- Department of Spine Surgery, Robert Jones and Agnes Hunt NHS Foundation Trust, Oswestry, Shropshire, United Kingdom,
- Wrightington, Wigan and Leigh NHS Foundation Trust, Wrightington Hospital, Wrightington, Lancashire, United Kingdom.
Correspondence Address:
Alok Gadkari, Department of Spine Surgery, Robert Jones and Agnes Hunt NHS Foundation trust, Oswestry, Shropshire, United Kingdom.
DOI:10.25259/SNI_545_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alok Gadkari1, Aashish Ghodke1, Amrit Jha2. Correlation of pelvic incidence and pelvic parameters in lumbar spondylolisthesis. 09-Sep-2022;13:405
How to cite this URL: Alok Gadkari1, Aashish Ghodke1, Amrit Jha2. Correlation of pelvic incidence and pelvic parameters in lumbar spondylolisthesis. 09-Sep-2022;13:405. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11861
Abstract
Background: Pelvic incidence (PI) and pelvic parameters (PP) regulate the sagittal alignment of the spine and the pelvis in normal populations. Correlation of PI even more so than PP with lumbar spondylolisthesis (LS) would be useful for surgical planning.
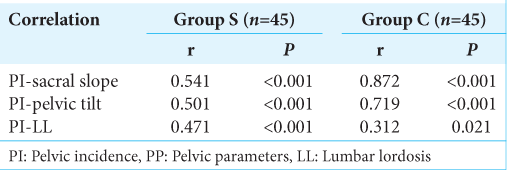
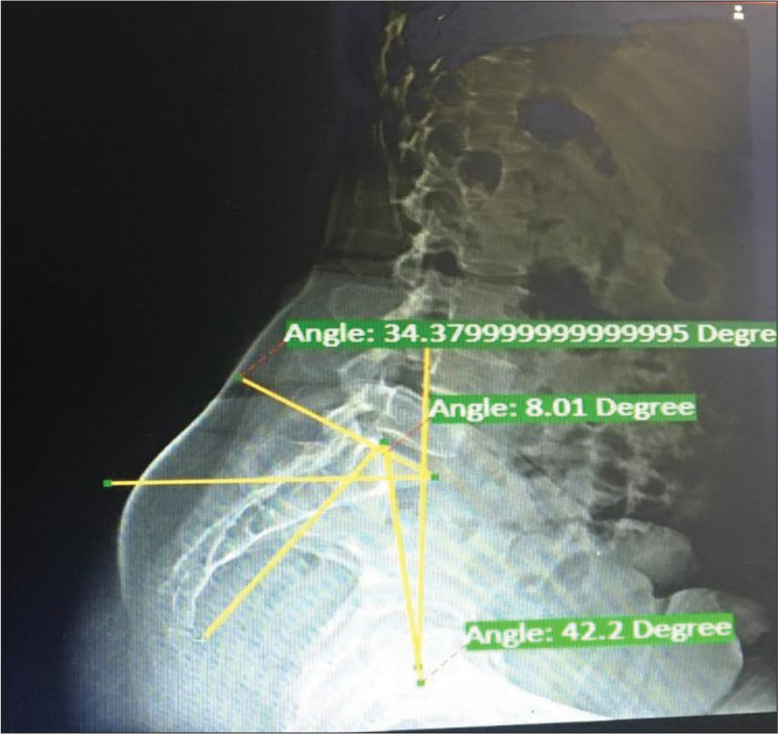
Methods: This study included 45 patients randomly selected with LS. They were divided into two groups; Group S had LS and Group C had low back pain due to other causes. All patients received lateral standing radiographs of the spine and pelvis. Based on these films, we measured the sacral slope, pelvic tilt, PI, and lumbar lordosis (LL).
Results: There were significant correlations between the PI and the sacral slope, pelvic tilt, and LL in Group S (P
Conclusion: Changes in spinopelvic parameters reflecting pelvic compensatory mechanisms differ depending on the extent of PI in patients with LS. In short, higher PI values correlated with more significant degrees of degenerative LS in Group S population.
Keywords: Lumbar lordosis, Lumbar spondylolisthesis, Pelvic incidence, Pelvic parameters
INTRODUCTION
The previous reports demonstrate that the pelvic incidence (PI) determines the sagittal spinal and pelvic alignment in normal populations. Understanding sagittal balance, including spinal alignment and the pelvic orientation, is critical for spine surgeons. Here, we evaluated the role of PI as it related to lumbar spondylolisthesis (LS) in patients under consideration for lumbar surgery.
MATERIALS AND METHODS
Clinical population
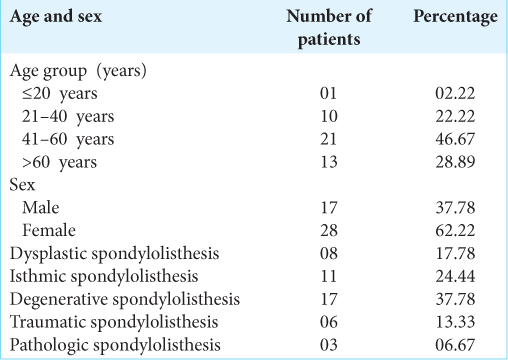
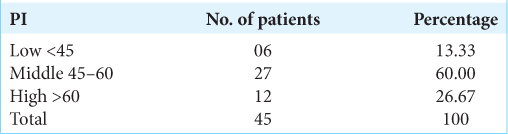
We randomly selected 45 patients with LS. Patients were all above 18 years of age and had LS. Those who had prior surgery were excluded from the study. Patients were divided into two groups; Group S (45 patients) had LS, while Group C (45 patients) had low back ache due to other causes. Patients were assessed utilizing lateral standing radiographs to determine sacral slope, pelvic tilt lumbar lordosis (LL), and the PI.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences version 20.0 software. For qualitative data, various rates, ratios, and percentage (%) were calculated. For quantitative data, mean, SD, median, etc., were calculated. A two-tailed test with P < 0.05 was considered as statistically significant.
RESULTS
DISCUSSION
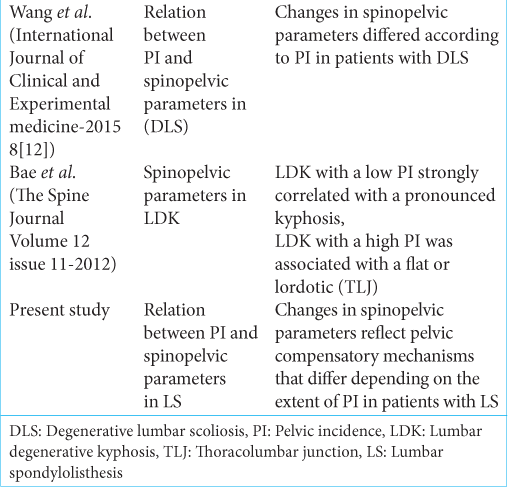
Wang et al. identified the influence of PI on spinopelvic parameters in patients with degenerative lumbar scoliosis (DLS).[
CONCLUSION
Changes in spinopelvic parameters reflect pelvic compensatory mechanisms that differ depending on the extent of PI in patients with LS.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bae JS, Jang JS, Lee SH, Kim JU. Radiological analysis of lumbar degenerative kyphosis in relation to pelvic incidence. Spine J. 2012. 12: 1045-51
2. Wang H, Ma L, Yang D, Ding W, Shen Y, Zhang Y. Radiological analysis of degenerative lumbar scoliosis in relation to pelvic incidence. Int J Clin Exp Med. 2015. 8: 22345-51