- Department of Neurosurgery, McMaster University, Hamilton, Canada.
- Department of Diagnostic Imaging, Health Sciences North, Sudbury, Ontario, Canada.
Correspondence Address:
Taylor Duda, Department of Neurosurgery, McMaster University, Hamilton, Ontario, Canada.
DOI:10.25259/SNI_221_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Taylor Duda, Euan Zhang2, Kesava Reddy1. Craniocerebral gunshot injury bullet migration to the cardiac right ventricle. 30-Sep-2021;12:491
How to cite this URL: Taylor Duda, Euan Zhang2, Kesava Reddy1. Craniocerebral gunshot injury bullet migration to the cardiac right ventricle. 30-Sep-2021;12:491. Available from: https://surgicalneurologyint.com/surgicalint-articles/11136/
Abstract
Background: Missile embolism is the process of slow velocity projectiles penetrating into vascular spaces followed by arterial, venous, or paradoxical embolism of the fragments. This is a rare complication in craniocerebral gunshot injuries (CGI), with only five other cases previously published demonstrating pulmonary or arterial emboli from these injuries. There is a high rate of mortality from these injuries.
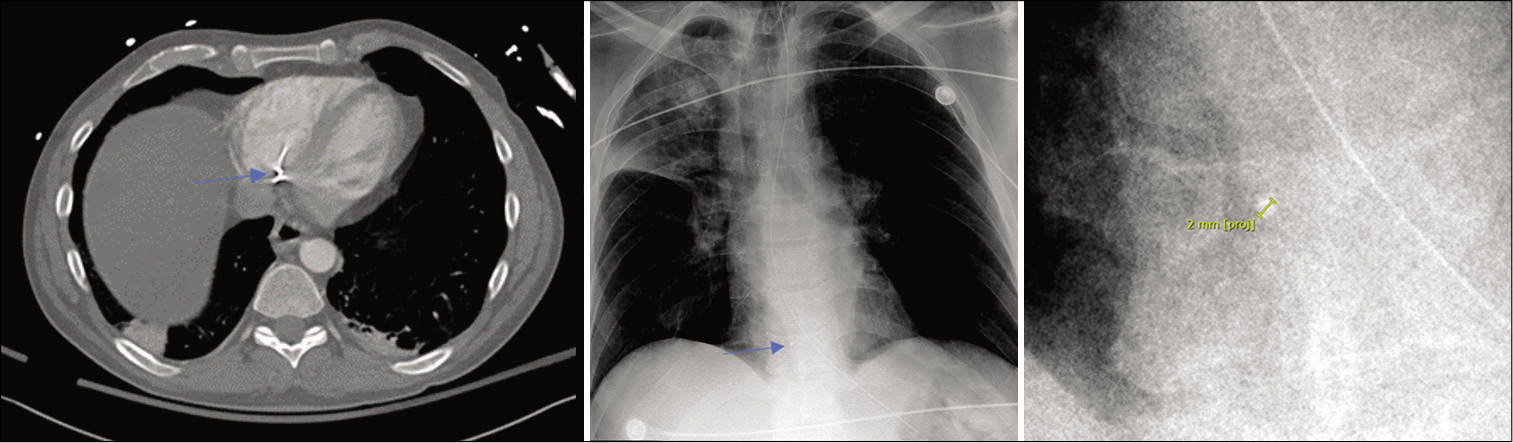
Case Description: A patient presented with a CGI from an occipital trajectory, causing penetrating fragments into the venous sinus system. The weapon was a Glock Model 17M 9 mm with a hollow-point bullet, fired close range. Initial chest X-ray demonstrated only atelectasis. After stabilization, 18 min from the initial chest X-ray, subsequent computed tomography (CT) imaging demonstrated extensive intracranial injuries and fragmentation of the bullet with the expected devastating intracranial injuries. Unexpectedly, chest CT revealed metallic fragments in the right cardiac ventricle which was redemonstrated on follow-up chest X-ray. Unfortunately, his extensive intracranial injuries and poor clinical status were nonsurvivable, and thus the family elected to discontinue supportive measures.
