- Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
Correspondence Address:
Masanori Kinosada, Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
DOI:10.25259/SNI_27_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masanori Kinosada, Hiroyuki Ikeda, Takumi Morita, Makoto Wada, Minami Uezato, Yoshitaka Kurosaki, Masaki Chin. Dilation of proximal internal carotid artery collapse due to severe distal stenosis after angioplasty for distal stenosis: A case report. 24-Feb-2023;14:75
How to cite this URL: Masanori Kinosada, Hiroyuki Ikeda, Takumi Morita, Makoto Wada, Minami Uezato, Yoshitaka Kurosaki, Masaki Chin. Dilation of proximal internal carotid artery collapse due to severe distal stenosis after angioplasty for distal stenosis: A case report. 24-Feb-2023;14:75. Available from: https://surgicalneurologyint.com/surgicalint-articles/12163/
Abstract
Background: We report a case of proximal internal carotid artery (ICA) collapse due to severe distal stenosis that dilated after angioplasty for distal stenosis.
Case Description: A 69-year-old woman underwent thrombectomy for the left ICA occlusion due to stenosis of C3 portion and was discharged home with a modified Rankin Scale score of 0. One year later, she developed cerebral infarction due to progressive stenosis of the C3 portion of the left ICA with proximal ICA collapse and underwent emergency percutaneous transluminal angioplasty (PTA) for distal stenosis. Device guidance to the stenosis was difficult due to proximal ICA collapse. After PTA, blood