- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
- Department of Neurology, Imari Arita Kyoritsu Hospital, Arita, Japan.
- Department of Neurosurgery, Imari Arita Kyoritsu Hospital, Arita, Japan.
- Department of Neurosurgery, Shiroishi Kyoritsu Hospital, Shiroishi, Japan.
Correspondence Address:
Tatsuya Tanaka, Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita, Japan.
DOI:10.25259/SNI_978_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Tanaka1, Hirofumi Goto2, Nobuaki Momozaki3, Eiichiro Honda4. Creating of “fascial sheath” around subcutaneous lumboperitoneal shunt catheters largely prevents postoperative subcutaneous shunt catheter migration. 11-Nov-2022;13:528
How to cite this URL: Tatsuya Tanaka1, Hirofumi Goto2, Nobuaki Momozaki3, Eiichiro Honda4. Creating of “fascial sheath” around subcutaneous lumboperitoneal shunt catheters largely prevents postoperative subcutaneous shunt catheter migration. 11-Nov-2022;13:528. Available from: https://surgicalneurologyint.com/surgicalint-articles/11988/
Abstract
Background: Spinal catheter migration into the subcutaneous tissue is common after lumboperitoneal shunt (LPS) placement. This study proposed a new method (i.e., wrapping fascia around the catheter like a sheath) to prevent LPS spinal catheter migration.
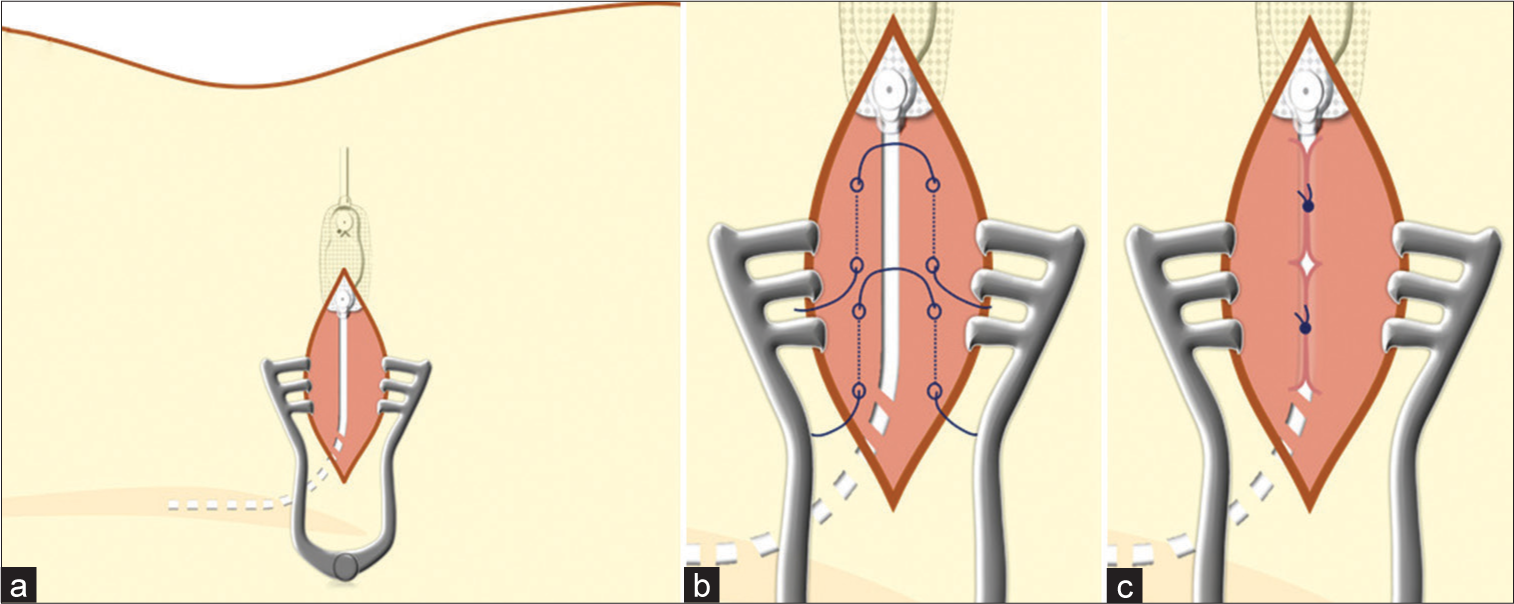
Methods: After a LPS spinal catheter was inserted under routine fluoroscopic guidance, and the paravertebral muscle fascia was closed, the fascia was sutured to wrap the catheter like a sheath using intermittent sutures.
Results: Before the introduction of this technique, the rate of LPS spinal catheter subcutaneous migration was 4.6%. In this study, following LPS shunt placement in 18 consecutive patients with normal pressure hydrocephalus, no further spinal catheter migrations were observed.
Conclusion: This novel method of “wrapping the LPS catheter with intermittent suture like a sheath” was found to be safe and effective for preventing further spinal catheter subcutaneous migration.
Keywords: Complication, Lumboperitoneal shunt, Normal pressure hydrocephalus, Spinal catheter, Subcutaneous migration
INTRODUCTION
A recent randomized and controlled trial reported that lumboperitoneal shunt (LPS) placement can be beneficial for patients with idiopathic normal pressure hydrocephalus (iNPH).[
Here, we introduce a novel method of wrapping the subcutaneous shunt catheter with intermittent fascial sutures to create a protective “sheath” for preventing LPS shunt migration.
