- Department of Undergraduate, Faculty of Engineering, Medical School, University Campus Bio-Medico of Rome, England
- Department of Neurosurgery, Manchester Centre of Clinical Neurosciences, Salford, Manchester, England.
Correspondence Address:
Pietro Ivo D’Urso
Department of Neurosurgery, Manchester Centre of Clinical Neurosciences, Salford, Manchester, England.
DOI:10.25259/SNI_609_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marco Manzo, Pietro Ivo D’Urso. Craniocervical junction arachnoid cyst. 28-Feb-2020;11:34
How to cite this URL: Marco Manzo, Pietro Ivo D’Urso. Craniocervical junction arachnoid cyst. 28-Feb-2020;11:34. Available from: https://surgicalneurologyint.com/surgicalint-articles/9882/
Abstract
We report the case of a 33-year-old patient who underwent fenestration of a large symptomatic cranio-cervical junction arachnoid cyst.
Keywords: Arachnoid cyst, Craniocervical junction, Posterior fossa cyst
Arachnoid cysts are relatively common benign cysts of the central nervous system, seldom requiring surgical treatment.
Herein, we present the rare case of a large craniocervical junction arachnoid cyst.
A 33-year-old man presented to the Neurosurgery Clinic with a 2-year history of worsening occipital headaches, triggered by coughing and straining. He reported gradual onset of this symptom without precipitating factors. He denied head injury or history of malignancy and did not suffer sensory-motor symptoms in his limbs nor sphincter disturbance.
On examination, he was neurologically intact and there was no evidence of papilledema at the fundoscopy.
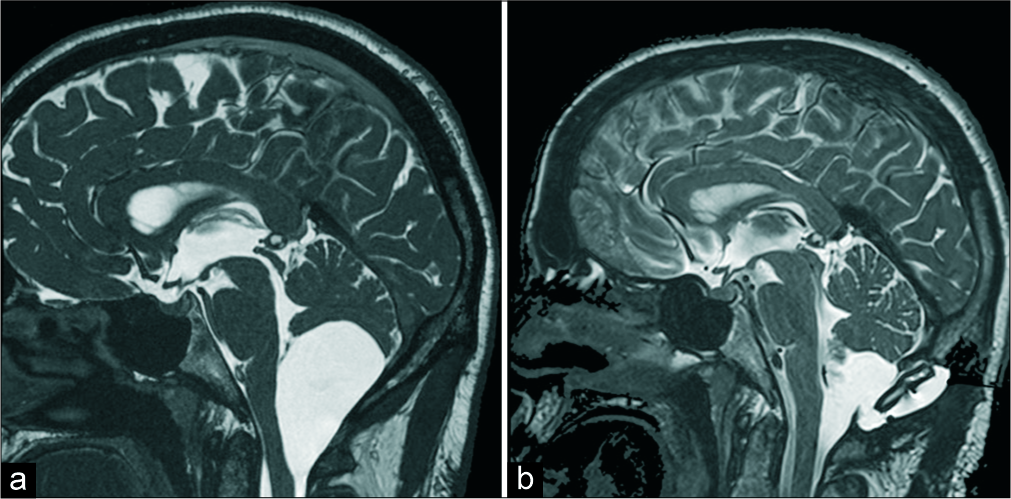
Magnetic resonance imaging (MRI) of the brain revealed a large craniocervical junction cyst with brainstem compression and cerebrospinal fluid (CSF) pathway obstruction [
In view of patient’s symptoms, surgery was felt to be indicated.
A midline posterior fossa craniotomy was carried out and the cyst was drained and widely fenestrated into the surrounding CSF spaces.
Histology was confirmed to be consistent with an arachnoid cyst.
There were no postoperative deficits and the patient was discharged home.
Twelve months following surgery, his headaches had resolved and his MRI showed satisfactory decompression [
We have described the case of a patient with a large craniocervical junction arachnoid cyst, successfully treated surgically.