flow in the left ICA increased, and proximal ICA collapse dilated over time. Due to severe residual stenosis, she underwent more aggressive PTA followed by Wingspan stenting. Device guidance to the residual stenosis was facilitated because proximal ICA collapse had already dilated. Six months later, proximal ICA collapse further dilated.
Conclusion: PTA for severe distal stenosis with proximal ICA collapse may result in dilation of proximal ICA collapse over time.
Keywords: Dilation, Distal stenosis, Percutaneous transluminal angioplasty, Proximal collapse, Wingspan
INTRODUCTION
Carotid artery near-occlusion is a condition, in which blood flow to the distal internal carotid artery (ICA) is reduced due to severe stenosis of the proximal ICA, resulting in collapse of the ICA distal to the stenosis, and narrowing of the vessel diameter.[
CASE REPORT
Patient
A 69-year-old woman.
Present illness
One year before, the patient presented with the right upper and lower extremity paralysis. The National Institutes of Health Stroke Scale (NIHSS) score was 10, and the Alberta stroke program early computed tomography (CT) score was also 10. Computed tomography-angiography (CTA) showed left ICA occlusion [
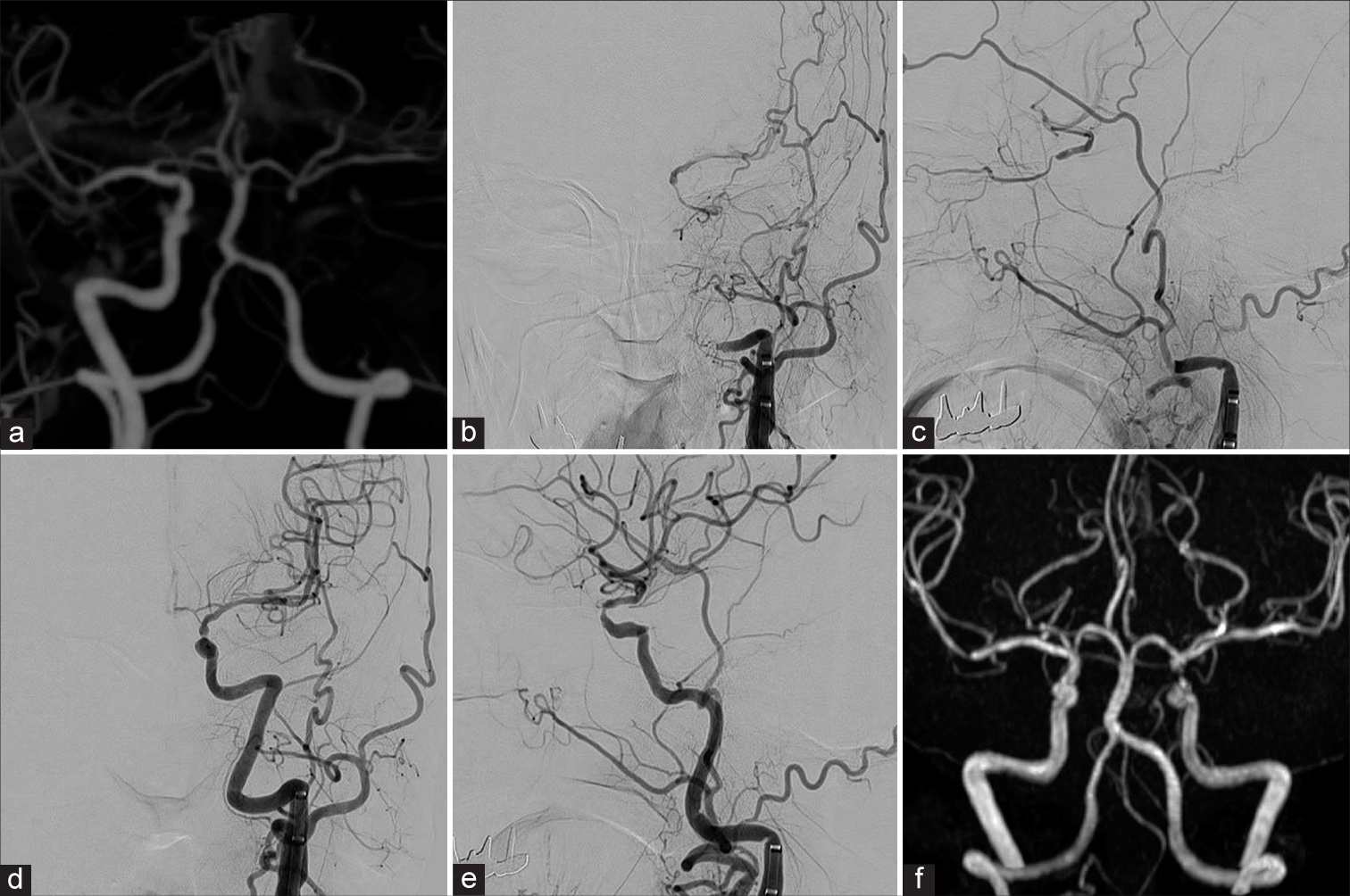
Figure 1:
Perioperative images of thrombectomy performed 1-year ago. (a) Preoperative CTA showing left ICA occlusion. (b and c) Preoperative angiography showing occlusion of the left ICA and collateral vessels in the C2 portion of the ICA from the external carotid artery and