- Department of Neurosurgery, Sapienza University, Rome, Italy.
DOI:10.25259/SNI_128_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Valerio di Norcia, Luigi Valentino Berra, Luca D’Angelo, Antonio Santoro. Dorsal epidural “Spindle Cell Lipoma” in a pregnant female. 14-Apr-2021;12:162
How to cite this URL: Valerio di Norcia, Luigi Valentino Berra, Luca D’Angelo, Antonio Santoro. Dorsal epidural “Spindle Cell Lipoma” in a pregnant female. 14-Apr-2021;12:162. Available from: https://surgicalneurologyint.com/surgicalint-articles/10710/
Abstract
Background: Spindle cell lipoma (SCL) constitutes just 1.5% of all lipomatous tumors. They typically occur in the upper back and shoulders. Here, we report a 37-year-old female presenting with a SCL in the dorsal epidural thoracic spine, during her 9th month of pregnancy.
Case Description: A 37-year-old female presented with a subacute (2 months) progressive paraparesis during her 9th month of pregnancy. The MR showed a dorsal epidural mass at the D8 level. Following a cesarean section, the patient underwent a laminectomy for tumor excision. Microscopically, the lesion proved to be a SCL. At 5-year follow-up, there was no tumor recurrence.
Conclusion: SCL represents a variant of benign lipomas that may occur in the dorsal thoracic spine. Gross total excision may be followed by a benign clinical course without recurrence or malignant degeneration. Very atypical SCLs need closer follow-up to avoid the misdiagnosis of liposarcoma.
Keywords: Epidural space, Liposarcoma, Neurosurgery, Spindle cell lipoma, Spine
INTRODUCTION
