- Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, USA
- Department of Orthopaedics, Cedars-Sinai Medical Center, Los Angeles, USA
- Department of Neurosurgery, University of California Davis Medical Center, Sacramento, California, USA
Correspondence Address:
Doniel Drazin
Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, USA
DOI:10.4103/2152-7806.159381
Copyright: © 2015 Al-Khouja L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Al-Khouja L, Shweikeh F, Pashman R, Johnson JP, Kim TT, Drazin D. Economics of image guidance and navigation in spine surgery. Surg Neurol Int 25-Jun-2015;6:
How to cite this URL: Al-Khouja L, Shweikeh F, Pashman R, Johnson JP, Kim TT, Drazin D. Economics of image guidance and navigation in spine surgery. Surg Neurol Int 25-Jun-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/economics-of-image-guidance-and-navigation-in-spine-surgery/
Abstract
Background:Image-guidance and navigation in spinal surgery is becoming more widely utilized. Several studies have shown the use of this technology to increase accuracy of pedicle screw placement, decrease the rates of revision surgery, and minimize radiation exposure. In this paper, the authors analyze the economics of image-guided surgery (IGS) and navigation in spine surgery.
Methods:A literature review was performed using PubMed, the CEA Registry, and the National Health Service Economic Evaluation Database. Each article was screened for inclusion and exclusion criteria, including costs, reoperation, readmission rates, operating room time, and length of stay.
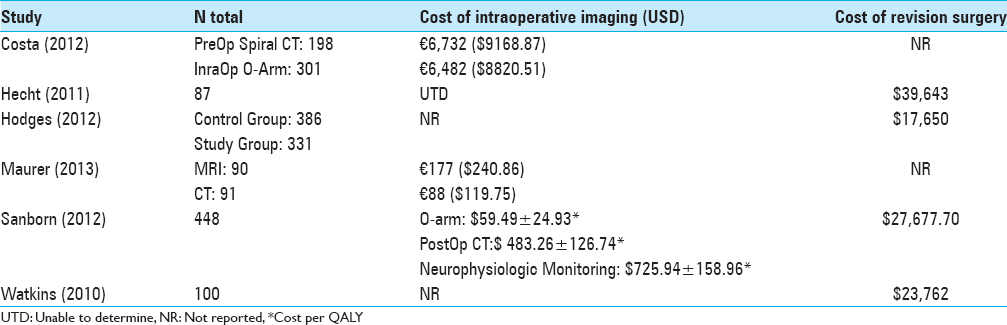
Results:Thirteen studies were included in the analysis. Six studies were identified to meet the inclusion criteria for reporting costs and seven met the criteria for analysis of efficacy. Average costs ranged from $17,650 to $39,643. Pedicle screw misplacement rates using IGS ranged from 1.20% to 15.07% while reoperation rates ranged from 0% to 7.42%.
Conclusion:There is currently an insufficient amount of studies reporting on the economics of spinal navigation to accurately conclude on its cost-effectiveness in clinical practice. Although a few of these studies showed less costs associated with intraoperative imaging, none were able to establish a statistically significant difference. Preliminary findings drawn from this study indicate a possible cost-effectiveness advantage with IGS, but more comprehensive data on costs need to be reported in order to validate its utilization.
Keywords: Costs, fluoroscopy, image-guidance, navigation, reoperation
INTRODUCTION
Currently, there are several types of spinal navigation systems that utilize X-ray, computed tomography (CT), magnetic resonance imaging (MRI), and 3D fluoroscopy to avoid misplacement of screws/instrumentation. Accurate placement of instrumentation is critical to avoid iatrogenic morbidity.[
MATERIALS AND METHODS
The search engines PubMed, CEA Registry, and National Health Service Economic Evaluation Databases (NHS EED) were utilized. The following were the key words used in the search: Spine, costs, navigation, O-arm, C-arm, image guidance, readmission, reoperation, fluoroscopy, CT, spine, and revision. The following costs were evaluated: Intraoperative imaging, revision/reoperation, number of screws used/misplaced, operating room (OR) time, length of stay, imaging method, and number requiring post-operative CT scans.
