- College of Osteopathic Medicine, Kansas City University, Kansas City, Missouri, United States,
- School of Medicine, Universidad Anáhauc Querétaro, Santiago de Querétaro, Mexico,
- Department of Neurosurgery, Desert Regional Medical Center, Palm Springs, California, United States,
- College of Osteopathic Medicine, William Carey University, Hattiesburg, Mississippi, United States.
DOI:10.25259/SNI_415_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Frank De Stefano1, Timothy Mayo1, Claudia Covarrubias2, Brian Fiani3, Brian Musch4. Effect of comorbidities on ischemic stroke mortality: An analysis of the National Inpatient Sample (NIS) Database. 07-Jun-2021;12:268
How to cite this URL: Frank De Stefano1, Timothy Mayo1, Claudia Covarrubias2, Brian Fiani3, Brian Musch4. Effect of comorbidities on ischemic stroke mortality: An analysis of the National Inpatient Sample (NIS) Database. 07-Jun-2021;12:268. Available from: https://surgicalneurologyint.com/surgicalint-articles/10858/
Abstract
Background: Stroke risk has been attributed to many pathological and behavioral conditions. Various modifiable and non-modifiable risk factors have been recognized and found consistent throughout epidemiological studies. Herein, we investigate the effect of comorbidities seen with patient’s suffering from ischemic stroke and its effect on in-hospital mortality.
Methods: We identified patients >18 year old in the National Inpatient Sample database with diseases of interest utilizing the tenth International Classification of Disease 10 diagnostic codes from the years 2016 to 2018. Interval data were analyzed using one-way ANOVA. Post hoc analysis was performed using Bonferroni correction methods. To determine independent predictors of in-hospital mortality, odds ratios were calculated using binary logistic regression for each comorbidity. Descriptive and numerical statistics, imputation, and logistic regression were calculated using SPSS software version 25.
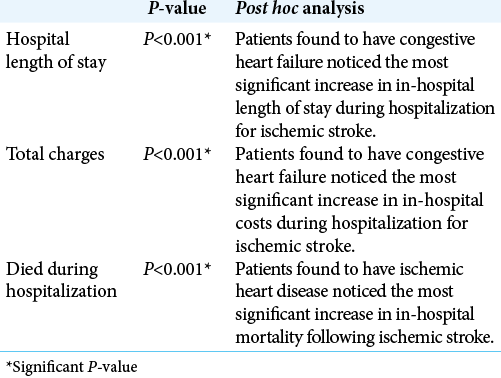
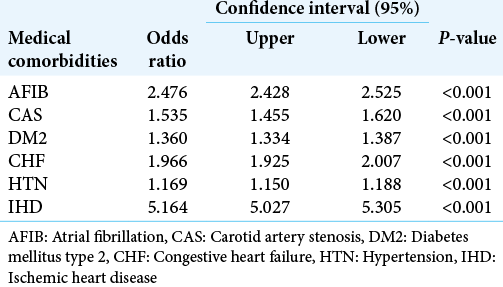
Results: Patients hospitalized with ischemic stroke were found to have the following comorbidities: atrial fibrillation (7.5%), carotid artery stenosis (1.1%), diabetes mellitus type 2 (11.4%), congestive heart failure (CHF) (7.5%), essential hypertension (21.2%), and ischemic heart disease (IHD) (2.3%). In-hospital mortality rates were higher in patients hospitalized with ischemic stroke and concomitant IHD (28.2%, P P P
Conclusion: Patients hospitalized from ischemic stroke suffered from the coexistence of other comorbidities. Of the comorbidities studied, IHD was identified as having the most significant impact on in-hospital mortality.
