-40
17. Stetson ND, Pile-Spellman J, Brisman JL. Contrast extravasation on computed tomographic angiography mimicking a basilar artery aneurysm in angiogram-negative subarachnoid hemorrhage: Report of 2 cases. Neurosurgery. 2012. 71: E1047-52
18. Thaker NG, Turner JD, Cobb WS, Hussain I, Janjua N, He W. Computed tomographic angiography versus digital subtraction angiography for the postoperative detection of residual aneurysms: A single-institution series and meta-analysis. J Neurointerv Surg. 2012. 4: 219-25
19. Walcott BP, Stapleton CJ, Koch MJ, Oglivy CS. Diffuse patterns of nonaneurysmal subarachnoid hemorrhage originating from the basal cisterns have predictable vasospasm rates similar to aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2015. 24: 795-801
20. Wong H, Hodgson L, Banfield J, Shankar JJ. Digital subtraction angiography for CT angiogram negative hemorrhages. Can J Neurol Sci. 2018. 45: 522-6