- Department of Neurosurgery, Graduate School of Medical Science, Kanazawa University, Takara-machi, Kanazawa 920-8641, Japan
Correspondence Address:
Yasuhiko Hayashi
Department of Neurosurgery, Graduate School of Medical Science, Kanazawa University, Takara-machi, Kanazawa 920-8641, Japan
DOI:10.4103/sni.sni_70_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Yasuhiko Hayashi, Issei Fukui, Yasuo Sasagawa, Kouichi Misaki, Masahiro Oishi, Mitsutoshi Nakada. Effectiveness of modified dural incision to preserve the patency of the occipital sinus in foramen magnum decompression for a patient with Chiari malformation type I. 03-Aug-2018;9:153
How to cite this URL: Yasuhiko Hayashi, Issei Fukui, Yasuo Sasagawa, Kouichi Misaki, Masahiro Oishi, Mitsutoshi Nakada. Effectiveness of modified dural incision to preserve the patency of the occipital sinus in foramen magnum decompression for a patient with Chiari malformation type I. 03-Aug-2018;9:153. Available from: http://surgicalneurologyint.com/surgicalint-articles/effectiveness-of-modified-dural-incision-to-preserve-the-patency-of-the-occipital-sinus-in-foramen-magnum-decompression-for-a-patient-with-chiari-malformation-type-i/
Abstract
Background:Foramen magnum decompression (FMD) has been acknowledged as a standard surgical procedure for symptomatic patients with Chiari malformation type I (CM-I). However, even if dural incision is necessary during FMD, the procedure of cutting off the occipital sinus has not been regarded as a safe option.
Case Description:A 27-year-old woman with intractable occipital headache was diagnosed with CM-I without syringomyelia. Preoperative examination revealed a large oblique occipital sinus on her right side. During the first FMD, the dura mater was not incised to preserve the occipital sinus. However, her headache was not relieved with painkillers and cerebellar tonsillar ectopia remained. During the second FMD, two dural incisions were made, while preserving the occipital sinus patency. The dural patch was made using an autologous fascia for both dural incisions. Postoperatively, headache was completely resolved immediately, and cerebellar tonsil was elevated without any complication.
Conclusion:This dural incision, which is a modification of the method introduced by Pritz, would be a useful FMD option for patients of CM-I with dominant occipital sinus, which would lead to the serious neurological sequelae if the sinus flow is disturbed.
Keywords: Chiari malformation, dura, foramen magnum decompression, incision, occipital sinus
INTRODUCTION
Chiari malformation type I (CM-I) is a well-known hindbrain disorder that is characterized by cerebellar tonsillar herniation behind the cervicomedullary junction, which is associated with the hypoplastic posterior cranial fossa, and often accompanied by syringomyelia.[
CLINICAL PRESENTATION
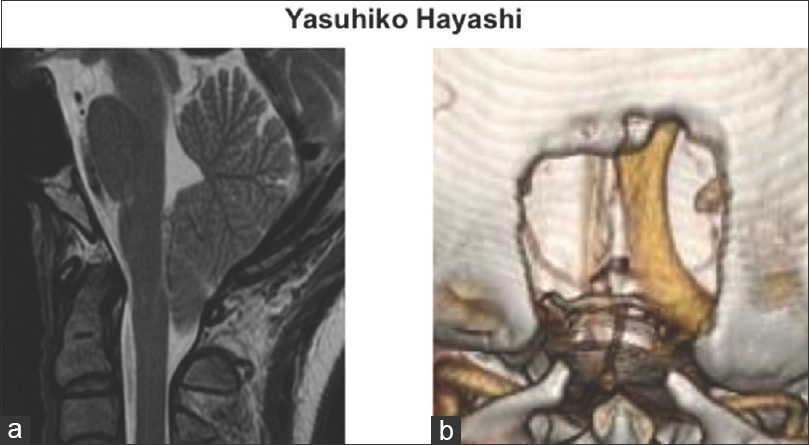
A 27-year-old woman suffered from occipital headache, which retracted downward and deteriorated when looking down. She consulted a local hospital and was diagnosed with CM-I with the use of magnetic resonance imaging (MRI) [