Keywords: Atrial fibrillation, Carotid artery stenosis, Congestive heart failure, Diabetes mellitus, Ischemic heart disease
INTRODUCTION
Stroke is a major cause of death and disability with serious economic and social consequences. Every year more than 795,000 people have a stroke in the United States (US) alone, with 87% of cases attributed to ischemic stroke.[
Although stroke mortality has been declining over the past few decades due to the introduction of modern treatments, it still remains the fifth leading cause of death in the US, accounting for an estimated 150,000 deaths/year.[
Stroke risk has been attributed to many pathological and behavioral conditions. Although direct causality is difficult to assign given that most patients suffer from multiple comorbidities at once, various modifiable and non-modifiable risk factors have been recognized and found consistent throughout epidemiological studies.[
It is estimated that up to 90% of all strokes are caused by behavioral risk factors, making stroke highly preventable.[
The National Inpatient Sample (NIS) is a large database that is maintained under the Healthcare Cost and Utilization Project (HCUP), which is both considered the largest collection of longitudinal hospital care data in the US and sponsored by the Agency for Healthcare Research and Quality (AHRQ).[
MATERIALS AND METHODS
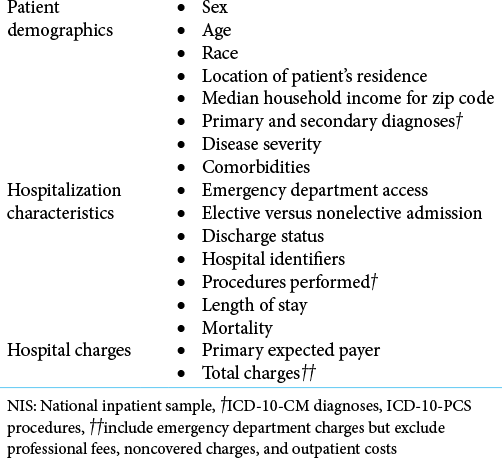
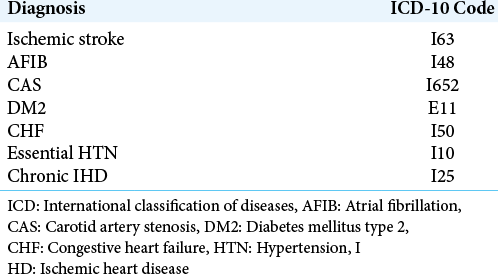
Using the NIS database, we identified patients >18 years old with diseases of interest utilizing the tenth ICD-10 diagnostic codes from the years 2016 to 2018. To better account for national estimates, our sample data were weighted using the provided discharge weights from the NIS database. This weighting scale provides a sample of discharges from all hospitals nationally within the HCUP. Patients diagnosed with ischemic stroke were identified using the ICD-10 code of interest listed as the first primary diagnosis, indicating a primary diagnosis at hospital discharge. Comorbidities of interest were identified using the subsequent three diagnosis codes following the primary diagnosis code. [
Demographic data in the form of gender, age, and race were collected for analysis from the NIS database. Patient outcomes were evaluated using data from the NIS database including length of stay, total health-care costs billed during hospitalization, and in-hospital mortality. In-hospital mortality is defined as patients dying during hospitalization. Charges accrued during hospital stay did not include professional fees and noncovered charges. If the total charges provided included professional fees, then professional fees were subtracted from the total charge during HCUP processing.
[
RESULTS
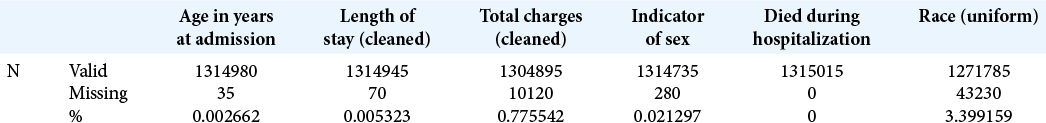
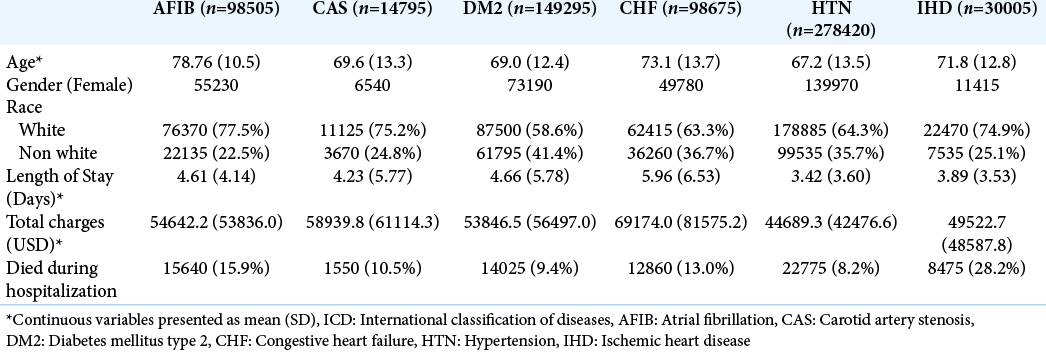
A total of 1,441,230 hospitalizations were identified with ischemic stroke between 2016 and 2018. 126,215 cases were excluded from this study due to multiple comorbidities reported. 1,315,015 cases were included in this study: about 50.8% female and 49.2% male with a mean age of 69.9 ± 14.4 years. Patients hospitalized with ischemic stroke were found to have the following comorbidities: AFIB (7.5%), carotid artery stenosis (CAS) (1.1%), DM type 2 (DM2) (11.4%), congestive heart failure (CHF) (7.5%), essential HTN (21.2%), and ischemic heart disease (IHD) (2.3%). [
[
[
DISCUSSION
Patients suffering from ischemic have variable mortality rates depending on modifiable and non-modifiable risk factors. These risk factors increase susceptibility to ischemic as well as a variety of pathologic comorbidities that may put patients at increased risk for stroke mortality. Our results indicated that in individuals with ischemic stroke, mortality is over 5 times higher when concomitant IHD is present, significantly higher than the other comorbidities studied. In addition, we found that in individuals suffering from ischemic stroke, mortality is roughly 1.2 times higher when individuals have pre-existing HTN, the lowest increase in mortality of the comorbidities studied. Despite these findings, however, we found that both the length of stay and total in hospital charges were lowest and second lowest in HTN and IHD, respectively.
