- Department of Anaesthesia and Intensive Care, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
DOI:10.25259/SNI_576_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Deepika Jain, Hemant Bhagat, Divya Jain. Effect of intravenous lignocaine infusion on the quality of emergence in patients undergoing transsphenoidal resection of pituitary tumors – A prospective, randomized controlled trial. 20-Jun-2020;11:154
How to cite this URL: Deepika Jain, Hemant Bhagat, Divya Jain. Effect of intravenous lignocaine infusion on the quality of emergence in patients undergoing transsphenoidal resection of pituitary tumors – A prospective, randomized controlled trial. 20-Jun-2020;11:154. Available from: https://surgicalneurologyint.com/surgicalint-articles/10089/
Abstract
Background: Emergence from anesthesia is a critical step in patients undergoing transsphenoidal pituitary surgery (TSS). The cough suppressant and anesthetic sparing properties of lignocaine makes it a favorable option for smooth extubation and maintaining stable hemodynamics intraoperatively. We aimed to evaluate the effect of lignocaine infusion on the quality of emergence (QOE) and intraoperative hemodynamics in patients undergoing transsphenoidal resection of pituitary tumors.
Methods: Fifty patients scheduled to undergo TSS were randomly divided into ligocaine group (n = 25), receiving 1.5 mg/kg bolus dose of lignocaine followed by continuous infusion of 1.5 mg/kg/h and saline group (n = 25). Patients assigned to the control group received equal volume of saline receiving equal volume of saline. The four emergence parameters (mean arterial pressure [MAP], heart rate (HR), cough, and agitation) were abbreviated into an aggregated score for QOE. Time to emergence and intraoperative hemodynamics were also recorded.
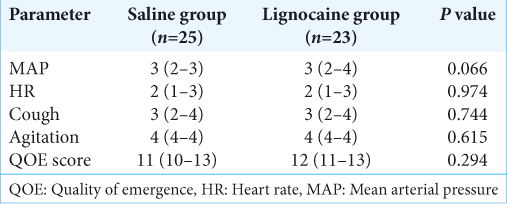
Results: The QOE was not found to be different between the two groups (P = 0.294). Lignocaine did not increase the time to emergence (P = 0.166). The intraoperative HR and MAP were comparable between the two groups. A lower minimum alveolar concentration of desflurane was required in lignocaine group during insertion of nasal speculum (P = 0.018) and at the time of seller ridge dissection (P = 0.043) compared to the saline group.
Conclusion: Intraoperative lignocaine infusion of 1.5 mg/kg/h did not significantly improve the QOE with respect to hemodynamics, cough, and emergence agitation in patients undergoing transsphenoidal resection of pituitary tumors.
Keywords: Lignocaine infusion, Quality of emergence, Transsphenoidal pituitary surgery
INTRODUCTION
The anesthetic management of patients undergoing transsphenoidal pituitary surgery (TSS) offers mydriad of challenges. The high occurrence of associated cardiovascular disorders such as hypertension, and coronary artery disease makes them susceptible to perioperative cardiac events especially during the periods of stress.[
Emergence from anesthesia is a critical phase in patients of TSS. To ensure smooth emergence various techniques such as deep plane extubation,[
Recently, there has been growing interest in combining local anesthetics with general anesthesia. Lignocaine as an adjuvant to general anesthesia has been shown to have anesthetic sparing effect.[
Considering these properties of lignocaine and the anesthetic goals of TSSs, we aimed to evaluate the effect of lignocaine on the quality of emergence (QOE) in patients undergoing transsphenoidal resection of pituitary tumors. The effects of lignocaine on intraoperative hemodynamic stability and its sparing effect on volatile anesthetic agents were also evaluated.
MATERIALS AND METHODS
The study was conducted at Post Graduate Institute for Medical Education and Research, Chandigarh, after obtaining approval from the Institute’s Ethics Committee (NK/792/MD/1569-70 under Chairmanship of Dr KL Gupta on 20.3.2013) and written informed consent. Fifty ASA 1 and 2 patients, between 18 and 65 years scheduled to undergo transsphenoidal resection of pituitary tumors were enrolled for the study. Patients with reported adverse reactions to lignocaine or other amide local anesthetic agent, those on concurrent treatment with Class 1 anti-arrhythmic drugs, having history of renal or liver insufficiency, heart block or arrhythmias, or undergoing revision surgery for pituitary tumor were excluded from the study.
