- Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
DOI:10.25259/SNI_701_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anil Kumar Sharma, Charandeep Singh Gandhoke, Nitish Nayak. Effect of coronavirus disease 2019 pandemic on case volume, spectrum, and perioperative coronavirus disease 2019 incidence in neurosurgical patients: An experience at a tertiary care center in India. 13-Nov-2020;11:390
How to cite this URL: Anil Kumar Sharma, Charandeep Singh Gandhoke, Nitish Nayak. Effect of coronavirus disease 2019 pandemic on case volume, spectrum, and perioperative coronavirus disease 2019 incidence in neurosurgical patients: An experience at a tertiary care center in India. 13-Nov-2020;11:390. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10383
Abstract
Background: The volume and spectrum of neurosurgical procedures being performed during the coronavirus disease 2019 (COVID-19) pandemic have significantly changed as compared to the pre-COVID-19 period. The objective of this study is to examine this change and draw useful conclusions.
Methods: We collected data retrospectively of all patients who attended outpatient clinics and who were operated at our institute under the department of neurosurgery from October 23, 2019, to August 23, 2020. These data were then divided into two groups (pre-COVID period and during the COVID pandemic) and compared.
Results: Out of the 388 surgeries performed, 284 surgeries were performed during the pre-COVID period, and 104 surgeries were performed during the COVID pandemic. During this ongoing COVID pandemic, the total number of surgeries performed by the department of neurosurgery decreased significantly by 63.38%, the proportion of routine surgeries performed decreased from 50.35% to 19.23% and the proportion of minor cases increased from 19.72% to 30.77%. The Outpatient Clinic Workflow decreased by 72.3% as compared to the pre-COVID period, and the perioperative COVID-19 reverse transcription-polymerase chain reaction positive incidence in our neurosurgical patients was 11.71%.
Conclusion: This paper highlights the drastic reduction in the operative workflow and the outpatient clinic workflow during the ongoing corona pandemic which will have significant collateral damages in the long run. We will have to strike the right balance between providing our patients with the best medical treatment while limiting the spread of the COVID-19 infection.
Keywords: Case volume, COVID-19, Pandemic, Perioperative COVID-19 incidence, Spectrum
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a worrisome pandemic and remains a challenge for health-care systems worldwide. Since January 30, 2020, when the first case of coronavirus infection was reported from Thrissur, Kerala; India has rapidly become home to a mammoth COVID-19 outbreak.[
We are facing a global pandemic, and it is very important to be clear that there is no correct roadmap to navigate this difficult situation. Neurosurgeons are facing a unique set of challenges, including working beyond their area of practice, prioritization of neurosurgical cases with limited resources, confronting novel ethical dilemmas, exposing themselves to medicolegal threats, and, in some cases, to financial insecurities. Neurosurgeons, in particular, are unfamiliar and uncomfortable with the idea of suspending or postponing surgeries as they are trained for decades to “run toward the fire” rather than away from it.
In the present study, the authors have evaluated the volume and spectrum of neurosurgical patients who have undergone surgery at their institution during the COVID-19 pandemic. These data were compared with the volume and spectrum of neurosurgical patients operated for the same duration in the pre-COVID period. We also present perioperative COVID-19 incidence in our neurosurgical patients and their management during this ongoing pandemic.