The relationship between relatively short length of stay and increased odds of mortality as seen in patients with ischemic stroke suffering from concomitant IHD supports previous research.[
This study is limited by the inherent nature of retrospective study design and database review. The large sample size of the data collected, however, decreases likelihood of results being produced by confounding variables or chance. The NIS database consists of patient data strictly from US hospitals. Although the sample size is sufficient for interpretation, the outcomes and relationships displayed in our findings may not necessarily apply to other populations. In addition, the database accuracy is relied on heavily when patients are admitted for hospitalization. As such, it is possible that reporting error and misclassification biases existed within databases relying on patient sourcing.
With these factors in mind, it is important to notice that conditions such as AFIB, CAS, DM2, and CHF present in patients experiencing stroke all yielded somewhat similar increase in odds of in-hospital mortality. Further research is needed to evaluate the risk factors shared between these individual conditions and risk factors for ischemic stroke. In addition, the relationships between these risk factors may be further classified (e.g. causal, overlapping, and synergistic).
CONCLUSION
In patients hospitalized from ischemic stroke, the coexistence of other comorbidities – AFIB, CAS, DM2, CHF, HTN, and IHD notably increases the odds of in-hospital mortality. Of the comorbidities studied, IHD made the most significant impact on mortality. Less impactful was AFIB, CHF, CAS, and DM2; the least impactful was HTN. It is possible that the degree of overlap between risk factors of ischemic stroke also plays a large role in the morbidity and mortality. Increased risk factors for ischemia, whether in the context of ischemic stroke or another disease, should be taken into consideration when monitoring and treating patients in the outpatient setting. Further studies evaluating and classifying the relationships between risk factors of various cardiovascular diseases are needed.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barthels D, Das H. Current advances in ischemic stroke research and therapies. Biochim Biophys Acta Mol Basis Dis. 2020. 1866: 165260
2. Donkor ES. Stroke in the 21st century: A snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018. 2018: 3238165
3. NIS Hospital Ownership Files. Available from: https://www.hcupus.ahrq.gov/db/nation/nis/nisownership.jsp [Last accessed on 2021 Apr 25].
4. Herpich F, Rincon F. Management of acute ischemic stroke. Crit Care Med. 2020. 48: 1654-63
5. Jiang X, Morgenstern LB, Cigolle CT, Claflin ES, Lisabeth LD. Multiple chronic conditions and functional outcome after ischemic stroke: A systematic review and meta-analysis. Neuroepidemiology. 2020. 54: 205-13
6. Kelley KA, Tsikitis VL. Clinical research using the national inpatient sample: A brief review of colorectal studies utilizing the NIS database. Clin Colon Rectal Surg. 2019. 32: 33-40
7. Lingsma HF, Bottle A, Middleton S, Kievit J, Steyerberg EW, Marang-van de Mheen PJ. Evaluation of hospital outcomes: The relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res. 2018. 18: 116
8. Murphy SL, Xu J, Kochanek KD, Arias E, Tejada-Vera B. Deaths: Final data for 2018. Natl Vital Stat Rep. 2021. 69: 1-83
9. Soler EP, Ruiz VC. Epidemiology and risk factors of cerebral ischemia and ischemic heart diseases: Similarities and differences. Curr Cardiol Rev. 2010. 6: 138-49
10. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP. Heart disease and stroke statistics-2020 update: A report from the American heart association. Circulation. 2020. 141: e139-596
11. Zafar A, Al-Khamis FA, Al-Bakr AI, Alsulaiman AA, Msmar AH. Risk factors and subtypes of acute ischemic stroke. A study at King Fahd Hospital of the University. Neurosciences (Riyadh). 2016. 21: 246-51