Lipomas are benign tumors arising from mature adipocytes. The variant called spindle cell lipoma (SCL), accounting for only 1.5% of all lipomatous tumors, is about 60 times less common than benign lipomas.[
MATERIALS AND METHODS
A 37-year-old female presented with paresthesias/hypoesthesias and mild bilateral lower extremity paraparesis (3–4/5 proximally/distally) over the past 2 months of her pregnancy.
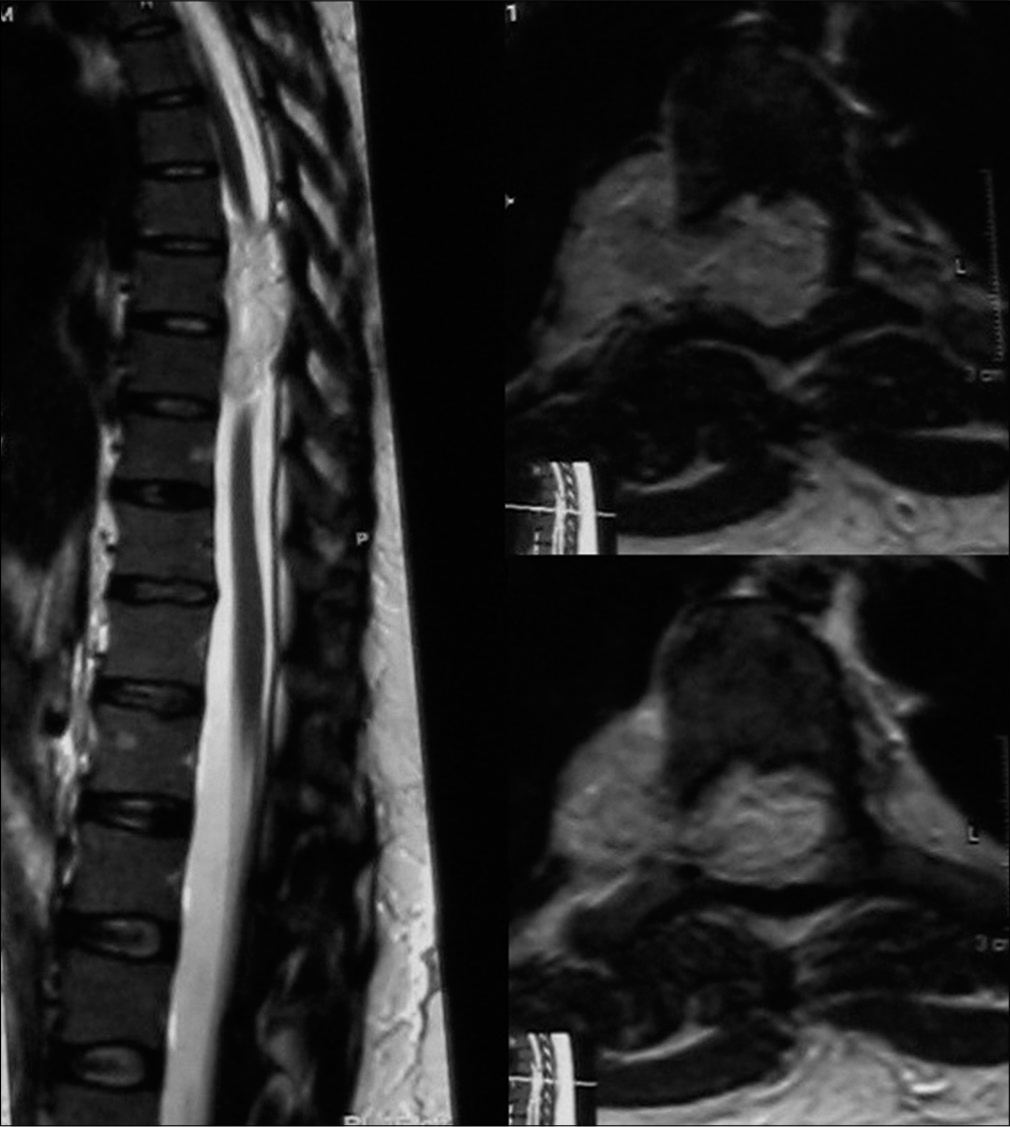
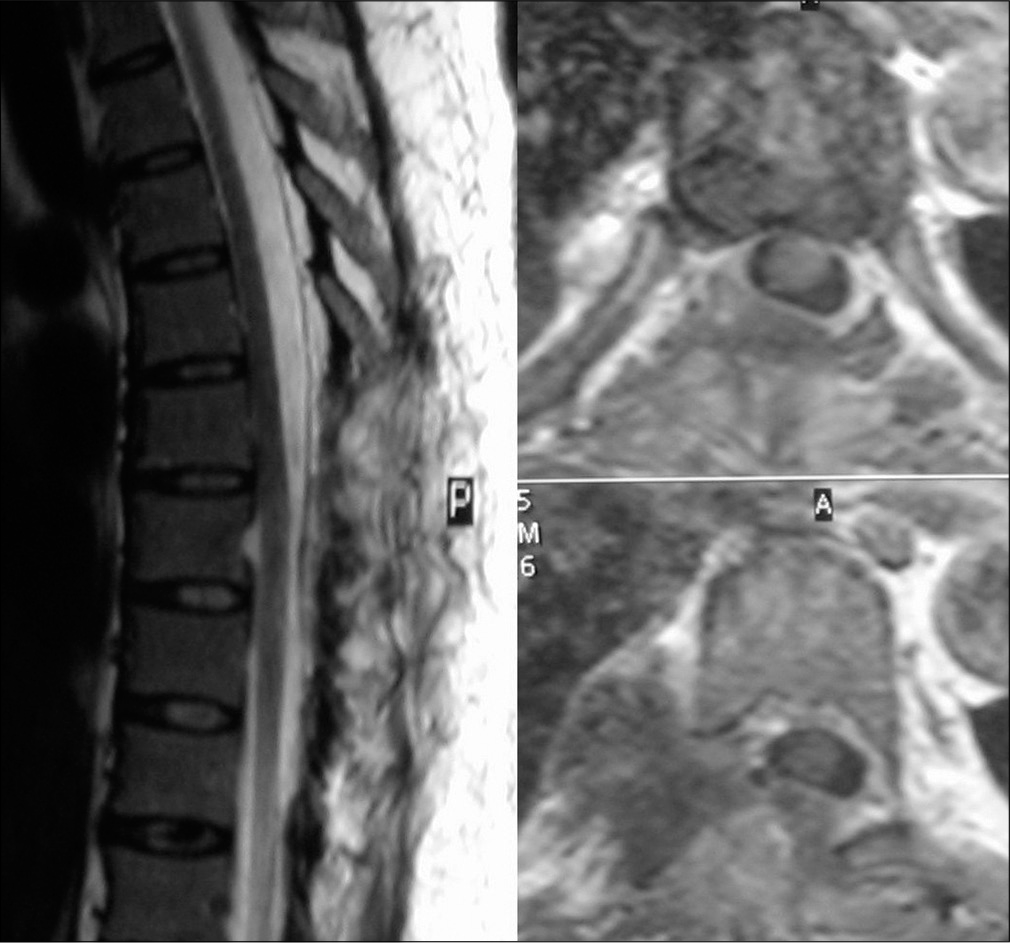
The MR revealed an epidural, slightly irregular, mass (5 × 3 cm) extending from D7 to D9 that compressed the dural sac, and extruded through the right D8–D9 neural foramen [
Surgery
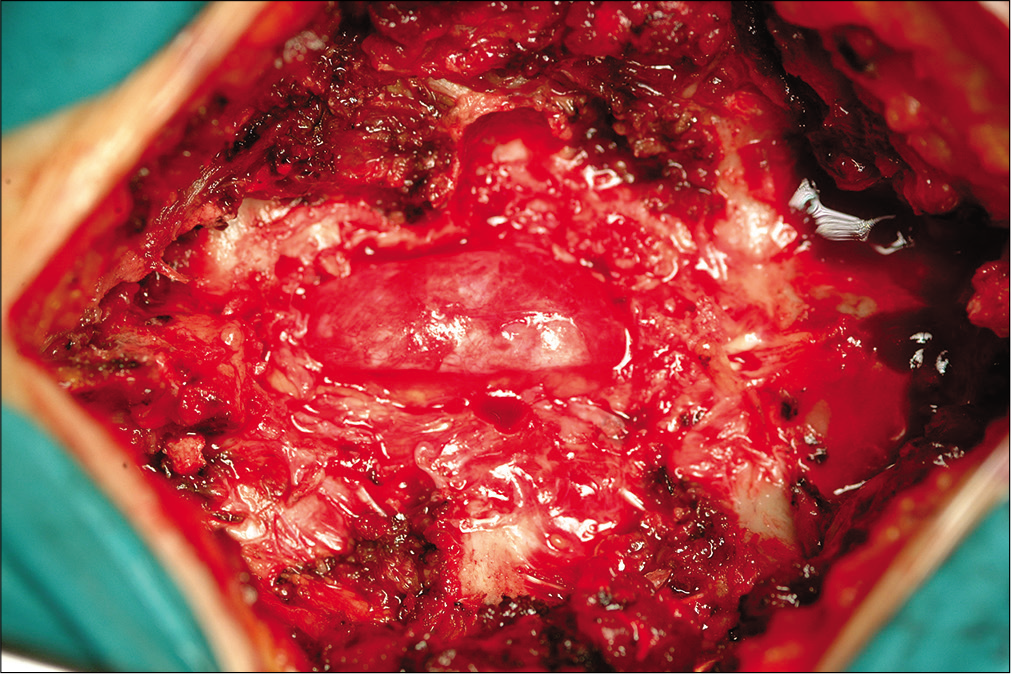
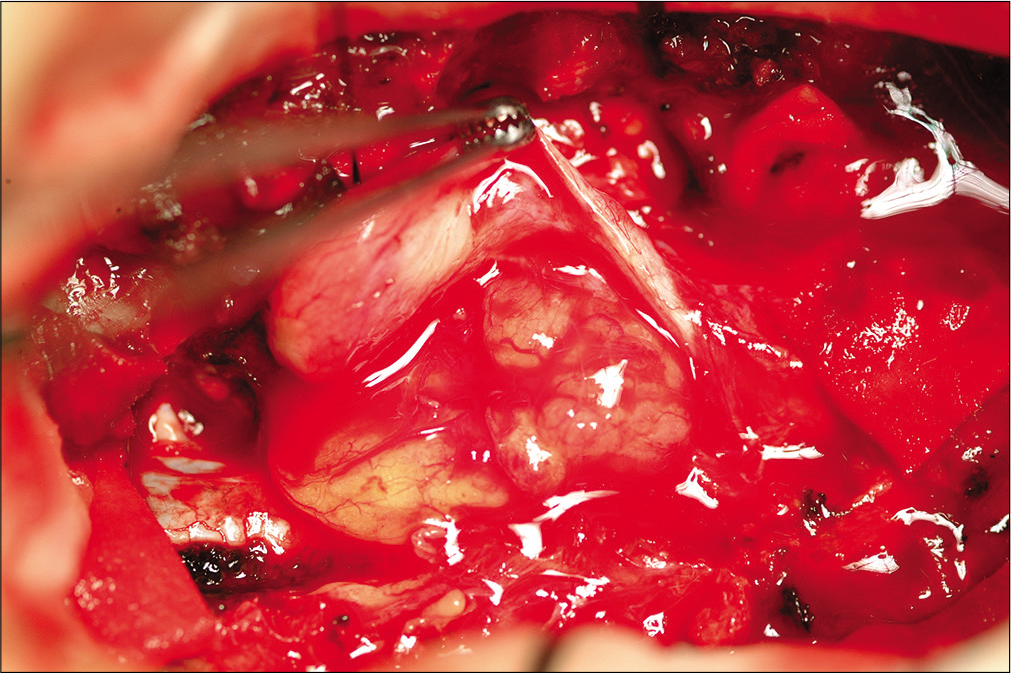
Following a cesarean section, the patient underwent D7– D9 laminectomy and right partial D8 costotrasversectomy [