MATERIALS AND METHODS
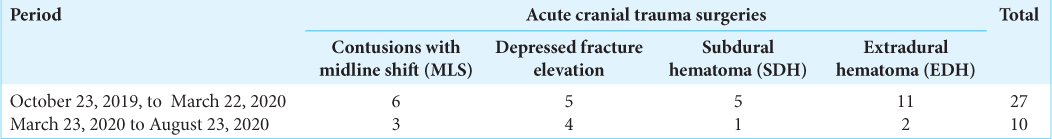
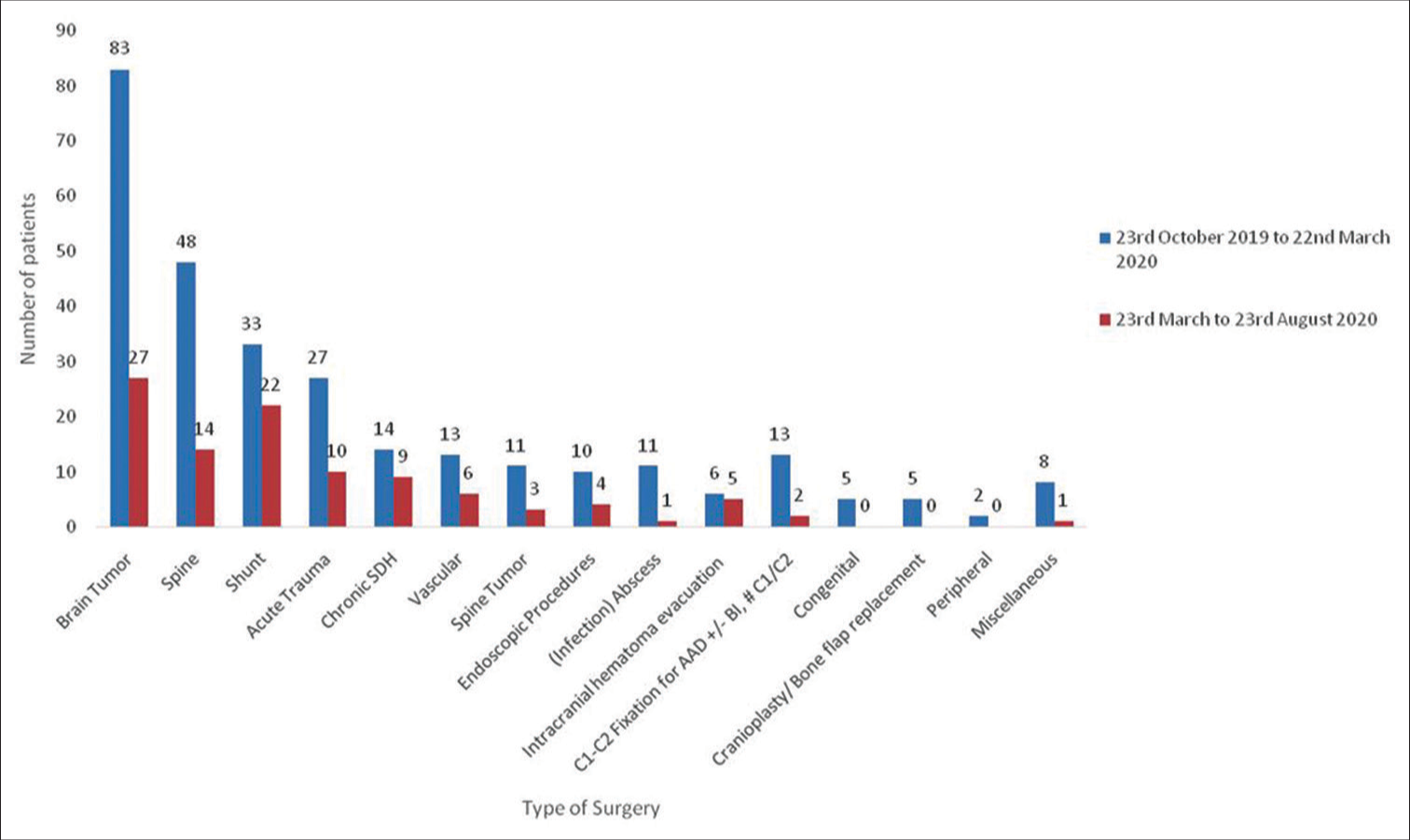
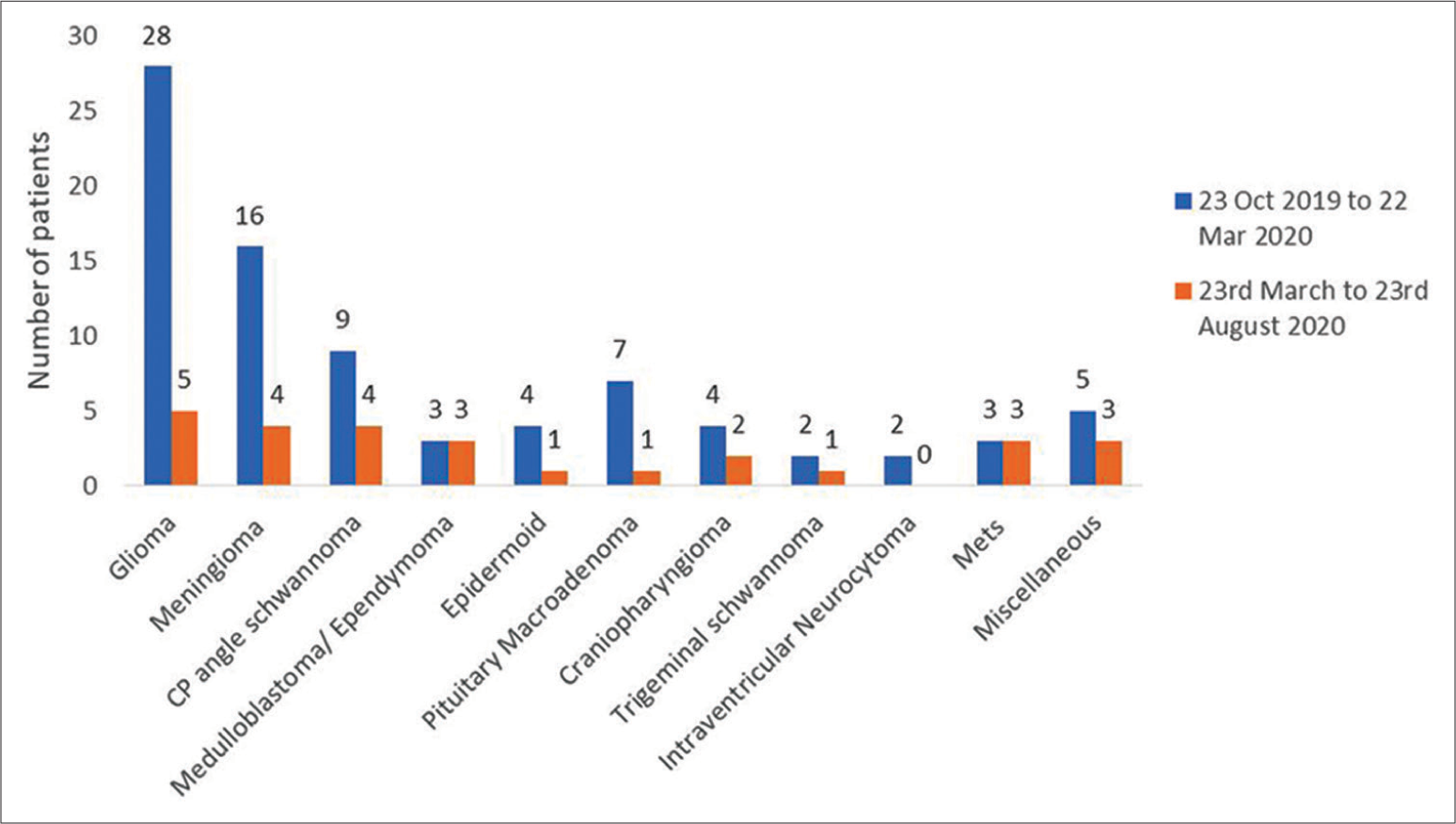
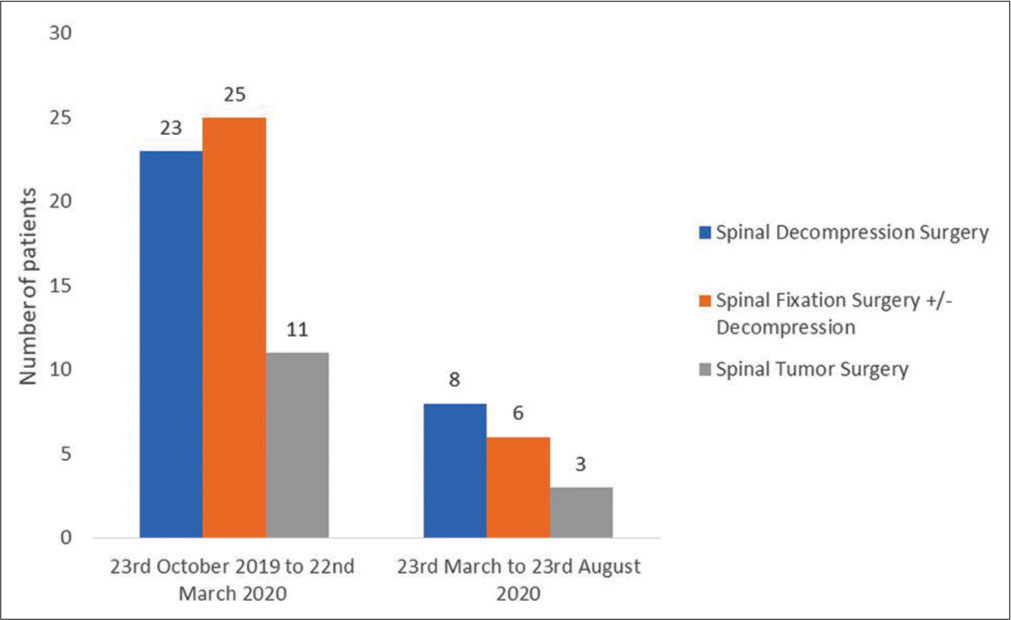
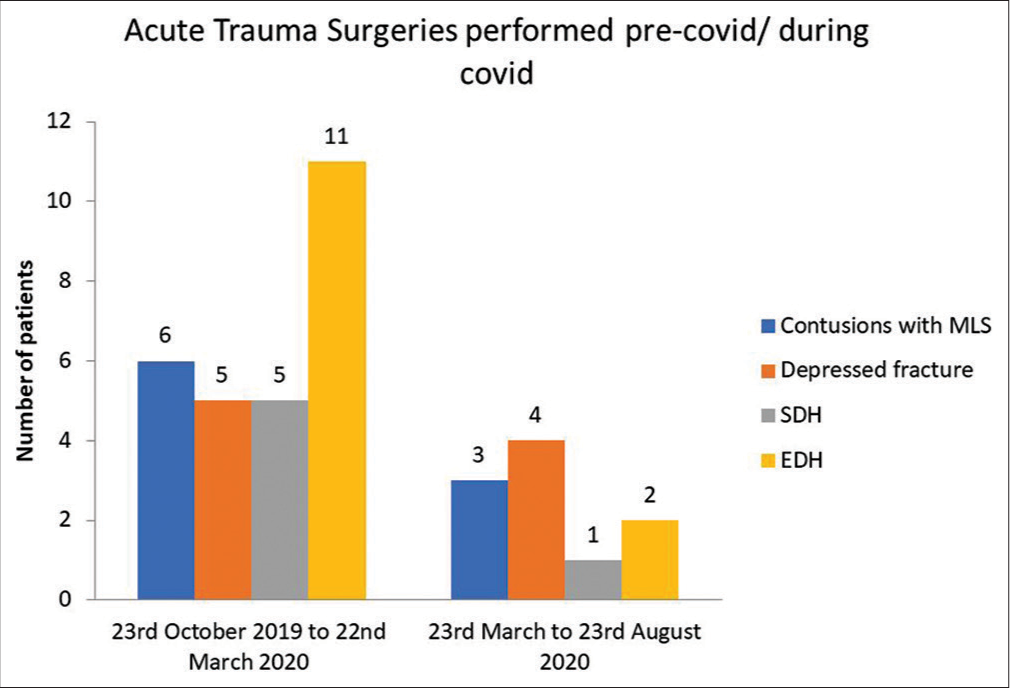
We collected data retrospectively of all patients who were operated at our institute under the department of neurosurgery from October 23, 2019, to August 23, 2020 (total 10 months duration). These data were then divided into two groups – pre-COVID period (October 23, 2019– March 22, 2020 – 5 months) and during the COVID pandemic (March 23, 2020–August 23, 2020 – 5 months). The diagnosis, surgeries performed, their nature – major or minor, routine or emergency, cranial, or spinal was compared between the two groups. The groups were further subdivided into various categories (CSF diversion procedures, acute neurotrauma, neuro-oncology [brain and spinal tumors], congenital, peripheral, neurovascular, miscellaneous, etc.) and comparison was done between the various categories of the two groups.
Data analysis was done using the Statistical Package for the Social Sciences version 26:0 (International Business Machines Corporation, New York, United States of America). Frequency and percentage (%) were used to describe the qualitative data variables. Mean and standard deviation (SD) were used to describe the quantitative data variables. Wherever applicable, an unpaired t-test was applied. Statistical significance was defined as P < 0.05.