RESULTS
Six studies were identified to meet the inclusion criteria for reporting costs through PubMed, CEA Registry, and NHS EED. Four of the six studies (66.67%) reported costs of intraoperative imaging [
All seven studies reported rates of reoperation and six of the seven studies reported on rates of screw misplacement (85.71%). Pedicle screw misplacement rates ranged from 1.20% to 15.07% while reoperation rates ranged from 0% to 7.42%. These numbers are slightly higher compared to previous studies showing that IGS decreased overall pedicle screw misplacement rates to 0–9%.[
DISCUSSION
Although many authors have shown support for the use of IGS, there is a scarcity of literature reporting the costs associated with spinal navigation or comparative studies showing cost differences between various interventions.[
A few studies have already reported that IGS decreases procedure time compared with conventional methods.[
Koktekir et al. found that intraoperative fluoroscopy significantly decreased risk of misplacement at rates comparable to other imaging methods (i.e. CT).[
Occupational exposure to radiation when utilizing intraoperative imaging has also been a topic not thoroughly investigated. Watkins et al. measured the amount of exposure 0.18 mrem/case for a total of 18 mrem/100 cases, consistent with other studies discussing radiation exposure with spinal intraoperative imaging, [
Lu and colleagues noted that most spinal surgical interventions become reasonably cost effective after 2 years and increase in cost-effectiveness over time.[
Of further note, each of these six studies considered various modalities used in image-guided spine surgery, which makes it more difficult to ascertain which of them ranks superiorly to the others. Ideally, we would need studies that look at each of these IGS technologies and perform a CEA in a standardized fashion with the appropriate statistical analyses as stated above in order to perform an accurate meta-analysis. This will provide more reliable data to help establish an accurate conclusion. This systematic review further shows that we currently do not have the data or evidence to show if one IGS procedure is more cost effective than the other in a reliable and reproducible study.
Study limitations
There was no standardized methodology utilized among the studies to make reasonable conclusions regarding their findings. Each study's approach to data collection and statistical analysis was also different, making it difficult to make conclusions regarding any of these IGS techniques. However, the sampling of articles used is believed to be representative of currently published data on the effectiveness of screw placement using intraoperative imaging techniques. Additionally, no formal statistical analysis could be performed on the data collected, as expected, making it difficult to achieve any conclusion on the cost-effectiveness of IGS for spine surgeries.
Future outlook
In addressing the economics of spinal navigation in the future, investigating costs should incorporate direct, indirect, and total costs over a minimum of 2 years to establish proper conclusions. Monetary values of interest include cost of initial surgery with or without spinal navigation, cost of supplies/personnel required for the use of the IGS, and cost of reoperation. Nonmonetary variables of interest include rates of pedicle screw misplacement, rates of reoperation, levels of radiation exposure per case, and OR time. Determining these variables will allow for more accurate conclusions to be made regarding the cost-effectiveness of spinal navigation in hope of making appropriate economic changes within our healthcare system.
CONCLUSION
There is currently an insufficient amount of studies reporting on the costs of spinal navigation to accurately conclude on its cost-effectiveness in clinical practice. Although a few of these studies showed less costs associated with intraoperative imaging, none were able to establish a statistically significant difference. Preliminary findings from this study indicate a possible cost-effectiveness with the utilization of spinal navigation, but more definitive and detailed data on costs need to be reported in order to perform a more accurate cost analysis.
References
1. Abe Y, Ito M, Abumi K, Kotani Y, Sudo H, Minami A. A novel cost-effective computer-assisted imaging technology for accurate placement of thoracic pedicle screws. J Neurosurg Spine. 2011. 15: 479-85
2. Baaj AA, Beckman J, Smith DA. O-Arm-based image guidance in minimally invasive spine surgery: Technical note. Clin Neurol Neurosurg. 2013. 115: 342-5
3. Braak SJ, Zuurmond K, Aerts HC, van Leersum M, Overtoom TT, van Heesewijk JP. Feasibility study of needle placement in percutaneous vertebroplasty: Cone-beam computed tomography guidance versus conventional fluoroscopy. Cardiovasc Intervent Radiol. 2013. 36: 1120-6
4. Boos N. The impact of economic evaluation on quality management in spine surgery. Eur Spine J. 2009. 18: S338-47
5. Bydon M, Xu R, Amin AG, Macki M, Kaloostian P, Sciubba DM. Safety and efficacy of pedicle screw placement using intraoperative computed tomography: Consecutive series of 1148 pedicle screws. J Neurosurg Spine. 2014. 21: 320-8