ophthalmic artery to the distal ICA (b: frontal view, c: lateral view). (d and e) Postoperative angiography showing TICI 2b recanalization and WASID 68% stenosis in the C3 portion of the left ICA (d: frontal view, e: lateral view). (f) Magnetic resonance angiography the day after thrombectomy showing the patency of the left ICA. ICA: Internal carotid artery, TICI: Thrombolysis in cerebral infarction, WASID: Warfarin-aspirin symptomatic intracranial disease.
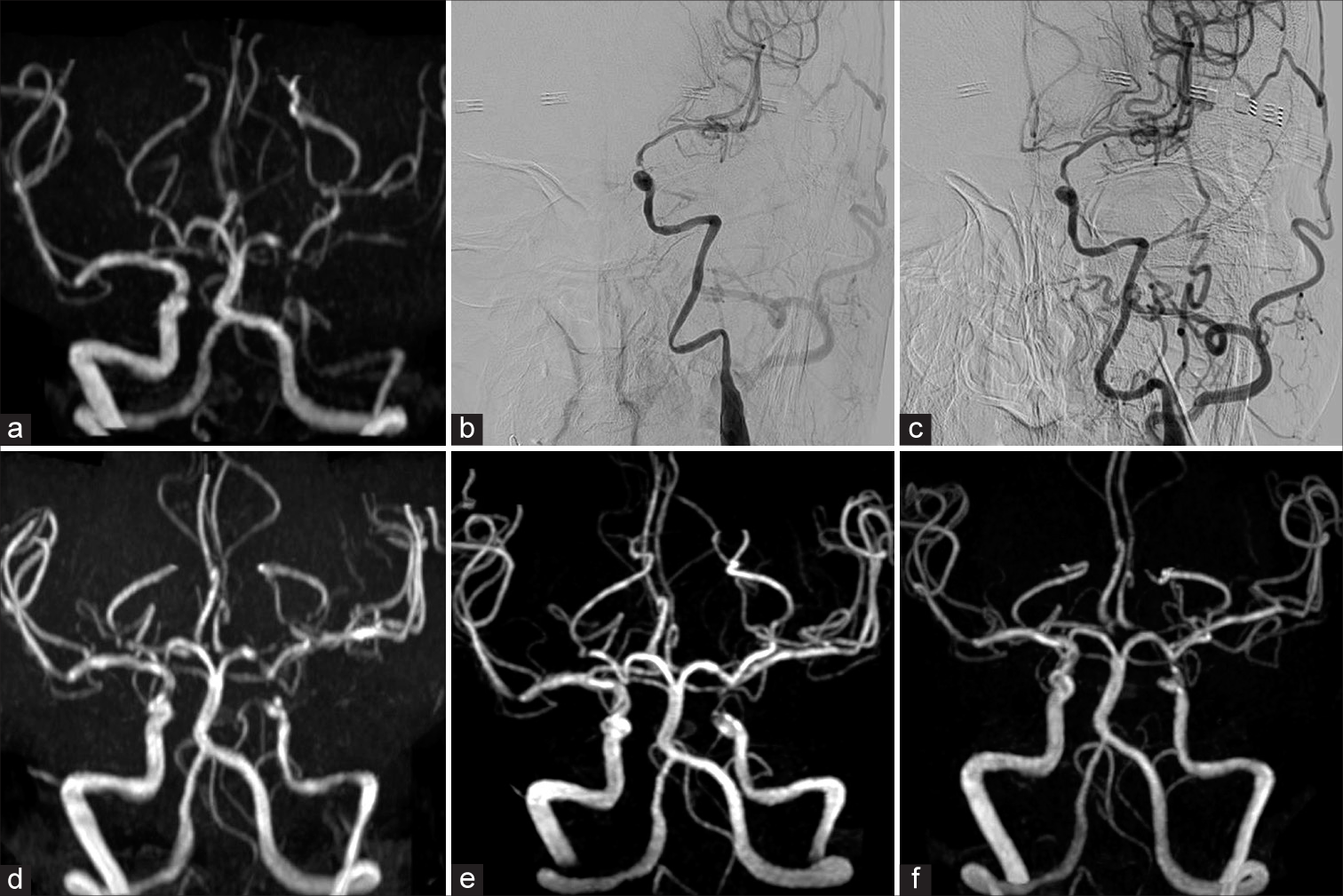
Figure 2:
Perioperative images of initial percutaneous transluminal angioplasty. (a) Preoperative MRA showing reduced blood flow signals in the left ICA and left MCA. (b) Preoperative angiography showing severe stenosis of WASID 92% in the C3 portion of the left ICA with proximal ICA collapse and blood flow delay in the left MCA region. (c) Postoperative angiography showing dilatation of the stenosis (WASID 71%) and disappearance of blood flow delay in the left MCA region. (d) MRA the day after PTA showing increased blood flow signals in the left ICA and left MCA compared to preoperative ones, but the left-right asymmetry in ICA diameters remained. (e) MRA 5 days after PTA showing increased blood flow signals in the left ICA. (f) MRA 11 days after PTA showing maintenance of increased blood flow signals in the left ICA. MRA: Magnetic resonance angiography, ICA: Internal carotid artery, MCA: Middle cerebral artery, PTA: Percutaneous transluminal angioplasty, WASID: Warfarin-aspirin symptomatic intracranial disease.