Anesthesia protocol
All the patients received tablet alprazolam 0.25 mg on the night before surgery and tablet ranitidine 150 mg and tablet metoclopramide 10 mg 2 h before surgery as premedication. Patients were fasted according to nil per os guidelines. Intraoperative monitoring included continuous electrocardiography, pulse oximetry, end tidal carbon dioxide, non-invasive and invasive blood pressure, minimum alveolar concentration (MAC), and neuromuscular monitoring. The depth of anesthesia was measured using bispectral index (BIS).
General anesthesia was induced with morphine 0.1 mg/kg, propofol 1% bolus till loss of verbal response to commands and/or a BIS value <40. Vecuronium 0.1 mg/kg was given after checking ventilation to facilitate tracheal intubation. A throat pack was inserted after intubation. Patients were mechanically ventilated to attain normocapnia. Anesthesia was maintained with oxygen-nitrous oxide-desflurane. The concentration of desflurane was titrated to achieve BIS values between 40 and 60. Vecuronium was administered to maintain a TOF count between 1 and 2. Normothermia was attained for all patients. Intravenous diclofenac (2 mg/kg) and ondansetron (4 mg) were administered to all patients 30 min prior end of surgery.
Study protocol
Patients were randomized into two groups – lignocaine group (n = 25) and saline group (n = 25) using computer generated number table. The random number was enclosed in sealed opaque envelopes. After shifting the patient into operating room, the sealed envelope was opened by an anesthetic not involved in the study to prepare the drug for infusion according to randomization. Patients assigned to lignocaine group received an intravenous bolus of preservative free lignocaine (1% preparation) of 1.5 mg/kg just before induction of anesthesia with a subsequent continuous infusion of 1.5 mg/kg/h. Patients assigned to the control group received equal volume of saline. The hemodynamic parameters (heart rate [HR] and mean arterial pressure [MAP]), BIS, and MAC values were recorded at predetermined time intervals during preinduction (T1), postinduction (T2), postintubation (for first 5 min) (T3), during infiltration of nasal mucosa with solution of lignocaine and adrenaline (T4), during insertion of Hardy’s self-retaining nasal speculum (T5), at the time of sphenoid bone (T6), and seller ridge dissection (T7), during switching off the anesthetic agents (T8), at the time of extubation and every 5 min after extubation for 30 min.
The aim was to maintain hemodynamic parameters (MAP and HR) within 20% of baseline values. Any deviation from this was classified as hypertension (MAP >20% above baseline) or hypotension (MAP <20% below baseline) and tachycardia (HR >20% above baseline) or bradycardia (HR <40 bpm). Hypertension and/or tachycardia were treated with 1 μg/kg of intravenous fentanyl, if BIS was within the study range. Patients not responding to fentanyl were given esmolol 0.5–1 mg/kg as required. Hypotensive episodes were managed primarily with crystalloids, and 3 mg of i.v. mephentermine, if required. Atropine (0.5 mg) was used for bradycardia associated with hypotension.
All the anesthetic agents including desflurane, nitrous oxide, and drug infusion were stopped after the completion of surgery and packing of the nose. Residual neuromuscular blockade was reversed using neostigmine and glycopyrrolate after return of spontaneous respiratory effort. Tracheal extubation was performed after the patient responded to verbal commands, demonstrated purposeful movement and had adequate spontaneous respiration.
Time to emergence was defined as the period from switching off of anesthetic agents till tracheal extubation. Maximum MAP and HR attained during this period was recorded as emergence MAP and HR, respectively. ΔMAP (emergence MAP – baseline MAP) and ΔHR (emergence HR – baseline HR) were calculated as the difference between the emergence and baseline parameters. Percentage (%) increase in MAP and HR was also determined.
Patients with percentage increase in MAP ≥20% or those with emergence MAP >120 mmHg were treated with i.v. esmolol 0.5 mg/kg.
Cough during emergence was classified as (none-no cough; mild-single cough; moderate -more than one bout but unsustained that is <5 s cough; severe-sustained, and >5 s bouts of cough).[
The four emergence parameters (MAP, HR, cough, and agitation) were abbreviated into an aggregated score for QOE [
Statistical analysis
The statistical analysis was carried out using Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, version 15.0 for Windows). Mean and medians were calculated for all quantitative variables and for measures of dispersion, standard deviation or standard error were calculated. Normality of data was checked by measures of Kolmogorov–Smirnov tests of normality. For normally distributed data, means of two groups were compared using t-test. For skewed data, Mann–Whitney test was applied. Qualitative or categorical variables were described as frequencies and proportions. Proportions were compared using Chi-square or Fisher’s exact test, whichever was applicable. For comparison of time related variables, repeated measure ANOVA followed by one-way ANOVA was applied. All statistical tests were two-sided and were performed at a significance level of α = 0.05.