MATERIALS AND METHODS
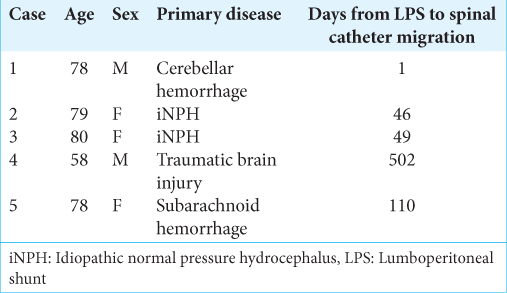
Overall, 18 consecutive patients underwent LPS placement for iNPH through our modified technique between 2018 and 2019. Based on our previous experience, LPS spinal catheter subcutaneous migration occurred in 4.6% of cases (five of 107 patients; 2011–2017) [
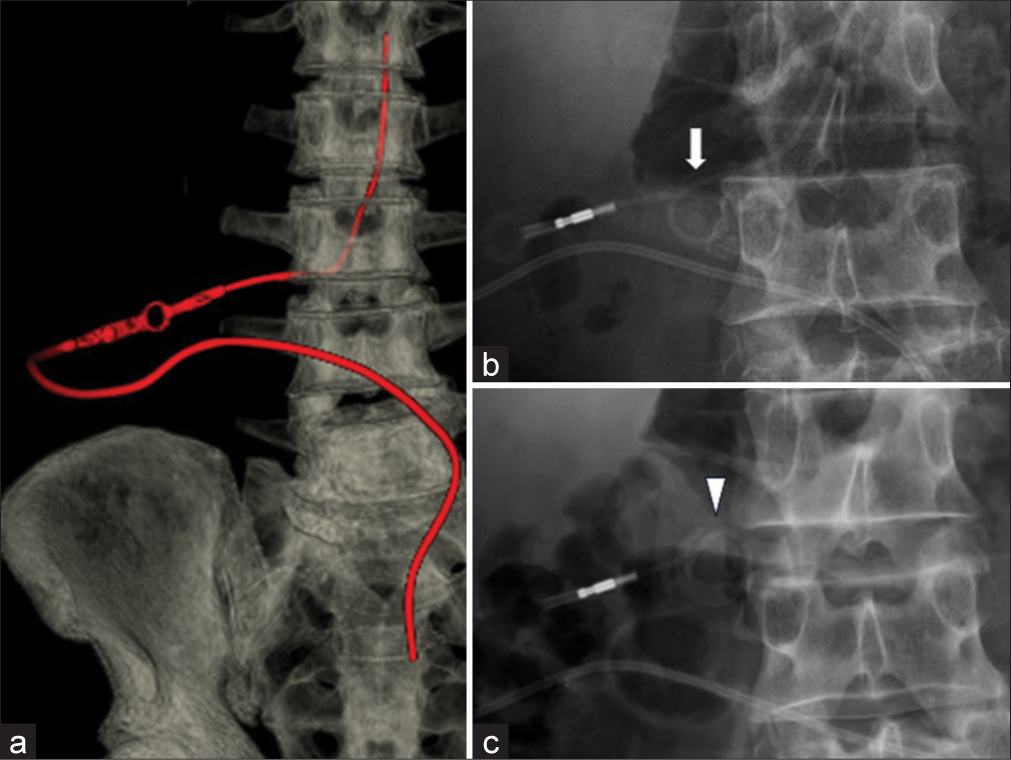
Figure 1:
Case 4 - Postoperative three-dimensional computed tomography on day 50 shows correct placement of the spinal catheter (a). Postoperative anterior-posterior (AP) radiograph on day 295 shows catheter migration (b, arrow). Postoperative AP radiograph on day 502 shows catheter coiling (c, arrowhead).
Preoperative clinical data
Overall, 10 enrolled patients were females and eight were males, and the mean age of the participants was 73.6 (45–85) years. Of these, 12, four, one, and one patients presented with iNPH, communicating hydrocephalus after subarachnoid hemorrhage, communicating hydrocephalus caused by dural arteriovenous fistula, and communicating hydrocephalus after head trauma.
RESULTS
No spinal catheter-related complications were observed after the use of our method.
DISCUSSION
Spinal catheter migration after LPS placement for NPH is a common complication occurring in 4.6% of patients based on our previous experience and 1.1–1.9% of patients according to the relevant literature.[
Our modified technique allows for the correct placement of the spinal catheter under fluoroscopic guidance to avoid the direct ejection force due to hyperflexion exerted on the catheter. In addition, we can minimize excessive dissection of the subcutaneous tissue, thereby reducing dead space and better anchoring the catheter to the paravertebral muscle/ fascia using a protective sheath (i.e., interrupted sutures in the fascia) around the catheter itself.[
Notably, after the use of this modified “sheath technique” after LPS shunt placement in 18 consecutive patients with NPH, no further spinal catheter migrations were observed.
CONCLUSION
We created a sheath around subcutaneous LPS spinal catheters for patients with NPH, and this prevented spinal catheter subcutaneous migration in the present case series.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Kawahara T, Tokimura H, Higa N, Hirano H, Bohara M, Hanaya R. Surgical technique for preventing subcutaneous migration of distal lumboperitoneal shunt catheters. Innov Neurosurg. 2013. 1: 169-72
2. Kazui H, Miyajima M, Mori E, Ishikawa M, SINPHONI-2 Investigators. Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): An open-label randomised trial. Lancet Neurol. 2015. 14: 585-94
3. Tanaka T, Goto H, Momozaki N, Honda E. Incidence of radiculopathy following lumboperitoneal shunt placement without fluoroscopy for normal pressure hydrocephalus. Surg Neurol Int. 2022. 13: 437
4. Tucker A, Kajimoto Y, Ohmura T, Ikeda N, Furuse M, Nonoguchi N. Fluoroscopic-guided paramedian approach for lumbar catheter placement in cerebrospinal fluid shunting: Assessment of safety and accuracy. Oper Neurosurg (Hagerstown). 2019. 16: 471-7