Histology
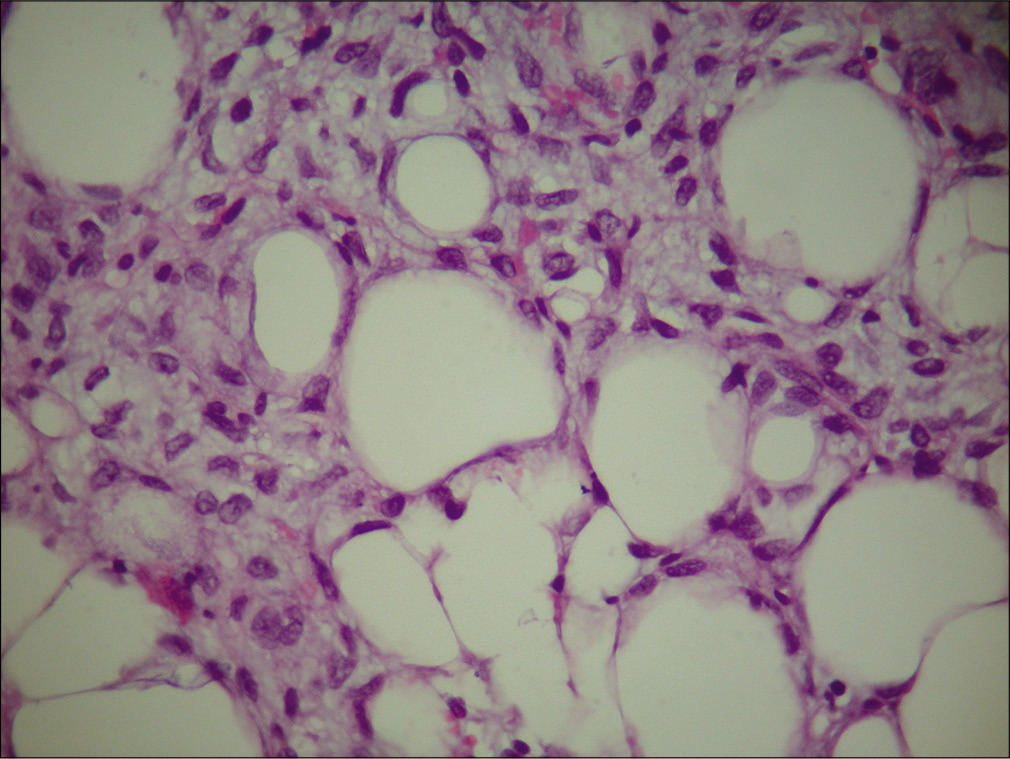
The tumor consisted of adipose tissue with features of a typical SCL: Spindle cells in a myxoid stroma within lobules of mature adipose tissue [
Postoperative course
At 24 h after surgery, a postoperative MR confirmed the complete removal of the lesion [
DISCUSSION
Here, we presented a 37-year-old pregnant female, with a 2-month history of a progressive paraparesis attributed to a SCL and hormonal changes.[
The MR documented a hyperintense lesion on T1-weighted images, a hypointense lesion on T2-weighted studies, and inhomogeneous intralesional enhancement. Surgical intervention is typically effective in eradicating these tumors, which do not warrant further adjunctive treatment (e.g., radiation or chemotherapy).