Initial PTA
An 8-Fr Optimo Epd balloon catheter (Tokai Medical Products, Kasugai, Japan) was guided to the cervical portion of the left ICA. It was deemed difficult to guide a distal access catheter to proximal ICA collapse, so an Excelsior SL-10 microcatheter (Stryker, Kalamazoo, MI, USA) and a Chikai 14 200 cm guidewire (Asahi Intecc, Seto, Japan) were guided from the Optimo Epd. The CHIKAI 14 passed through the stenosis and reached the MCA superior trunk. The Excelsior SL-10 was removed from the extended CHIKAI 14, and an Unryu xp 1.5 mm × 10 mm (Kaneka Medix, Osaka, Japan) was guided along the CHIKAI 14, but collapse and tortuosity of the proximal ICA made it difficult to guide it to the stenosis. Staged dilatation of the C3 portion of the ICA was performed with an Unryu xp balloon 1.5 mm × 10 mm and an Unryu xp balloon 2.0 mm × 10 mm. Angiography confirmed dilatation of the stenosis (WASID 71%) and disappearance of blood flow delay in the left MCA region, and the operation was completed [
The day after PTA, she improved to no neurological deficit, and clopidogrel 75 mg/day was added to the medication; MRI showed no enlargement of the infarcted area, and MRA showed increased blood flow signals in the left ICA and left MCA compared to preoperatively, but the left-right asymmetry in the ICA diameters remained [
Despite management of medical risk factors and administration of one antiplatelet drug, a second cerebral infarction due to stenosis at the C3 portion of the left ICA occurred, for which stenting was indicated. Since MRA and CTA confirmed dilation of proximal ICA collapse, Wingspan stenting was deemed feasible by placing a distal access catheter in the proximal ICA. A second PTA was scheduled 13 days after initial PTA.
Second PTA
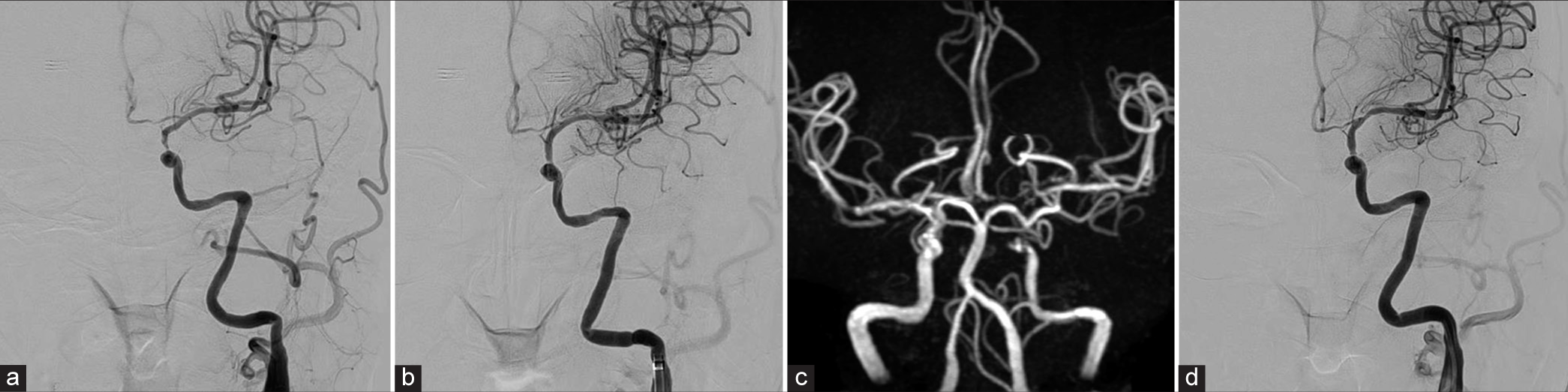
Angiography showed dilation of proximal ICA collapse and improvement of vascular tortuosity [
Figure 3:
Perioperative images of second percutaneous transluminal angioplasty. (a) Preoperative angiography showing dilatation of proximal ICA collapse and improvement of vascular tortuosity. (b) Postoperative angiography showing dilatation of stenosis (WASID 55%). (c) Magnetic resonance angiography the day after stenting showing good blood flow in the left ICA. (d) Angiography 6 months after stenting showing further improvement of proximal ICA collapse. ICA: Internal carotid artery, WASID: Warfarin-aspirin symptomatic intracranial disease.
