- Department of Neurosurgery, Apollo Hospital, Bhubaneswar, Odisha, India
- Department of Orthopaedics, Apollo Hospital, Bhubaneswar, Odisha, India
Correspondence Address:
Biswaranjan Nayak
Department of Neurosurgery, Apollo Hospital, Bhubaneswar, Odisha, India
DOI:10.4103/2152-7806.159835
Copyright: © 2015 Nayak B. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Nayak B, Patnaik S, Sahoo PK, Biswal D. Craniocervical junction tuberculosis: Usual pathology at an unusual site. Surg Neurol Int 02-Jul-2015;6:115
How to cite this URL: Nayak B, Patnaik S, Sahoo PK, Biswal D. Craniocervical junction tuberculosis: Usual pathology at an unusual site. Surg Neurol Int 02-Jul-2015;6:115. Available from: http://surgicalneurologyint.com/surgicalint_articles/craniocervical-junction-tuberculosis-usual-pathology-at-an-unusual-site/
Abstract
Background:Tuberculosis (TB) of the craniocervical junction is rare even where the condition is endemic. It poses problems in both diagnosis and management if not managed in time it may cause life-threatening complications.
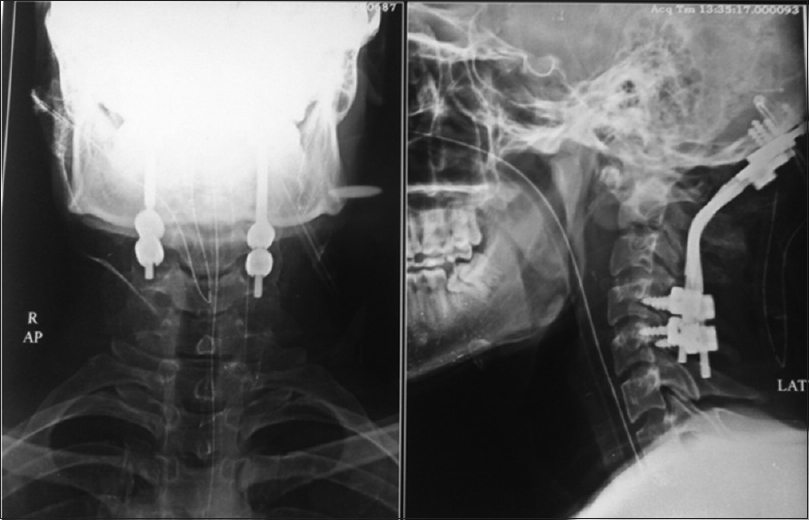
Case Description:An 18-year-old male patient presented with pain in the nape of the neck since 12 months duration which was not improving with medication. After magnetic resonance imaging of cervical spine, he was diagnosed as craniocervical junction TB. We did a transoral decompression of abscess with biopsy along with posterior decompression of cord and occipitocervical fusion. Biopsy of pathological material came as TB. He was advised for anti-tubercular therapy for 18 months.
Conclusion:Although craniocervical junction TB is a rare disease, the outcome of treatment is good. Antituberculous drug therapy remains the mainstay of treatment after confirming the diagnosis. The surgical management options include transoral decompression with or without posterior fusion, depending upon the presence and persistence of atlantoaxial instability.
Keywords: Craniocervical junction, posterior fusion, transoral decompression, tuberculosis
INTRODUCTION
Tuberculosis (TB) is a worldwide health problem, according to the World Health Organization it is the leading infectious cause of mortality worldwide killing 1.45 million people.[
CASE REPORT
An 18-year-old male patient presented with pain in the nape of the neck since 12 months duration which was not improving with medication. The patient had stiffness of the neck with decreased range of movement in all directions. Routine hematological investigations were within the normal limit, and he was screened for rheumatologic problems without revealing any pathology. On magnetic resonance imaging of cervical spine [
DISCUSSION
The occipitocervical junction, a transitional zone between the skull and the spinal column, serves as the most mobile part of the axial skeleton. Bony abnormalities affecting this complex results in dysfunction of the neural structures by compression along the entire circumference, altering the arterial supply, venous drainage, and changing the cerebrospinal fluid dynamics.