Conclusion: This case demonstrates radiographic imaging of a metallic intravascular fragment from CGI through presumed transvenous mechanisms. The imaging provides a consistent timeline demonstrating migration can occur in the acute phase. This study additionally supports the presumed mechanism for pulmonary of migration through the right heart. Fragment embolization should be considered in cases of acute deterioration in this patient population.
Keywords: Bullet migration, Case report, Craniocerebral gunshot injury, Neurotrauma
INTRODUCTION
Missile embolism was first reported by Thomas Davies in 1834 and later recognized during the Vietnam War as associated with small caliber, slow velocity projectiles penetrating vasculature and fragments becoming emboli. They have been classified as arterial, venous, or paradoxical. Systemic arterial embolus is 80% of reports.[
Bullet-related embolism is rare, with few cases published. Bullet embolism has also been reported from gunshot injures to the lower back,[
The first report of a cranial venous sinus embolus to the heart was reported in 1964. It was treated through craniotomy for control of intracranial hemorrhage and cardiotomy 19 days later for retrieval of the bullet fragment entering the left anterior descending coronary artery.[
Previous reviews suggest that there is a high morbidity rate and that venous extraction may be mandatory.[
CASE REPORT
A middle-aged male presented to the trauma bay with a craniocerebral gunshot injury (CGI). Collateral history revealed a close-range injury from a Glock Model 17M 9 mm hollow-point bullet. Airway was secured with intubation at the scene by the emergency medical service (EMS), but a subsequent air leak necessitated replacement of the endotracheal tube on arrival. Cardiopulmonary resuscitation was ongoing with EMS due to a narrow complex rhythm pulseless electrical activity on scene. Return of spontaneous circulation was achieved with one cycle of epinephrine 1 mg intravenously as per Advanced Cardiac Life Saving guidelines.[
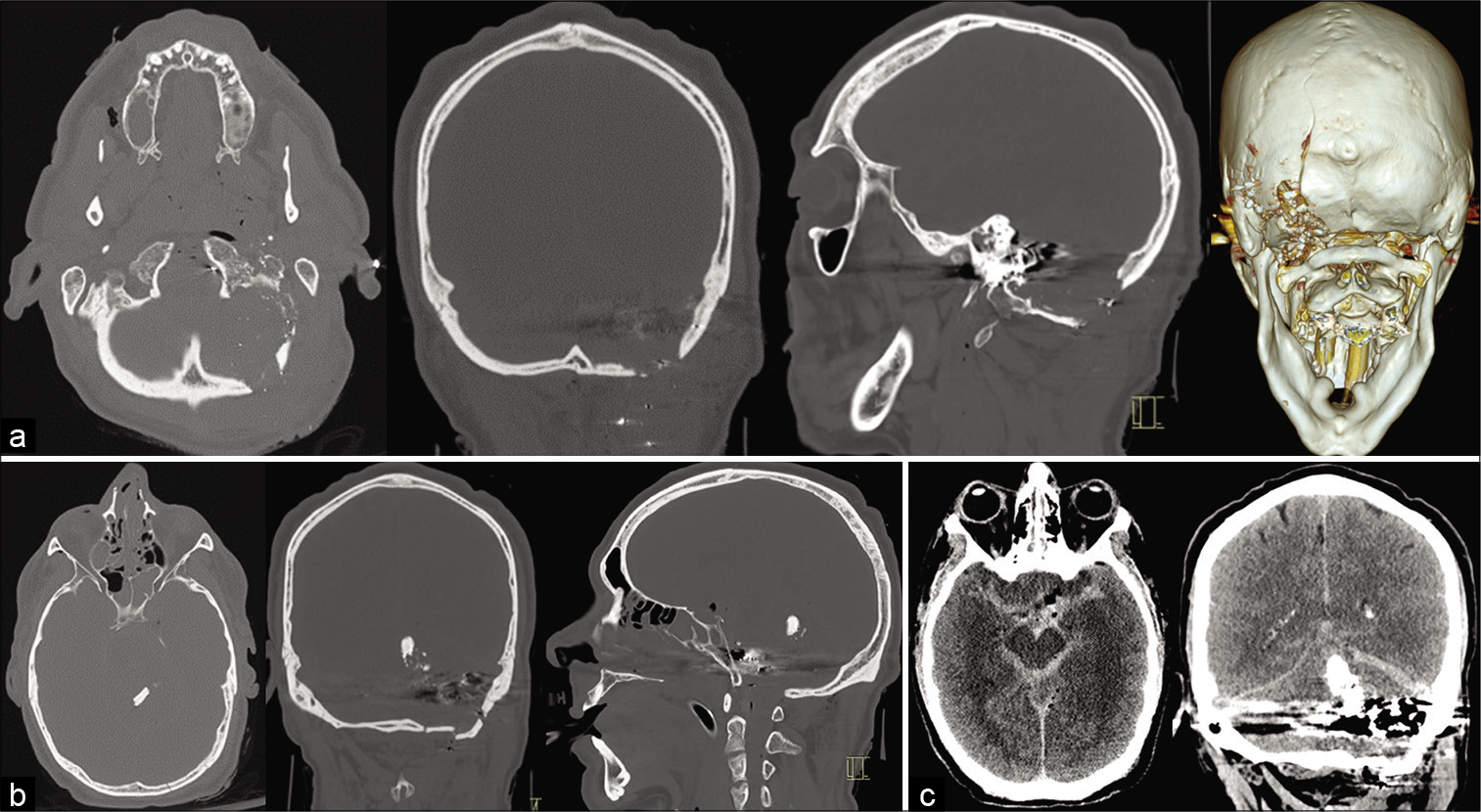
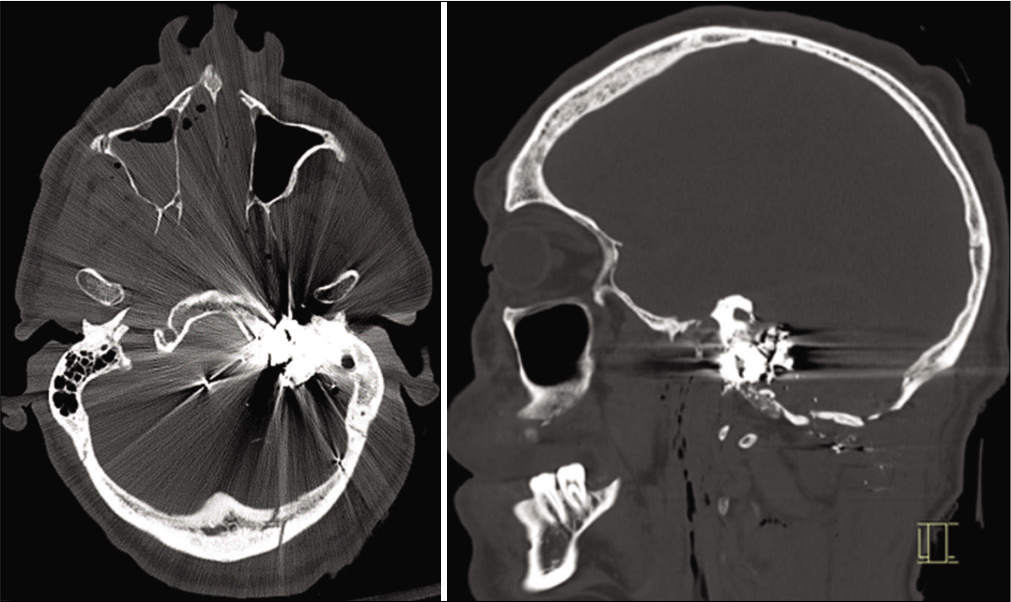
Subsequent computer tomography (CT) scan was performed 18 min after the initial chest X-ray. This included CT of the head, neck, full spine, chest, abdomen, and pelvis as well as CT angiography of the carotids. CT demonstrated penetrating injury to the left occipital bone with comminuted fractures extending to the mastoid temporal bone, right occipital condyle, bilateral carotid canals, and sphenoid sinuses [
Diffuse traumatic subarachnoid hemorrhage, a moderate-volume intraventricular hemorrhage, subdural hemorrhage, epidural hemorrhage, and a 1.5 cm × 0.6 cm × 0.5 cm left lateral pontine intraparenchymal hemorrhage was found [
CT of the chest demonstrated a small metallic fragment within the right ventricle, without any other penetration or associated injuries to the chest or abdomen [
The patient remained at a GCS of 3, with fixed dilated pupils and no brainstem reflexes, including no spontaneous respiratory effort. The extensive nature of his injury was discussed with the family, and a decision was made to pursue supportive end-of-life care without organ donation as consistent with the patient’s previously expressed wishes.