Histology/pathology
Histologically and macroscopically these lesions are well-encapsulated lobulated masses, similar to the classical lipomas, with some gray-whitish areas, high cellularity zones, without calcifications, necrosis, or hemorrhages. Typically, mature adipocytes are replaced by small spindle cells looking like fibroblasts, within a matrix of collagen fibril and mucin.[
In our case, an equal distribution of not-adipose and adipose cells population was evident, surrounded by a stroma rich in mucin and without fibrous filaments. Vascularization was well represented, but without the plexiform aspect: This characteristic, with the absence of lipoblasts, allowed a quick distinction from the myxoid liposarcoma.
Immunohistochemistry
SCLs are considered positive to CD34 and usually negative to desmin reactions.[
Postoperative MR studies
The first MR at 24 h after surgery showed, in this case, complete removal of the mass. Five days after surgery, the patient was discharged neurologically intact. During the 5-year follow-up period, there were no signs of tumor recurrence on follow-up MR studies. As these lesions are benign, this absence of recurrence was anticipated.
CONCLUSION
A 37-year-old female presented with 2 months of a progressive paraparesis attributed to a dorsal D7–D9 benign epidural SCL. Five years following gross total tumor excision, the patient’s symptoms resolved and the tumor never recurred.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Badeau M, Vihma V, Mikkola TS, Tiitinen A, Tikkanen MJ. Estradiol fatty acid esters in adipose tissue and serum of pregnant and pre-and postmenopausal women. J Clin Endocrinol Metab. 2007. 92: 4327-31
2. Bancroft LW, Kransdorf MJ, Peterson JJ, Sundaram M, Murphey MD, O’Connor MI. Imaging characteristics of spindle cell lipoma. AJR Am J Roentgenol. 2003. 181: 1251-4
3. Fletcher CD, Martin-Bates E. Spindle cell lipoma: A clinicopathological study with some original observations. Histopathology. 1987. 11: 803-17
4. Kransdorf MJ, Murphey MD, McAllister L, Barrett K.editors. Soft tissue tumors in a large referral population: Prevalence and distribution of diagnoses by age, sex and location. Imaging of Soft Tissue Tumors. Philadelphia, PA: Saunders; 2006. p. 6-38
5. Oaks J, Margolis DJ. Spindle cell lipoma of the mediastinum: A differential consideration for liposarcoma. J Thorac Imaging. 2007. 22: 355-7
6. Tardio JC, Aramburu JA, Santonja C. Desmin expression in spindle cell lipomas: A potential diagnostic pitfall. Virchows Arch. 2004. 445: 354-8
7. Turhan-Haktanir N, Demir Y, Ayçiçek A, Aktepe F, Calişkan G. Concurrent large spindle cell and ordinary lipomas. J Craniofac Surg. 2007. 18: 1193-5
8. Weiss SW, Weiss SW, Goldblum JR.editors. Benign lipomatous tumors. Enzinger and Weiss’s Soft Tissue Tumors. Philadelphia, PA: Mosby; 2008. p. 429-76