Figure 1
(a) Preoperative T2-weighted magnetic resonance image on the sagittal section clearly demonstrated the decent of the cerebellar tonsil and tightness of the cerebellar hemisphere in the posterior fossa. (b) The three-dimensional contrasted enhanced venography on the computed tomography scan clearly revealed the dominant occipital sinus on the right side, and undeveloped transverse and sigmoid sinuses on the same side
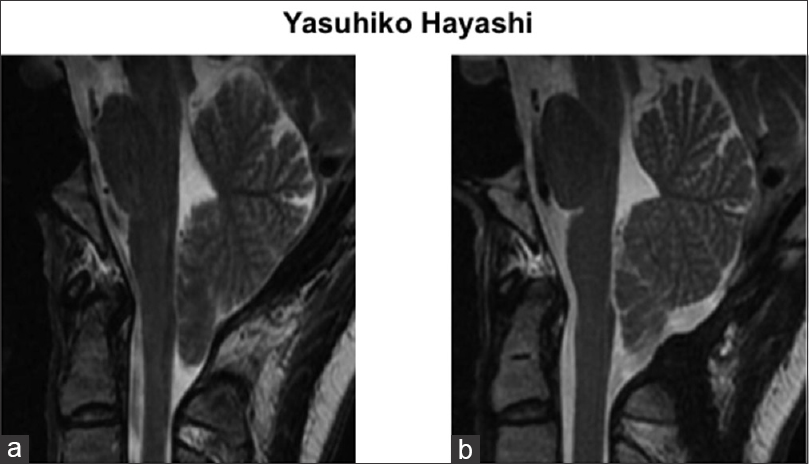
During the first FMD, dura mater was kept intact to preserve the occipital sinus after removal of the occipital bone and epidural fibrous band. However, the operation did not relieve her headache or improve cerebellar tonsillar herniation [
Figure 2
(a) Compared with the preoperative image, a T2-weighted magnetic resonance image on the sagittal section after the first foramen magnum decompression (FMD) showed no apparent change. (b) A T2-weighted MR-image of the sagittal section after the second FMD revealed the elevation of the cerebellar tonsil and opening of the retrocerebellar space over the cerebellar convexity, indicating that CM-1 findings were remarkably improved
Surgical technique during the second FMD
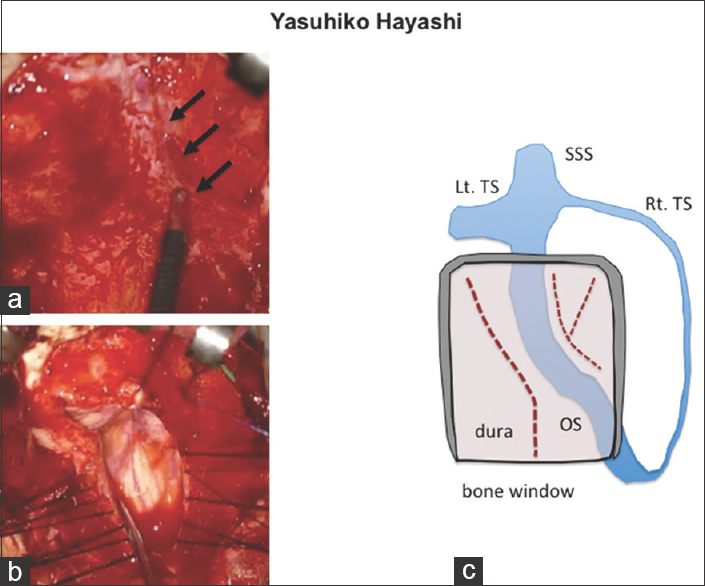
Under general anesthesia, she was placed in prone position with skeletal fixation. Intraoperative administration of antibiotics was performed routinely. A linear suboccipital skin incision from 3 cm above the inion to the level of C4 was carried down to the pericranium. The fascia was harvested from both sides to make a dural patch after undermining the occipital scalp. Then, the dura mater was exposed in a 3 × 3 cm bone window made during the previous surgery. The running course of the occipital sinus was confirmed with a micro-doppler [
Figure 3
(a) The intraoperative picture revealed the confirmation of the occipital sinus (arrows) with micro-doppler. (b) The dural incision consisted of two parts as follows: a midline incision from the level of C1 to that of the cervicomedullary junction, and an incision over the left cerebellar hemisphere. (c) The scheme of the dural incisions in the present case. OS, occipital sinus; SSS, superior sagittal sinus; TS, transverse sinus
Postoperative clinical course was uneventful; her headache was completely resolved immediately after the operation. She was discharged home and returned to her previous work. In addition, a postoperative MRI obtained 3 months after the operation revealed the elevation of the cerebellar tonsil, indicating that the findings of CM-1 had improved remarkably [
DISCUSSION
Although Y-shaped dural incisions have been performed after coagulation of the occipital sinus, during FMD for cases of CM-I with the occipital sinus, this has mostly been based on the personal experience of each surgeon. No clinical studies have investigated the safety of performing coagulation of the occipital sinus, in terms of short- and long-term neurological outcomes.