RESULTS
A total of 388 patients underwent surgery at our institute from October 23, 2019, to August 23, 2020. Out of these, 284 patients underwent surgery during the pre-COVID period and 104 patients underwent surgery during the COVID pandemic. Out of the 284 patients that underwent surgery in the pre-COVID period, 143 were routine surgeries and 141 were emergency surgeries. During the COVID pandemic, out of the 104 surgeries performed, 84 were emergency surgeries, and 20 were routine surgeries.
Effect of COVID pandemic on operative workflow
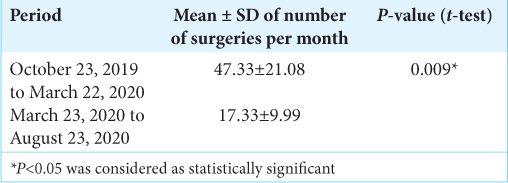
During this ongoing COVID pandemic, the total number of surgeries performed by the department of neurosurgery declined significantly by 63.38%. When the means of the number of surgeries performed per month in the pre-COVID and during the COVID period were compared using the unpaired t-test, it was found to be highly statistically significant (P = 0.009) [
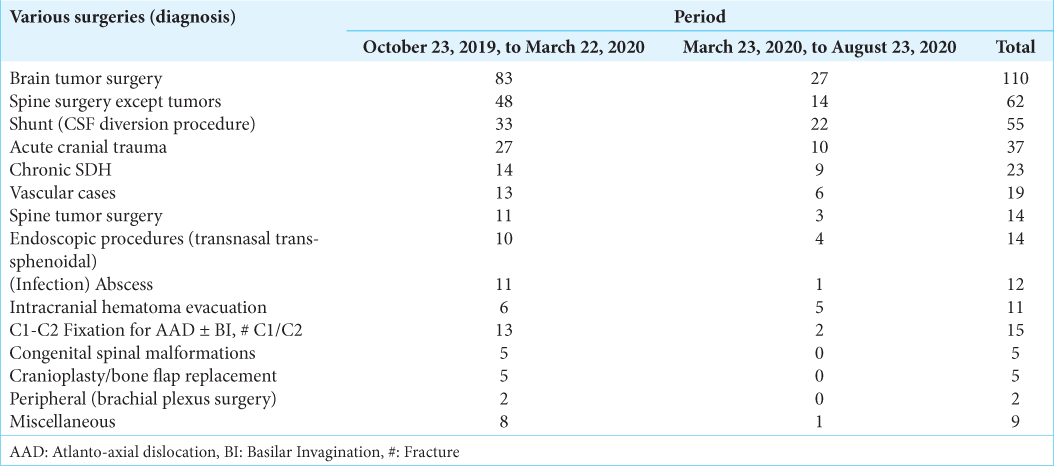
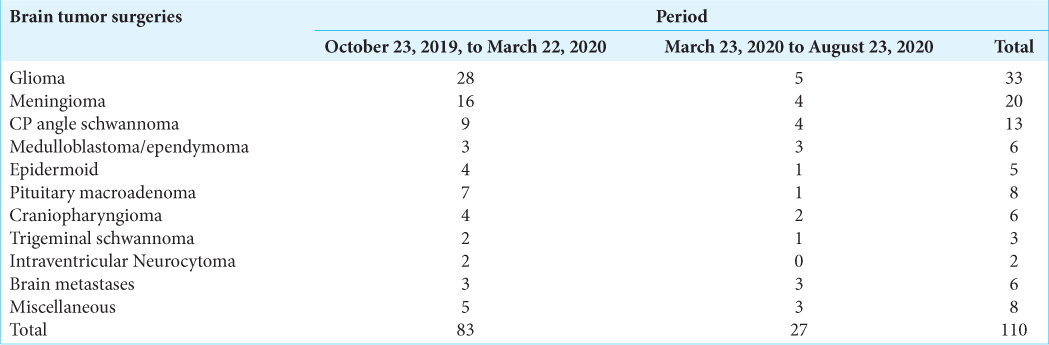
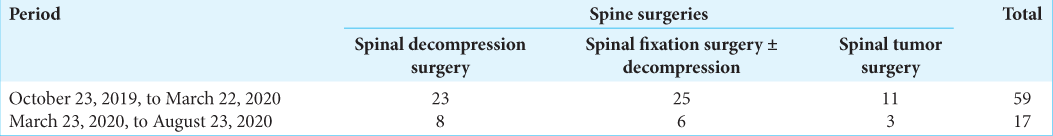
The proportion of spinal cases (compared to the preCOVID period) decreased from 27.11% to 18.27%, and the proportion of cranial cases increased from 72.89% to 81.73%. When we compare the various categories in the two groups, we noted that brain tumor surgery cases decreased from 83 in the pre-COVID period to 27 during the pandemic [
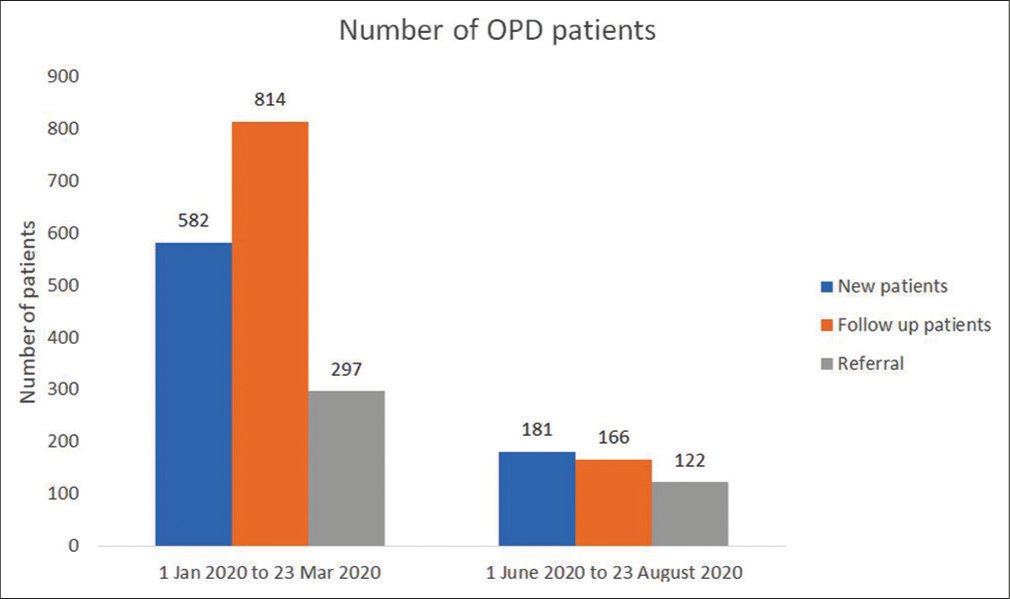
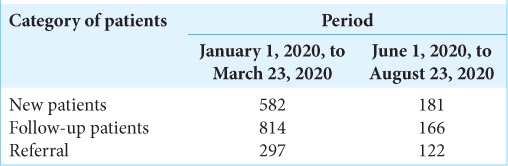
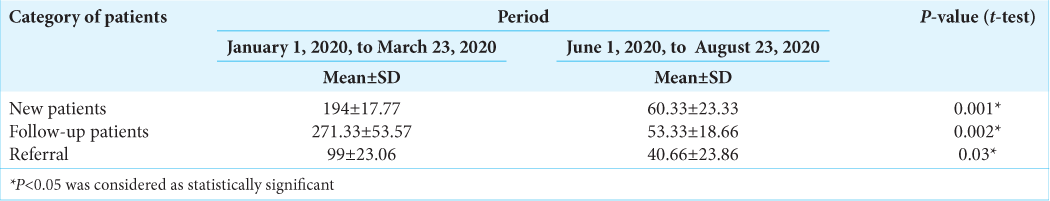
Effect of COVID pandemic on outpatient clinic workflow
We attended to 526 patients in the outpatient clinic of our hospital in November 2019, 567 patients in December 2019, 598 patients in January 2020, 620 patients in February 2020, and 475 patients in March 2020 till March 22, 2020. Our Outpatient clinics were closed from March 23, 2020, to May 31, 2020 due to the National Lockdown declared by the Indian Government. In June 2020, we attended to 77 patients in the outpatient clinic of our hospital, in July 2020, the number increased to 233, and in August 2020 (till August 23, 2020), the number stood at 159. We attended to 1693 patients during the time period from January 1, 2020, to March 22, 2020 (pre-COVID period). During the COVID pandemic, from June 1, 2020, to August 23, 2020, we attended to 469 patients (a decrease of 72.3% Outpatient Clinic Workflow as compared to the pre-COVID period) [
Management of COVID-positive neurosurgical patients