Sample size was estimated based on total QOE score of 16. To detect a 4 point increase in the emergence score with the use of lignocaine when compared to placebo with SD of 4, the calculated sample size was 22 per group at a power of 90% and confidence interval of 95%. For possible dropouts, it was decided to include 25 patients per group. The effect size would be one.
RESULTS
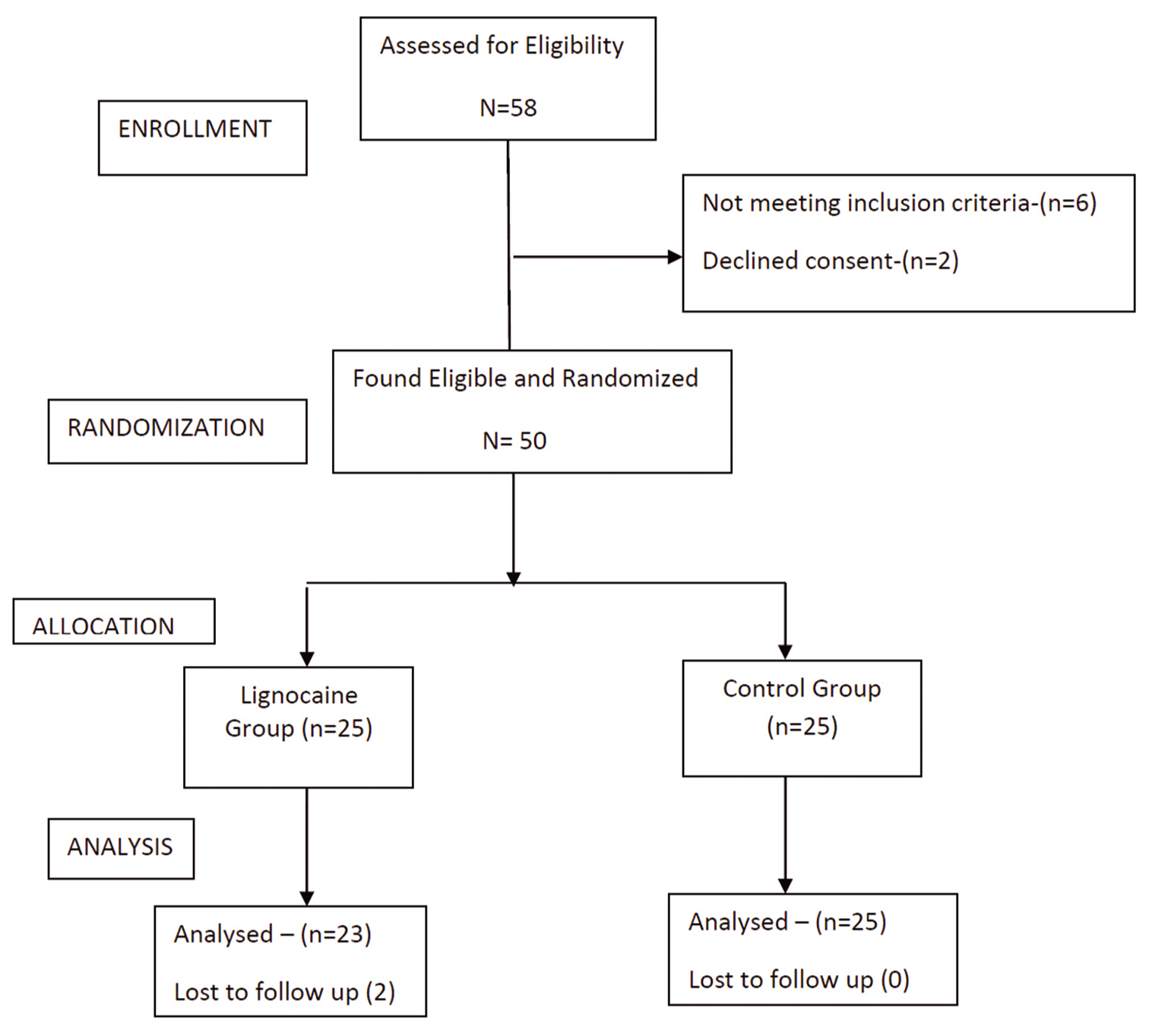
A total of 58 patients were screened for eligibility, two did not meet inclusion criteria and two patients refused consent. Out of 50 patients randomized in the study, 23 patients in the lignocaine group and 25 in the saline group completed the study. Two patients in the lignocaine group were excluded from the study. One had severe bradycardia not responding to treatment protocol and hence required cessation of the drug infusion. The other was not extubated at the end of the surgery due to a surgical complication. [
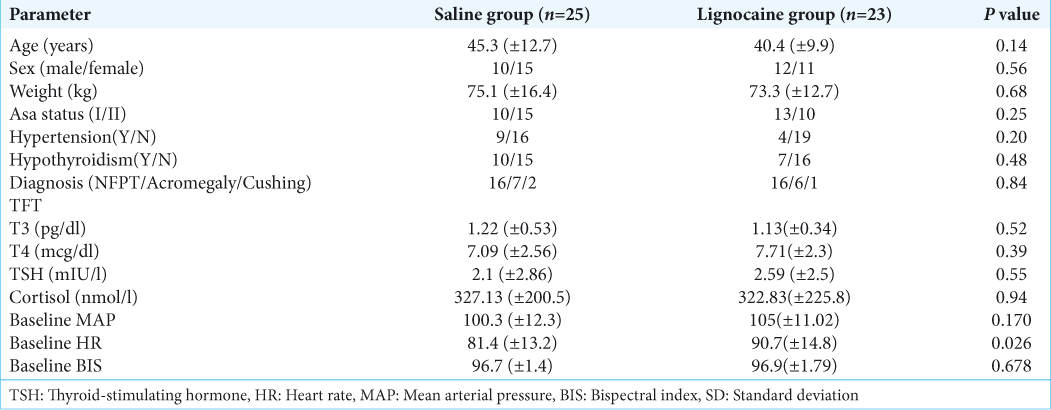
The baseline patient demographics and characteristics are presented in [
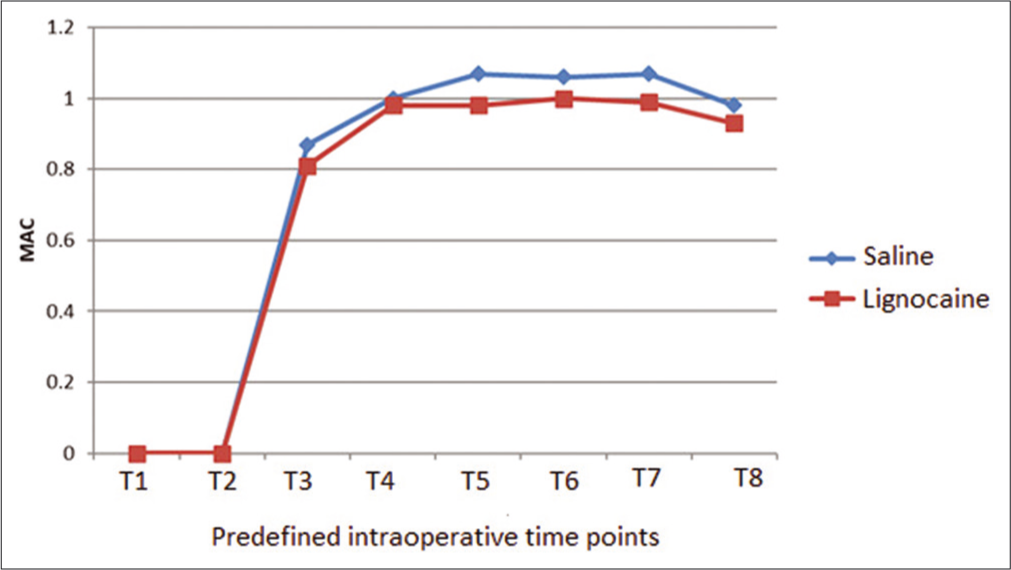
Intraoperatively, the blood pressure was maintained close to the target (within 20% of baseline) more effectively among the lignocaine group as compared to the saline group. Fentanyl was required in only three patients of lignocaine group while eight patients required the drug in saline group to achieve this target. Esmolol which was the second-line antihypertensive agent was also required more frequently in the saline group (five as compared to one). The intraoperative HR and blood pressure were comparable between the two groups. A lower MAC of desflurane was required to maintain adequate depth