Arachnoid cysts at the craniocervical junction are extremely rare.[
They can be congenital or acquired. Congenital cysts arise during development from the primitive meninges that surround the neural tube and, although present at birth, they progressively enlarge compressing neural structures and causing symptoms later in life. Acquired cysts can be secondary to head injury, hemorrhage, chemical irritation, meningitis, or tumors.[
The posterior fossa is the second most common site of arachnoid cysts; in fact, 40% of cysts occur in this region. Most posterior fossa arachnoid cysts are diagnosed within the three decades and it is not well understood why they become symptomatic later in life compared with cysts at other sites.[
The natural history of craniocervical junction arachnoid cysts is not well understood. Although many of these cysts are encountered incidentally, they may become symptomatic due to their expansion. Several mechanisms have been proposed to explain the enlargement of arachnoid cysts, and these include active or passive CSF transport through the cyst wall, hydrodynamic effects of the CSF, or a valve mechanism.
The most common presenting symptoms of craniocervical arachnoid cysts are secondary to cerebellar, brainstem or spinal cord compression, or hydrocephalus. In our patient, the cyst was congenital, likely originating from the cisterna magna and extending into the foramen magnum and its expansion has probably caused CSF outflow obstruction, manifesting with worsening cough headache.
Hydrocephalus is a common feature of posterior fossa arachnoid cysts, especially in the midline and mechanical factors explain hydrocephalus in most cases. In our patient, despite the significant compression, no hydrocephalus had developed yet, perhaps due to early detection of the cyst. The optimal treatment for arachnoid cysts has yet to be determined. The most common procedures are microsurgical or endoscopic fenestration of the cysts, resection, or shunt placements. While in the past shunting was the most common and accepted procedure, due to the high rates of complications, shunts for arachnoid cysts are currently less commonly carried out and reserved in case of failure of microsurgical or endoscopic techniques. Indeed microscopic or endoscopic techniques are nowadays the most favorite treatment options. In a large microsurgery series, 82% of patients improved and 5% worsened and complications rates were 17%, whereas 7% of patients suffered a recurrence warranting additional intervention.[
In our case, we opted for a wide microsurgical fenestration and intraoperatively we felt that complete resection of the cyst wall could have carried a risk of damaging the pia of the posterior medulla and dorsal upper cord.
Despite the benign natural course of these cysts, recurrence can occur even several years following surgery.
It is still matter of debate whether a complete excision rather than a simple fenestration should be achieved. In our experience, a wide fenestration offers satisfactory clinical results, with minimal risks of morbidity, and in our opinion, both microsurgical and endoscopic techniques are valuable treatment options.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bhatia S, Thakur RC, Devi BI, Radotra BD, Kak VK. Craniospinal intradural arachnoid cyst. Postgrad Med J. 1992. 68: 829-30
2. Fukushima Y, Sato M, Taguchi J, Sasaki M, Kanai N, Hayakawa T. Craniospinal arachnoid cyst: Case report. No Shinkei Geka. 1996. 24: 75-9
3. Helland CA, Wester K. A population based study of intracranial arachnoid cysts: Clinical and neuroimaging outcomes following surgical cyst decompression in adults. J Neurol Neurosurg Psychiatry. 2007. 78: 1129-35
4. Karabatsou K, Hayhurst C, Buxton N, O’Brien DF, Mallucci CL. Endoscopic management of arachnoid cysts: An advancing technique. J Neurosurg. 2007. 106: 455-62
5. Kuroiwa T, Takeuchi E, Yamada K, Ohta T, Miyaji Y, Onomura T. An intradural arachnoid cyst of the craniovertebral junction; a case report. No Shinkei Geka. 1991. 19: 1097-9
6. Price SJ, David KM, O’Donovan DG, Aspoas AR. Arachnoid cyst of the craniocervical junction: Case report. Neurosurgery. 2001. 49: 212-5
7. Shukla R, Sharma A, Vatsal DK. Posterior fossa arachnoid cyst presenting as high cervical cord compression. Br J Neurosurg. 1998. 12: 271-3
8. Takanashi Y, Mochimatsu Y, Shyudo T, Yamamoto I. A case report of an arachnoid cyst in the craniovertebral junction. No To Shinkei. 1995. 47: 68-70