- Department of Neurosurgery, Hôpitaux Universitaires de Marseille Nord, Aix Marseille University, Marseille, France,
- Department of Neurosurgery, Tanta University, Tanta, Gharbeya, Egypt.
Correspondence Address:
Hussein Hamdi, Department of Neurosurgery, Tanta University, Tanta, Gharbeya, Egypt.
DOI:10.25259/SNI_375_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Talal Al-Shabibi1, Hussein Hamdi2, Ahmed Balaha2, Yasser Ghoraba2, Jean-Marc Kaya1. Delayed Collet-Sicard syndrome after internal carotid dissection and Jefferson fracture. Case report and Review of Literature. 27-Jul-2021;12:374
How to cite this URL: Talal Al-Shabibi1, Hussein Hamdi2, Ahmed Balaha2, Yasser Ghoraba2, Jean-Marc Kaya1. Delayed Collet-Sicard syndrome after internal carotid dissection and Jefferson fracture. Case report and Review of Literature. 27-Jul-2021;12:374. Available from: https://surgicalneurologyint.com/surgicalint-articles/10999/
Abstract
Background: Lower cranial nerve palsies, or Collet-Sicard syndrome, can be caused by many different etiologies including head trauma, basilar occipital fractures, tumors, and interventions. Few reports describe different presentations of this condition, and we present here a case study to increase awareness of and add to the variable spectrum.
Case Description: A 56-year-old who had been hit while diving was admitted to our department. On examination, he was conscious without any signs of lateralization but presented with severe neck pain. CT brain and cervical spine revealed a C1 fracture with bilateral symmetrical fracture of the anterior and posterior arches (Jefferson’s fracture) and slight bilateral joint dislocation C1-C2 discreetly predominant on the left. One week later, he presented with dysarthria, dysphonia, swallowing disorder, anisocoria, tongue deviation, and palate deviation (XII, IX, and X). CT Angiography showed dissection of the internal carotid artery immediately after the carotid bulb. He has been treated conservatively with curative anticoagulants with stable symptoms. No surgical intervention had been proposed.
Conclusion: Adding to the literature, delayed Collet-Sicard syndrome and lower cranial affection can be caused by missed carotid wall hematoma following severe craniocervical trauma associated with Jefferson’s fracture.
Keywords: Collet-Sicard syndrome, Injury, Internal carotid dissection, Jefferson fracture, Lower cranial nerves
INTRODUCTION
In 1915, Frederic Collet[
Very few reports in the literature are describing the situation with different presentations. Usually, the symptoms and signs are dramatic and presented soon after trauma. Consequences of intracranial or even extracranial events can contribute to nerve affection mechanisms and subsequent manifestations such as bulbar palsy, motor, sensory deficits, dysphagia, or dysphonia.[
Each single case study could add to the spectrum of this rare presentation. Some patients were treated conservatively with very good outcome and recovery or stable clinical course.[
We present here a unique case of Jefferson fracture C1 with internal carotid dissection (ICD) causing delayed lower cranial nerve affection to add to the spectrum in the literature.
CASE DESCRIPTION
A 56-year-old male had been hit while diving in a swimming pool and presented with severe post-traumatic cervical pain, with active and passive movements. On clinical examination, he was conscious and oriented without any signs of lateralization. In addition, there was no motor or sensory deficit.
X-ray cervical spine did not show any abnormalities. Computed tomography (CT) of the brain and cervical spine study showed C1 fracture; bilateral symmetrical fracture of the anterior and posterior arches of C1 (Jefferson’s fracture) with slight bilateral joint dislocation C1-C2 discreetly predominant on the left. Spine magnetic resonance imaging (MRI) showed straightness of the cervical spine, and no disturbance of the coronal statics, and no constitutional cervical ductal stenosis as a secondary stenosis. No abnormality of the medullary signal as well as paraspinal soft tissue. Cervical angioscan was not done in the first admission.
On admission, the patient was managed conservatively in the form of anxiolytics, calcium channel inhibitors, and strong opioid analgesics. No surgical intervention was required, and the clinical situation remained stable with pain improvement.
Patient was discharged 2 days after admission on conservative treatment and neck collar.
One week later, he presented with mild complaints of dysarthria, dysphagia, and dysphonia. Clinical examination found no deficit except deviated tongue and palate, without ptosis or anhydrosis. Normal blood pressure and oxygen saturation, but sinus bradycardia were observed and required intensive care unit admission.