DISCUSSION
This case demonstrates likely migration of a metallic fragment from the CGI through presumed transvenous route to the right cardiac ventricle. Given no dynamic imaging of the process of migration was possible, only serial imaging minutes apart, this study is limited in conclusively stating the path of migration, though a transvenous route through sinus or tributary is the most likely possibility. Although in this case, the patient was clinically neurologically unsalvageable, it demonstrates that migration of fragments may occur in the acute phase. While it is challenging to determine whether this contributed to this young man’s demise, in the context of acute deterioration, an embolism of bullet fragments should be considered. This case adds to other literature demonstrating subacute pulmonary embolism of such fragments by radiographically confirming the interim step of acute emboli in the right ventricle.
The capacity of CGI emboli migrating acutely, as is likely in this case, or in a delayed fashion, as in previous cases, has implications for treatment decisions. When decompressive or other surgery is offered, classical teaching is to avoid pursuing deep intracranial bullet retrieval, though there is no documented evidence addressing this.[
CONCLUSION
Craniocerebral gunshot injures can cause fragmentation of bullet or bone to venous sinuses. Venous sinus injuries have the potential for not only exsanguination but also transvenous migration of embolic material. Bullet fragment-related embolism should be considered on the differential of gunshot patients who have the possibility of venous injury.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. 2. Breeding JM, Smith RS, Dort JM. Bullet embolus to the heart after gunshot wound to the neck: A case report. Am Surg. 2007. 73: 1245-6 3. Carey ME, Young HF, Rish BL, Mathis JL. Follow-up study of 103 American soldiers who sustained a brain wound in Vietnam. J Neurosurg. 1974. 41: 542-9 4. Duke E, Peterson AA, Erly WK. Migrating bullet: A case of a bullet embolism to the pulmonary artery with secondary pulmonary infarction after gunshot wound to the left globe. J Emerg Trauma Shock. 2014. 7: 38-40 5. Goldman RL, Carmody RF. Foreign body pulmonary embolism originating from a gunshot wound to the head. J Trauma. 1984. 24: 277-9 6. Govindaraju RC, Kolwalkar JP. Missile embolism from pulmonary vein to systemic circulation: Case report with systematic literature review. J Emerg Trauma Shock. 2019. 12: 218-21 7. Hammon WM. Analysis of 2187 consecutive penetrating wounds of the brain from Vietnam. J Neurosurg. 1971. 34: 127-31 8. Hiebert CA, Gregory FJ. Bullet embolism from the head to the heart. JAMA. 1974. 229: 442-3 9. Khomenko I, Tsema I, Shklyarevych P, Kravchenko K, Holinko V, Nikolaienko S. Pulmonary artery embolism by a metal fragment after a booby trap explosion in a combat patient injured in the armed conflict in East Ukraine: A case report and review of the literature. J Med Case Rep. 2018. 12: 330 10. Kovalev V, Salaiz OD. Surgical management of a bullet embolism to the pulmonary artery. Cureus. 2020. 12: e8138 11. Loggini A, Vasenina VI, Mansour A, Das P, Horowitz PM, Goldenberg FD. Management of civilians with penetrating brain injury: A systematic review. J Crit Care. 2020. 56: 159-66 12. Miller KR, Benns MV, Sciarretta JD, Harbrecht BG, Ross CB, Franklin GA. The evolving management of venous bullet emboli: A case series and literature review. Injury. 2011. 42: 441-6 13. Nehme AE. Intracranial bullet migrating to pulmonary artery. J Trauma. 1980. 20: 344-6 14. Shannon F, McCroskey B, Moore E, Moore F. Venous bullet embolism: Rationale for mandatory extraction. J Trauma. 1987. 27: 1118-22 15. Siddiqui MI, Hawksworth SA, Sun DY. Removal of migrating lumbar spine bullet: Case report and surgical video. World Neurosurg. 2019. 131: 62-4