In the present case study, there was a single, large occipital sinus in the patient with CM-I, and both transverse and sigmoid sinuses on the right side were undeveloped. Therefore, the venous return in the posterior fossa was considered to be mainly dependent on the occipital sinus. Only a bony removal without dural incision was performed during the first operation. However, persistent headache following the first surgery led us to perform the modified Y-shaped dural incision with preservation of the occipital sinus. Excellent functional and radiological outcomes were obtained following the second procedure.
Pritz reported a simplified technique using a curvilinear dural incision and autologous pericranial graft on one side, avoiding the occipital sinus. Although he outlined several advantages of this technique, we believe that the most useful one was the avoidance of the occipital sinus. In our patient, this technique removed her intractable headache, without any complication leading to serious neurological deficits. Our results corroborated with Pritz,[
The occipital sinus can be found in 64.5% cases from adult cadaver study.[
The safety of the occipital sinus coagulation was considered from the viewpoint of embryological development. At the fetal developmental age of 4–5 months, five to seven venous channels originate from the primitive torcular area and from the medial portion of both transverse sinus, and communicate with the marginal sinus and the distal portion of the sigmoid sinus. They decrease in caliber and number due to diminution and fusion, with only a few prominent occipital sinuses being seen by the sixth or seventh month of gestation.[
CONCLUSION
This modified dural incision can be useful option to avoid a coagulation of a single, large occipital sinus, which seems to regulate the venous return in the posterior fossa, during FMD for patients with CM-I. Neurosurgeons should know this technique and preserve the dominant occipital sinus to avoid serious neurological deficits.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alperin N, Loftus JR, Bagci AM, Lee SH, Oliu CJ, Shah AH, Green BA. Magnetic resonance imaging-based measures predictive of short-term surgical outcome in patients with Chiari malformation Type I: A pilot study. J Neurosurg Spine. 2017. 26: 28-38
2. Arnautovic A, Splavski B, Boop FA, Arnautovic KI. Pediatric and adult Chiari malformation Type I surgical series 1955-2013: A review of demographics, operative treatment, and outcomes. J Neurosurg Pediatr. 2015. 15: 161-77
3. Beyrouti R, Mansour M, Kacem A, Zaouali J, Mrissa R. Occipital sinus thrombosis: An exceptional case report. J Stroke Cerebrovasc Dis. 2016. 25: e71-3
4. Das AC, Hassan M. The occipital sinus. J Neurosurg. 1970. 33: 307-11
5. Heiss JD, Suffredini G, Bakhtian KD, Sarntinoranont M, Oldfield EH. Normalization of hindbrain morphology after decompression of Chiari malformation Type I. J Neurosurg. 2012. 117: 942-46
6. Heiss JD, Suffredini G, Smith R, DeVroom HL, Patronas NJ, Butman JA. Pathophysiology of persistent syringomyelia after decompressive craniocervical surgery. J Neurosurg Spine. 2010. 13: 729-42
7. Kobayashi K, Suzuki M, Ueda F, Matsui O. Anatomical study of the occipital sinus using contrast-enhanced magnetic resonance venography. Neuroradiology. 2006. 48: 373-79
8. Lee HC, Lee JY, Ryu SK, Lim JM, Chong S, Phi JH. A method of posterior fossa dural incision to minimize hemorrhage from the occipital sinus: The “mosquito” method. Childs Nerv Syst. 2016. 32: 2429-2431
9. Okudera T, Huang YP, Ohta T, Yokota A, Nakamura Y, Maehata F. Development of posterior fossa dural sinuses, emissary veins, and jugular bulb: morphological and radiologic study. Am J Neuroradiol. 1994. 15: 1871-83
10. Pritz MB. Surgical treatment of Chiari malformation: Simplified technique and clinical results. Skull Base. 2003. 13: 173-7
11. Tubbs RS, Bosmia AN, Shoja MM, Loukaz M, Curé JK, Cohen-Gadol AA. The oblique occipital sinus: A review of anatomy and imaging characteristics. Surg Radiol Anat. 2011. 33: 747-49
12. Tubbs RS, Shoja MM, Loukas M. An unusual finding of the posterior cranial fossa: One case report. Ital J Anat Embryol. 2008. 113: 83-6