in lignocaine group as compared to the saline group. This difference was particularly significant at two stages: during insertion of nasal speculum (0.98 ± 0.11 vs. 1.07 ± 0.11; P = 0.018) and at the time of seller ridge dissection (0.99 ± 0.12 vs. 1.07 ± 0.12; P = 0.043) [
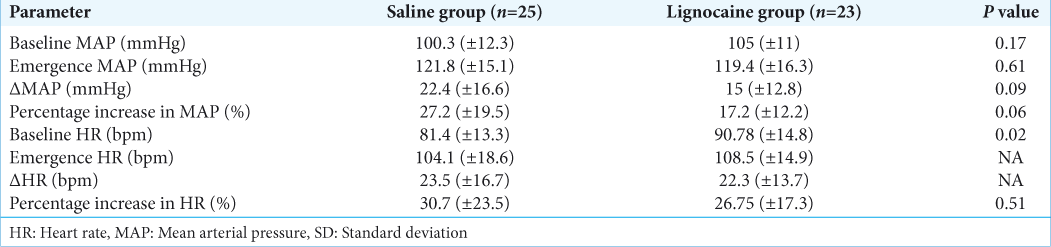
At emergence, the MAP was higher in the saline group compared to the lignocaine group as was the ΔMAP. Furthermore, the % increase in MAP was higher in the saline group. As a result, esmolol was required less frequently at emergence in the lignocaine group (11 patients [47.8%] in the lignocaine group required the drug while 17 patients (68%) required it in the saline group). The % increase in HR was comparable between the two groups [
The QOE score which was an aggregate of emergence MAP, HR, cough, and agitation was however not found to be different between the two groups. Contrary to the hypothesis, lignocaine did not increase the time to emergence (12.1 ± 5.6) min in saline group versus 10.0 ± 4.7 min; (P = 0.166). Postextubation parameters were comparable between the two groups [
DISCUSSION
In this prospective, randomized, double-blind study, we found that intraoperative use of intravenous lignocaine at 1.5 mg/kg/h did not significantly improve the QOE with respect to hemodynamics, incidence of coughing, and emergence agitation. However, lesser number of patients in the lignocaine group required antihypertensive agents in the perioperative period to maintain blood pressure within 20% of baseline. There was a slight decrease in the requirement of volatile anesthetic desflurane. Contrary to the hypothesis, lignocaine did not prolong the time to emergence from anesthesia. The postextubation hemodynamics were found to be comparable between the two groups.