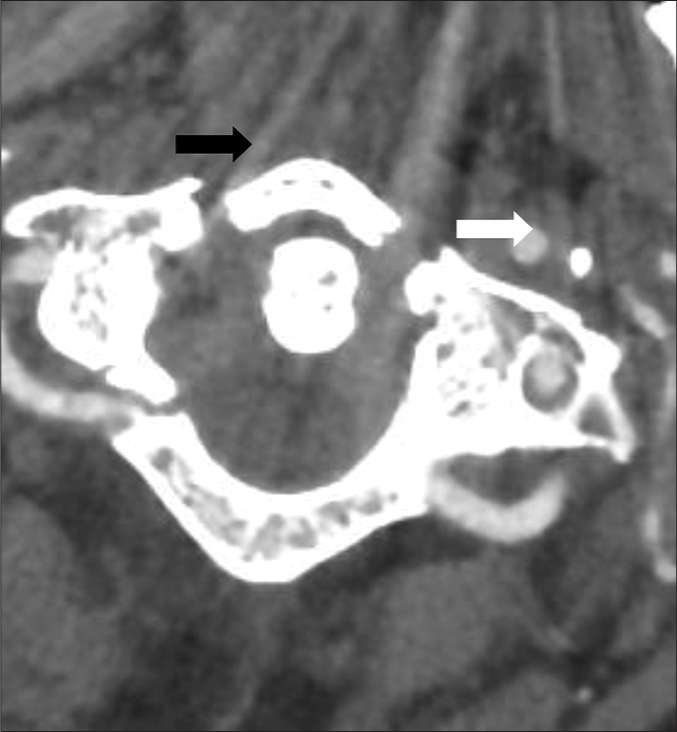
CT angiography showed right internal carotid artery occlusive dissection and carotid wall hematoma just above the carotid bulb [
The patient was observed in the ICU for a few days before he was discharged to the service. Introduction of curative anticoagulant was conducted. No surgical intervention had been proposed. The patient remains stable.
DISCUSSION
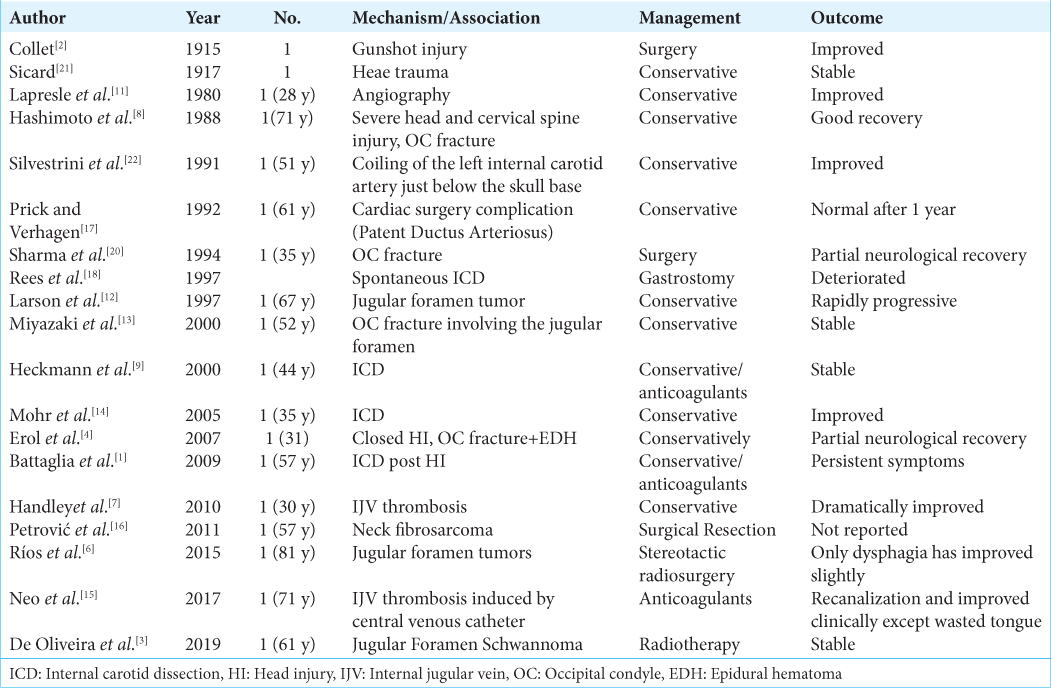
Lower cranial nerves affection could be caused directly or indirectly by several mechanisms following different causes as shown in [
Internal carotid artery dissection and occlusion are reported following different ways of cervical and head trauma.[
The wide spectrum of etiologies, mechanism, clinical presentation, and outcome has been reported through few case reports. High-resolution imaging studies are required to precisely define the mechanism of the conditions and degree of affection. Craniocervical CT and MRI are routinely used in the reported cases, but angiography is not routinely required.[
Different management strategies can be applied including conservative and surgical intervention depending on the primary etiology. Moreover, with conservative treatments, outcome varies from good recovery[
Spontaneous internal carotid artery dissection has been reported with headache, neck pain, and Horner syndrome.[
CONCLUSION
Adding to the literature, delayed Collet-Sicard syndrome and lower cranial affection can be caused by carotid wall hematoma following severe craniocervical trauma associated with Jefferson’s fracture.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
The authors have nothing to declare regarding the finiancial support and sponsorship.