All preoperative neurosurgical patients are first admitted in the screening ward where COVID-19 reverse transcription-polymerase chain reaction (RT-PCR) test is done. The report is usually available within 24 h. COVID-19 RT-PCR negative patients are then shifted to the neurosurgery ward, while COVID-19 RT-PCR positive patients are managed in the COVID ward. COVID-19 RT-PCR test is repeated again just before surgery (within 48 h) to reconfirm COVID-19 negative status. As of August 30, 2020, 13 neurosurgery patients have tested COVID-19 RT-PCR positive in the perioperative period. The perioperative COVID-19 RT-PCR positive incidence in neurosurgical patients at our institute, as of now, is 11.71%. Out of these 13 positive patients, only two patients were operated immediately in COVID-19 designated operation theaters as life-saving emergency surgeries (COVID-19 RT-PCR report came positive in the postoperative period) under full personal protective equipment cover. The remaining 11 patients were operated only after 2 COVID-19 RT-PCR swabs came negative. There was 1 mortality out of these 13 positive patients – a young male who presented to the emergency after a road traffic accident (RTA) with a Glasgow Coma Scale score of 6 (E1M4V1), hypovolemic shock, and radiology suggestive of frontoparietal depressed fracture with tentorial SDH with fracture femur, mandible, and multiple ribs. Out of these 13 positive patients, one re-positive case was also identified (a case of metastatic round cell tumor who was COVID-19 RT-PCR positive in June 2020, negative in July 2020, and then again COVID-19 RT-PCR positive after 6 weeks).
DISCUSSION
In this paper, we have presented the experience of our neurosurgery department during the ongoing COVID-19 pandemic by observing how and to what degree the workflow in hospitals has changed. Although there is a worldwide consensus to cut down on “elective” neurosurgical operations, we have to be equally vigilant to decrease the harm caused to the patients due to the delay of elective neurosurgical procedures.[
We started using telemedicine consultations for outpatient appointments that did not require in-person care. The use of telemedicine services and the reluctance of patients and their relatives to visit a facility catering to both COVID and nonCOVID patients (though in separate blocks) has resulted in a decrease of 72.3% Outpatient Clinic Workflow as compared to the pre-COVID period.