Postoperative course
Postoperative neurological findings were normal. MRA the day after stenting showed good blood flow in the left ICA [
DISCUSSION
The course of this case suggested that proximal ICA collapse occurs due to distal stenosis, that dilatation of distal stenosis improves proximal ICA collapse, and that this improvement is obtained at an early stage. Detailed reports documenting proximal ICA collapse due to distal stenosis have been scarce, whereas there are many reports on the treatment course of distal ICA collapse due to cervical ICA stenosis. In cases of symptomatic cervical ICA stenosis of 50% or more, the frequency of distal ICA collapse is relatively low, ranging from 5% to 12%.[
Just as distal ICA collapse due to proximal stenosis may dilate after dilatation of proximal stenosis, proximal ICA collapse due to distal stenosis may dilate after dilatation of distal stenosis. Distal ICA collapse due to proximal stenosis occurs when severe proximal stenosis reduces blood flow to the distal ICA.[
Since proximal ICA collapse in this case began to dilate 5 days after PTA, dilation of proximal ICA collapse may be obtained early after dilatation of distal stenosis. Matsuda et al. classified cervical ICA stenosis into a single-channel group and a multiple-channel group and reported that the single-channel group achieved improvement in distal vessel diameter immediately after CAS.[
In this case, the intraoperative findings 1 year before PTA showed no proximal ICA collapse, suggesting that the time course of proximal ICA collapse was not long and did not cause organic changes. In addition, no tandem stenotic lesions were observed. Thus, the increased blood flow due to dilatation of distal stenosis may have begun to improve vessel diameter at an early stage. In PTA for stenosis, device guidance to the stenosis and device maneuverability greatly affects the success or failure of the procedure. It has been reported that patients with distal ICA collapse associated with cervical ICA stenosis have difficulty in shunt insertion during CEA due to the narrow distal ICA.[
CONCLUSION
PTA for distal stenosis with proximal ICA collapse may result in dilation of proximal ICA collapse over time.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cay F, Cil BE, Balci S, Arsava EM, Topçuoğlu MA, Arat A. Relevance of distal arterial collapse in stenting of atherosclerotic near-occlusion of the carotid artery. AJNR Am J Neuroradiol. 2020. 41: 1054-60
2. Chai S, Sheng Z, Xie W, Wang C, Liu S, Tang R. Assessment of apparent internal carotid tandem occlusion on high-resolution vessel wall imaging: Comparison with digital subtraction angiography. AJNR Am J Neuroradiol. 2020. 41: 693-9
3. Clark OH, Moore WS, Hall AD. Radiographically occluded, anatomically patent carotid arteries. Arch Surg. 1971. 102: 604-6
4. Glagov S, Bassiouny HS, Sakaguchi Y, Goudet CA, Vito RP. Mechanical determinants of plaque modeling, remodeling and disruption. Atherosclerosis. 1997. 131: S13-4
5. Greiner C, Wassmann H, Palkovic S, Gauss C. Revascularization procedures in internal carotid artery pseudo-occlusion. Acta Neurochir (Wien). 2004. 146: 237-43
6. Gu T, Aviv RI, Fox AJ, Johansson E. Symptomatic carotid near-occlusion causes a high risk of recurrent ipsilateral ischemic stroke. J Neurol. 2020. 267: 522-30
7. Hirata Y, Sakata N, Tsuchimochi H, Tsugu H, Onishi H, Inoue T. Carotid endarterectomy for pseudo-occlusion of the cervical internal carotid artery. Acta Neurochir Suppl. 2014. 119: 91-6
8. Johansson E, Öhman K, Wester P. Symptomatic carotid near-occlusion with full collapse might cause a very high risk of stroke. J Intern Med. 2015. 277: 615-23
9. Lippman HH, Sundt TM, Holman CB. The poststenotic carotid slim sign: Spurious internal carotid hypoplasia. Mayo Clin Proc. 1970. 45: 762-7
10. Matsuda Y, Terada T, Okada H, Masuo O, Ohshima K, Tsuura M. Angiographic characteristics of pseudo-occlusion of the internal carotid artery before and after stenting. Neurosurgery. 2016. 79: 832-8
11. Morgenstern LB, Fox AJ, Sharpe BL, Eliasziw M, Barnett HJ, Grotta JC. The risks and benefits of carotid endarterectomy in patients with near occlusion of the carotid artery. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Neurology. 1997. 48: 911-5
12. Neves CR, Casella IB, da Silva ES, Puech-Leão P. Medical therapy for asymptomatic patients and stent placement for symptomatic patients presenting with carotid artery near-occlusion with full collapse. J Vasc Interv Radiol. 2018. 29: 998-1005
13. Omoto K, Takayama K, Myouchin K, Wada T, Nakagawa I, Tanaka T. Carotid artery stenting for near occlusion with full collapse. World Neurosurg. 2022. 163: e215-22
14. Zhang J, Chen J, Xu X, Sun M, Chen S, Liu P. Carotid endarterectomy for the treatment of carotid near-occlusion with recurrent symptoms. Front Neurol. 2022. 13: 765-95