6. Costa F, Porazzi E, Restelli U, Foglia EC, Cardia A, Ortolina A. Economic study: A cost-effectiveness analysis of an intraoperative compared with a preoperative image-guided system in lumbar pedicle screw fixation in patients with degenerative spondylolisthesis. Spine J. 2014. 14: 1790-6
7. Garber ST, Bisson EF, Schmidt MH. Comparison of three-dimensional fluoroscopy versus postoperative computed tomography for the assessment of accurate screw placement after instrumented spine surgery. Global Spine J. 2012. 2: 95-8
8. Hecht AC, Koehler SM, Laudone JC, Jenkins A, Qureshi S. Is intraoperative CT of posterior cervical spine instrumentation cost-effective and does it reduce complications?. Clin Orthop Relat Res. 2011. 469: 1035-41
9. Hodges SD, Eck JC, Newton D. Analysis of CT-based navigation system for pedicle screw placement. Orthopedics. 2012. 35: e1221-4
10. Houten JK, Nasser R, Baxi N. Clinical assessment of percutaneous lumbar pedicle screw placement using the O-arm multidimensional surgical imaging system. Neurosurgery. 2012. 70: 990-5
11. Kim TT, Drazin D, Shweikeh F, Pashman R, Johnson JP. Clinical and radiographic outcomes of minimally invasive percutaneous pedicle screw placement with intraoperative CT (O-arm) image guidance navigation. Neurosurg Focus. 2014. 36: E1-
12. Koktekir E, Ceylan D, Tatarli N, Karabagli H, Recber F, Akdemir G. Accuracy of fluoroscopically-assisted pedicle screw placement: Analysis of 1,218 screws in 198 patients. Spine J. 2014. 14: 1702-8
13. Larson AN, Polly DW, Guidera KJ, Mielke CH, Santos ER, Ledonio CG. The accuracy of navigation and 3D image-guided placement for the placement of pedicle screws in congenital spine deformity. J Pediatr Orthop. 2012. 32: e23-9
14. Lu Y, Qureshi SA. Cost Effectiveness Studies in Spine Surgeries: A Narrative Review. Spine J. 2014. 14: 2748-62
15. Maurer MH, Schreiter N, De bucourt M, Grieser C, Renz DM, Hartwig T. Cost comparison of nerve root infiltration of the lumbar spine under MRI and CT guidance. Eur Radiol. 2013. 23: 1487-94
16. Nottmeier EW, Seemer W, Young PM. Placement of thoracolumbar pedicle screws using three-dimensional image guidance: Experience in a large patient cohort. J Neurosurg Spine. 2009. 10: 33-9
17. Oertel MF, Hobart J, Stein M, Schreiber V, Scharbrodt W. Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. J Neurosurg Spine. 2011. 14: 532-6
18. Parker SL, Shau DN, Mendenhall SK, McGirt MJ. Factors influencing 2-year health care costs in patients undergoing revision lumbar fusion procedures. J Neurosurg Spine. 2012. 16: 323-8
19. Resnick DK. Digital versus plain film imaging in the operating room: Cost and safety considerations. Spine J. 2009. 9: 1035-6
20. Rivkin MA, Yocom SS. Thoracolumbar instrumentation with CT-guided navigation (O-arm) in 270 consecutive patients: Accuracy rates and lessons learned. Neurosurg Focus. 2014. 36: E7-
21. Sanborn MR, Thawani JP, Whitmore RG, Schmulevich M, Hardy B, Benedetto C. Cost-effectiveness of confirmatory techniques for the placement of lumbar pedicle screws. Neurosurg Focus. 2012. 33: E12-
22. Steinmetz MP, Mroz TE, Krishnaney A, Modic M. Conventional versus digital radiographs for intraoperative cervical spine-level localization: A prospective time and cost analysis. Spine J. 2009. 9: 967-71
23. Tjardes T, Shafizadeh S, Rixen D, Paffrath T, Bouillon B, Steinhausen ES. Image-guided spine surgery: State of the art and future directions. Eur Spine J. 2010. 19: 25-45
24. Tormenti MJ, Kostov DB, Gardner PA, Kanter AS, Spiro RM, Okonkwo DO. Intraoperative computed tomography image-guided navigation for posterior thoracolumbar spinal instrumentation in spinal deformity surgery. Neurosurg Focus. 2010. 28: E11-
25. Torres J, James AR, Alimi M, Tsiouris AJ, Geannette C, Härtl R. Screw placement accuracy for minimally invasive transforaminal lumbar interbody fusion surgery: A study on 3-d neuronavigation-guided surgery. Global Spine J. 2012. 2: 143-52
26. Tow BP, Yue WM, Srivastava A, Lai JM, Guo CM, Peng BC. Does Navigation Improve Accuracy of Placement of Pedicle Screws in Single Level Lumbar Degenerative Spondylolisthesis?-A Comparison Between Free-hand and 3D O-Arm Navigation Techniques. J Spinal Disord Tech. 2013. p.
27. van de kelft E, Costa F, Van der planken D, Schils F. A prospective multicenter registry on the accuracy of pedicle screw placement in the thoracic, lumbar, and sacral levels with the use of the O-arm imaging system and StealthStation Navigation. Spine. 2012. 37: E1580-7
28. van der Roer N, Boos N, van Tulder MW. Economic evaluations: A new avenue of outcome assessment in spinal disorders. Eur Spine J. 2006. 15: S109-1
29. Watkins RG, Gupta A, Watkins RG. Cost-effectiveness of image-guided spine surgery. Open Orthop J. 2010. 4: 228-33
30. Whitmore RG, Stephen J, Stein SC, Campbell PG, Yadla S, Harrop JS. Patient comorbidities and complications after spinal surgery: A societal-based cost analysis. Spine (Phila Pa 1976). 2012. 37: 1065-71
31. Yang BP, Wahl MM, Idler CS. Percutaneous lumbar pedicle screw placement aided by computer-assisted fluoroscopy-based navigation: Perioperative results of a prospective, comparative, multicenter study. Spine. 2012. 37: 2055-60
32. Zausinger S, Scheder B, Uhl E, Heigl T, Morhard D, Tonn JC. Intraoperative computed tomography with integrated navigation system in spinal stabilizations. Spine. 2009. 34: 2919-26