All new admissions are treated as asymptomatic carriers, and nonemergency surgical procedures are conducted only after a negative COVID-19 RT-PCR test. Nonemergency surgery for those who test positive for COVID-19 infection is postponed until 2 COVID-19 RT-PCR swabs come negative. This is backed by data from a recent article showing that 30-day mortality of elective and emergency surgeries was 23.8% in patients with perioperative COVID-19 infection and that pulmonary complications were seen in 51.2% of the cases.[
Our operative workflow has also significantly decreased. There are many factors responsible for this decrease. Our faculty, residents, and nursing officers have been partially reassigned to COVID wards to help in the care and treatment of patients infected with COVID-19. As the severity of the pandemic is increasing in India, more and more wards in our institute are getting converted to COVID wards, thus reducing the number of beds available for routine neurosurgery work. Non-essential elective surgeries have been restricted. During this ongoing corona pandemic, we found a substantial reduction in neurosurgical emergencies as compared to the pre-COVID era. This could be explained by the national lockdown and the decrease in RTAs including cranial/spinal trauma. The patients and their relatives are also reluctant to seek medical help at a facility that caters to both, COVID and non-COVID patients. All these factors have been responsible for decreasing the operative workflow of our department by 63.38%.
Goyal et al., in their paper, reported that there was a 52.2% reduction in the number of neurosurgeries performed during the COVID pandemic as compared to the pre-COVID era at All India Institute of Medical Sciences, Rishikesh, India.[
Aerosol generating procedures such as transnasal transsphenoidal endoscopic surgeries and surgeries that involve extensive bone drilling, including skull-base surgeries, pose the highest risk for neurosurgeons to get infected with the COVID-19 virus.[
The authors strongly suspect that the current COVID-19 health crisis will result in major collateral damages due to the delay in consultation, the failure to diagnose and treat some of the neurosurgical disorders at an early stage, and the presentation of postponed elective cases at a later date with a more advanced disease once the COVID pandemic is over. Moreover, how to deal with the acute surge of accumulated operative cases at the end of the pandemic is an unanswered question at this time.