Emergence from anesthesia is a challenge in all patients of neurosurgery as rapid and smooth awakening is desirable. Various studies have been conducted but none with conclusive results.[
Multiple studies have been conducted to assess the QOE using parameters such as blood pressure, HR, severity of cough, emergence agitation, and respiratory complications such as bronchospasm, laryngospasm, desaturation, and emergence time;[
It was found that the QOE was not different in patients receiving lignocaine as compared to those given saline. So far, the effect of lidocaine has been evaluated individually on the hemodynamics, cough response, and emergence agitation and there have been conflicting reports on its efficacy. In a previous study conducted by Lee et al.,[
Looking at individual parameters at emergence, it was found that the percentage increase in MAP was higher in the saline group. Hence, more number of patients in saline group required esmolol at emergence (to maintain MAP within 20% of baseline). The emergence HRs were however comparable. Mraovic et al. found that intravenous lignocaine given before extubation, did suppress the cough on emergence.[
Similarly, there was no difference in emergence agitation in between the two groups in the present study. There are studies which have shown that intravenous lidocaine does not reduce emergence agitation.[
Therefore, despite resulting in reduced blood pressure, lidocaine could not holistically contribute to each parameter measuring quality of extubation encompassing hemodynamics, cough response, and emergence agitation in summation.