Lymphatic channels play a dominant role in the etiopathogenesis of any infective process at the craniovertebral junction (CVJ). The infection probably begins in the retropharyngeal space with secondary involvement of bone, and is rarely primarily in the bone itself. Progression of the disease causes increasing ligamentous involvement, and the later stages involve increased destruction of bone.[
The lateral masses are the initial to be affected, and destruction of these will eventually lead to collapse or weakening of the bony pillars. Depending on the severity of the disease process, varying degree of bony destruction of the atlas may ensue. This bony destruction may manifest as neck pain, torticollis, occipital neuralgia, dysphagia, dyspnea (retropharyngeal abscess) or even as neurologic dysfunction.[
At this stage, the disease if unabated will cause ligament destruction aggravating the instability at the CVJ. Atlanto-axial dislocation (AAD) may result and if the prodens interval is more than 5 mm, it signifies the destruction of the transverse ligament of the atlas. Varying degree of rotatory malalignment is commonly associated and needs to be considered during treatment of the condition.
It is very unusual to find the disease advanced to the stage of complete liquefaction and dissolution of the atlas. When this occurs (as in our case), the instability at the CVJ is severe and demands urgent immobilization. It also forewarns complete osteoligamentous destruction and warrants emergency management. The associated problems of pressure such as dysphagia and asphyxia may assume alarming proportions. This may as in our case necessitate tracheostomy for effective airway ventilation.
As a sequelae, secondary basilar invagination may occur adding a different clinical dimension to the disease. An occipital bone may be involved as an extension of the disease with softening allowing the spinal column to further telescope into the posterior fossa. The proximity of the lower cranial nerves makes them vulnerable to be affected.
Conservative management for postinfective AAD,[
CONCLUSION
Although CVJ TB is a rare disease, the outcome of treatment is good. Antituberculous drug therapy remains the mainstay of treatment after confirming the diagnosis. The surgical management options include transoral decompression with or without posterior fusion, depending upon the presence and persistence of atlantoaxial instability.
References
1. Bhojraj SY, Shetty N, Shah PJ. Tuberculosis of the craniocervical junction. J Bone Joint Surg Br. 2001. 83: 222-5
2. Buxi TB, Sud S, Vohra R. CT and MRI in the diagnosis of tuberculosis. Indian J Pediatr. 2002. 69: 965-72
3. De Oliveira E, Rhoton AL, Peace D. Microsurgical anatomy of the region of the foramen magnum. Surg Neurol. 1985. 24: 293-352
4. Fang D, Leong JC, Fang HS. Tuberculosis of the upper cervical spine. J Bone Joint Surg Br. 1983. 65: 47-50
5. Kanaan IU, Ellis M, Safi T, Al Kawi MZ, Coates R. Craniocervical junction tuberculosis: A rare but dangerous disease. Surg Neurol. 1999. 51: 21-5
6. Lifeso R. Atlanto-axial tuberculosis in adults. J Bone Joint Surg Br. 1987. 69: 183-7
7. Michie I, Clark M. Neurological syndromes associated with cervical and craniocervical anomalies. Arch Neurol. 1968. 18: 241-7
8. Nicholson JT, Sherk HH. Anomalies of the occipitocervical articulation. J Bone Joint Surg Am. 1968. 50: 295-304
9. Pandya SK. Tuberculous atlanto-axial dislocation (with remarks on the mechanism of dislocation). Neurol India. 1971. 19: 116-21
10. Parke WW, Rothman RH, Brown MD. The pharyngovertebral veins: An anatomical rationale for Grisel's syndrome. J Bone Joint Surg Am. 1984. 66: 568-74
11. Tuli SM. Tuberculosis of the craniovertebral region. Clin Orthop Relat Res. 1974. 104: 209-12
12. Watson Jones R. Spontaneous hyperaemic dislocation of the atlas. Lancet. 1932. 25: 586-
13. . Available from: http://www.who.int/tb/publications/global_report/2011/gtbr11_full.pdf .