CONCLUSION
This paper highlights the drastic reduction in the operative workflow and the outpatient clinic workflow during the ongoing corona pandemic at a tertiary health-care institute which will have significant collateral damages in the long run. Every patient presenting for treatment should be considered a probable asymptomatic infected case unless proven otherwise. The current situation demands that neurosurgeons strike the right balance between providing their patients with the best medical treatment while limiting the spread of the COVID-19 infection.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Burks JD, Luther EM, Govindarajan V, Shah AH, Levi AD, Komotar RJ. Early changes to neurosurgery resident training during the Covid-19 pandemic at a large U.S. academic medical center. World Neurosurg. 2020. p.
2. CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures during COVID-19 Response. Available from: https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental [Last accessed on 2020 Aug 30].
3. Coronavirus Outbreak in India. Available from: https://www.covid19india.org/state/CT [Last accessed on 2020 Aug 30].
4. . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet. 2020. 396: 27-38
5. Fontanella MM, De Maria L, Zanin L, Saraceno G, Di Bergamo LT, Servadei F. Neurosurgical practice during the severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) pandemic: A worldwide survey. World Neurosurg. 2020. 139: e818-26
6. Galarza M, Gazzeri R. Letter: Collateral pandemic in face of the present COVID-19 pandemic: A neurosurgical perspective. Neurosurgery. 2020. 87: E186-8
7. Goyal N, Venkataram T, Singh V, Chaturvedi J. Collateral damage caused by COVID-19: Change in volume and spectrum of neurosurgery patients. J Clin Neurosci. 2020. 80: 156-61
8. Gupta P, Muthukumar N, Rajshekhar V, Tripathi M, Thomas S, Gupta SK. Neurosurgery and neurology practices during the novel COVID-19 pandemic: A consensus statement from India. Neurol India. 2020. 68: 246-54
9. Hoz SS, Al-Sharshahi ZF, Albanaa SA. Neurosurgery in Iraq at the time of corona. Surg Neurol Int. 2020. 11: 103
10. Jean WC, Ironside NT, Sack KD, Felbaum DR, Syed HR. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: A global neurosurgery study. Acta Neurochir. 2020. 162: 1229-40
11. Lee ZD, Yeu DL, Ang BT, Ng WH, Seow WT. Editorial, COVID-19 and its impact on neurosurgery: Our early experience in Singapore. J Neurosurg. 2020. 1: 1-2
12. Lo YT, Teo NW, Ang BT. Editorial, Endonasal neurosurgery during the COVID-19 pandemic: The Singapore perspective. J Neurosurg. 2020. 1: 1-3
13. Nepogodiev D, Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br J Surg. 2020:
14. Reid D. India Confirms Its First Coronavirus Case. Available from: https://www.cnbc.com/2020/01/30/india-confirms-first-case-of-the-coronavirus.html [Last accessed on 2020 Aug 30].
15. Reported Cases and Deaths by Country, Territory, or Conveyance. Available from: https://www.worldometers.info/coronavirus/#countries [Last accessed on 2020 Aug 30].
16. Rothrock RJ, Maragkos GA, Schupper AJ, McNeill IT, Oermann EK, Yaeger KA. By the numbers analysis of effect of COVID-19 on a neurosurgical residency at the epicenter. World Neurosurg. 2020. 142: e434-9
17. Saad H, Alawieh A, Oyesiku N, Barrow DL, Olson J. Sheltered neurosurgery during COVID-19: The Emory experience. World Neurosurg. 2020:
18. Tomlinson SB, Hendricks BK, Cohen-Gadol AA. Editorial, Innovations in neurosurgical education during the COVID-19 pandemic: Is it time to reexamine our neurosurgical training models?. J Neurosurg. 2020. 133: 1-2
19. Twitter. Available from: https://www.twitter.com/covid19indiaorg/status/1300296604910411776 [Last accessed on 2020 Aug 30].
20. Venkataram T, Goyal N, Dash C, Chandra PP, Chaturvedi J, Raheja A. Impact of the COVID-19 pandemic on neurosurgical practice in India: Results of an anonymized national survey. Neurol India. 2020. 68: 595-602