In conflicting reports by Mraovic et al.[
Intraoperatively, MAP was maintained within 20% of baseline more effectively in patients of lignocaine group with lesser requirement of both fentanyl and esmolol. This difference was prominent at certain points of intense stimulation during surgery like at the time of adrenaline infiltration and insertion of nasal speculum. This is consistent with a study by Hans et al.[
CONCLUSION
Our study states that 1.5 mg/kg/h of intraoperative lignocaine infusion did not significantly improve the QOE with respect to hemodynamics, cough, and emergence agitation in patients undergoing transsphenoidal resection of pituitary tumors. Further studies with larger sample size and increasing doses of lignocaine with monitoring of plasma lignocaine levels are required to definitely conclude its role in blunting the airway-circulatory responses at the time of extubation. Using other short acting agents such as opioids, beta-blockers in addition to lignocaine may also improve the outcome as compared to either agent alone.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Ali Z, Prabhakar H, Bithal PK, Dash HH. Bispectral index-guided administration of anesthesia for transsphenoidal resection of pituitary tumors: A comparison of 3 anesthetic techniques. J Neurosurg Anesthesiol. 2009. 21: 10-5
2. Altermatt FR, Bugedo DA, Delfino AE, Solari S, Guerra I, Munoz HR. Evaluation of the effect of intravenous lidocaine on propofol requirements during total intravenous anaesthesia as measured by bispectral index. Br J Anaesth. 2012. 108: 979-83
3. Aouad MT, Al-Alam AA, Nasr VG, Souki FG, Zbeidy RA, Siddik-Sayyid SM. The effect of low-dose remifentanil responses to the endotracheal tube during emergence from general anaesthesia. Anesth Analg. 2009. 108: 1157-60
4. Bajwa SS, Bajwa SK. Anesthesia and intensive care implications for pituitary surgery: Recent trends and advancements. Indian J Endocrinol Metab. 2011. 15: S224-32
5. Christensen V, Pedersen HJ, Skovsted P. Intravenous lidocaine as a suppressant of persistent cough caused by bronchoscopy. Acta Anaesth Scand. 1978. p. S84-6
6. Dzikiti TB, Hellebrekers LJ, Dijk PV. Effect of intravenous lidocaine on isoflurane concentration, physiological parameters, metabolic parameters and stress related hormones in horses undergoing surgery. J Vet Med A Physiol Pathol Clin Med. 2003. 50: 190-5
7. Hans GA, Lauwick SM, Kaba A, Bonhomme V, Struys MM, Hans PC. Intravenous lidocaine infusion reduces bispectral index-guided requirements of propofol only during surgical stimulation. Br J Anaesth. 2010. 105: 471-9
8. Himes RS, Di Fazio CA, Burney RG. Effects of lidocaine on the anesthetic requirements for nitrous oxide and halothane. Anesthesiology. 1977. 47: 437-40
9. Jang YH, Oh SR. Intravenous lidocaine does not reduce emergence agitation or pain after sevoflurane anesthesia in children. Korean J Anesthesiol. 2005. 49: 514-8
10. Koga K, Asai T, Vaughan RS, Latto IP. Respiratory complications associated with tracheal extubation. Timing of tracheal extubation and use of the laryngeal mask during emergence from anaesthesia. Anaesthesia. 1998. 53: 540-4
11. Lee JH, Koo BN, Jeong JJ, Kim HS, Lee JR. Differential effects of lidocaine and remifentanil on response to the tracheal tube during emergence from general anaesthesia. Br J Anaesth. 2011. 106: 410-5
12. Lin BF, Ju DT, Cherng CH, Hung NK, Yeh CC, Chan SM. Comparison between intraoperative fentanyl and tramadol to improve quality of emergence. J Neurosurg Anesthesiol. 2012. 24: 127-32
13. Mraovic B, Simurina T, Mikulandra S, Seric J, Sonicki Z. Effects of i.v lidocaine administered prior to extubation on early and late recovery after breast surgery. Eur J Anaesthesiol. 2010. 27: 8-
14. Patel RI, Hannallah RS, Norden J, Casey WF, Verghese ST. Emergence airway complications in children: A comparison of tracheal extubation in awake and deeply anesthetized patients. Anesth Analg. 1991. 73: 266-70
15. Sadegi M, Firozian A, Ghafari MH, Esfehani F. Comparison in effect of intravenous alfentanil and lidocaine on airway-circulatory reflexes during extubation. Int J Pharma. 2008. 4: 223-6
16. Sakabe T, Maekawa T, Ishikawa T, Takeshita H. The effects of lidocaine on canine cerebral metabolism and circulation related to the electroencephalogram. Anesthesiology. 1974. 40: 433-41
17. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA. The Richmond agitation-sedation scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002. 166: 1338-44
18. Shapiro HM, Galindo A, Whyte SR, Harris AB. Rapid intraoperative reduction of intracranial pressure with thiopental. Br J Anaesth. 1973. 45: 1057-62
19. Venkatesan T, Korula G. A comparative study between the effects of 4% endotracheal tube cuff lignocaine and 1.5 mg/kg intravenous lignocaine on coughing and hemodynamics during extubation in neurosurgical patients. J Neurosurg Anesthesiol. 2006. 18: 230-4