Conflicts of interest
There are no conflicts of interest.
References
1. Battaglia F, Martini L, Tannier C. Syndrome de ColletSicard après dissection carotidienne. Rev Neurol (Paris). 2009. 165: 588-90
2. Collet F. Sur un nouveau syndrome paralytique pharyngolarynge par blessure de guerre. Lyon Med. 1915. 124: 121-9
3. de Oliveira IA, Cordeiro BM, Coelho RD, de Sousa AF, Barros YC, Teixeira KI. Collet-Sicard syndrome: Case report. Curr Res Integr Med. 2019. 4: 16-8
4. Erol FS, Topsakal C, Kaplan M, Yıldırım H, Ozveren MF. Collet-Sicard syndrome associated with occipital condyle fracture and epidural hematoma. Yonsei Med J. 2007. 48: 120-3
5. Grundy DJ, McSweeney T, Jones HW. Cranial nerve palsies in cervical injuries. Spine (Phila Pa 1976). 1984. 9: 339-43
6. Gutierrez Rios R, Castrillo Sanz A, Gil Polo C, Zamora Garcia MI, Morollon Sanchez-Mateos N, Mendoza Rodriguez A. Collet-Sicard syndrome. Neurologia. 2015. 30: 130-2
7. Handley TP, Miah MS, Majumdar S, Hussain SS. Collet-sicard syndrome from thrombosis of the sigmoid-jugular complex: A case report and review of the literature. Int J Otolaryngol. 2010. 2010: 203587
8. Hashimoto T, Watanabe O, Takase M, Koniyama J, Kobota M. Collet-Sicard syndrome after minor head trauma. Neurosurgery. 1988. 23: 367-70
9. Heckmann JG, Tomandl B, Duhm C, Stefan H, Neundörfer B. Collet-Sicard syndrome due to coiling and dissection of the internal carotid artery. Cerebrovasc Dis. 2000. 10: 487-8
10. Holyst J. Internal carotid artery occlusion due to intraoral trauma. Acta Neurochir (Wien). 1976. 33: 325-9
11. Lapresle J, Lasjaunias P, Thévenier D. Transitory paralysis of cranial nerves IX, X and XII as well as the left VII after angiography. Contribution to the ischemic pathology of the cranial nerves. Rev Neurol (Paris). 1980. 136: 787-91
12. Larson WL, Beydoun A, Albers JW, Wald JJ. Collet-Sicard syndrome mimicking neuralgic amyotrophy. Muscle Nerve. 1997. 20: 1173-7
13. Miyazaki C, Katsume M, Yamazaki T, Aoki K, Kuroki T, Takasu N. Unusual occipital condyle fracture with multiple nerve palsies and Wallenberg syndrome. Clin Neurol Neurosurg. 2000. 102: 255-8
14. Mohr A, Ebert S, Knauth M. Spontaneous dissection of the internal carotid artery with ipsilateral Collet-Sicard syndrome. Rofo. 2006. 178: 444-6
15. Neo S, Lee KE. Collet-Sicard syndrome: A rare but important presentation of internal jugular vein thrombosis. Pract Neurol. 2017. 17: 63-5
16. Petrović S, Grozdanović D, Kovačević P, Višnjić M, Petrović D. Collet Sicard syndrome as atypical presentation of neck fibrosarcoma: A case report. Bosn J Basic Med Sci. 2011. 11: 137-40
17. Prick MJ, Verhagen WI. The Collet-Sicard syndrome as a complication of cardiovascular surgery. J Neurol Neurosurg Psychiatry. 1992. 55: 741
18. Rees JH, Valentine AR, Llewelyn JG. Spontaneous bilateral carotid and vertebral artery dissection presenting as a ColletSicard syndrome. Br J Radiol. 1997. 70: 856-8
19. Schneider RC, Lemmen LJ. Traumatic internal carotid artery thrombosis secondary to nonpenetrating injuries to the neck; a problem in the differential diagnosis of craniocerebral trauma. J Neurosurg. 1952. 9: 495-507
20. Sharma BS, Mahajan RK, Bhatia S, Khosla VK. Collet-Sicard syndrome after closed head injury. Clin Neurol Neurosurg. 1994. 96: 197-8
21. Sicard JA. Syndrome du carrefour condylodechire posterieur (type pur de paralysie laryngee associee). Marseille Med. 1917. 53: 383
22. Silvestrini M, Floris R, Tagliati M, Stanzione P, Simonetti G. Collet-Sicard syndrome caused by a coiling of the internal carotid artery. Riv Neurol. 1991. 61: 135-6