- Department of Surgery, Alkindy College of Medicine, University of Baghdad,
- Department of Neurosurgery, Neurosciences Hospital, Baghdad, Iraq.
- Department of Laboratory, Alyarmouk Teaching Hospital, Baghdad, Iraq.
Correspondence Address:
Bassam Mahmood Flamerz Arkawazi, Department of Surgery, Alkindy College of Medicine, University of Baghdad, Baghdad, Iraq.
DOI:10.25259/SNI_230_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Bassam Mahmood Flamerz Arkawazi1, Ahmed Al Atraqchi2, Arjan Adnan2, Shaymaa Dheyab3. Efficacy of Gamma Knife radiosurgery in the management of pituitary prolactinoma. 19-Jul-2021;12:357
How to cite this URL: Bassam Mahmood Flamerz Arkawazi1, Ahmed Al Atraqchi2, Arjan Adnan2, Shaymaa Dheyab3. Efficacy of Gamma Knife radiosurgery in the management of pituitary prolactinoma. 19-Jul-2021;12:357. Available from: https://surgicalneurologyint.com/surgicalint-articles/10981/
Abstract
Background: Gamma Knife radiosurgery (GKR) has been widely used in the management of a variety of intracranial tumors, including pituitary adenomas. Pituitary prolactinoma (Prs) is one of the most common types of these adenomas.
Methods: This prospective study included 50 patients with pituitary Prs over a period from June 2017 to June 2018 at the Neurosciences Hospital, Baghdad/Iraq. The GKR procedure was performed using the Leksell Gamma Knife® Perfexion™, 192 beams of Cobalt 60 radiation were delivered through the intact skull to the pituitary Prs.
Results: There is a significant female predominance 32 (72%). The results after 6 months of GKR showed significant improvement regarding the size of adenoma, prolactin hormone level, contrast enhancement on MRI, and medical treatment.
Conclusion: The study showed that the GKR is a safe and effective modality of treatment in the management of pituitary Prs.
Keywords: Gamma Knife, Pituitary adenoma, Prolactinoma, Stereotactic radiosurgery
INTRODUCTION
The incidence of pituitary adenomas in the autopsy series is almost 25%, but they account for only 15% of intracranial tumors in neurosurgical practice. Pituitary adenomas are classified with the most frequent being prolactinoma (Prs) and null cell adenomas, followed by growth hormone, adrenocorticotrophic hormone, and thyroid-stimulating hormone-producing adenomas. Some adenomas secrete more than 1 hormone.[
The main disadvantages of medical therapy are side effects, such as orthostatic hypotension, nausea, and vomiting. The therapeutic effect is only maintained as long as the drug is administered. After withdrawal of the drug, the prolactin hormone (PrH) level is expected to rise again and the tumor frequently reexpands. Surgery is designed for patients with intolerance to medication, those individually not responding to dopamine agonists (which constitute <10% of the cases), and those who for personal reasons reject medical treatment. Remission rates in a large series of surgically treated Prs vary between 54% and 86%.[
Aims of the study
In this study, we assessed the efficacy of Gamma Knife radiosurgery (GKR) in the management of pituitary Prs. The effect is measured by the following parameters:
Symptoms of the patients (amenorrhea and loss of libido). The PrH level. Contrast enhancement of the Prs on MRI. Medical treatment.
MATERIALS AND METHODS
This is a clinical prospective study that included 25 patients for the period from June 2017 to June 2018 in the Neurosciences Hospital, Baghdad/Iraq. All patients were referred by the endocrinologist for neurosurgical management. The inclusion criteria of the patients were as follows:
Clinical signs and symptoms, native and contrast-enhanced MRI findings, and elevated PrH levels confirming the diagnosis of Prs. All patients were on maximum or tolerable dopamine agonist therapy without a significant reduction in PrH levels or improvement in symptoms. None of the patients had a previous GKR or surgery for the Prs.
Any patient who did not fulfill the above criteria was excluded from the study.
The period of follow was 6 months. By the end of the 6th month post-GKR, clinical, radiological, laboratory, and medical treatment were reevaluated in all the patients.
This is the first trial in Iraq to assess the efficacy of GKR in the management of pituitary Prs.
GKR was performed using the Leksell Gamma Knife® Perfexion™, 192 beams of Cobalt 60 radiation are delivered through the intact skull to the pituitary adenoma. The dose of the radiation was 20–40 Gy (mean = 25)
Statistical analysis
Descriptive analysis in the form of percentage was calculated using Microsoft Office Excel Worksheet and presented in the relevant tables shown below. Chi-square test was used for statistical analysis by utilizing the Statistical Package for the Social Sciences version 17 (P < 0.05 was considered statistically significant).
RESULTS
Twenty-five patients were included in this study, 18 (72%) female and 7 (28%) male. The age of the patients ranged between 24 and 45 years (mean = 32.56), amenorrhea was present in 15/18 (83.3%) of the female patients, and loss of libido in 5/7 (71.4%) of the male patients. There was contrast enhancement of the Prs on MRI in 23/25 patients. All patients were on dopamine agonist medication.
Pre- and post-GKR differences
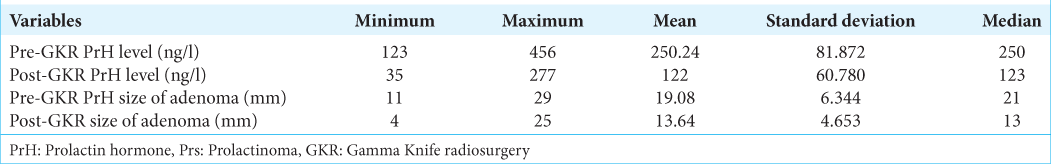
The PrH levels and the size of the Prs, pre- and post-GKR, are illustrated in [
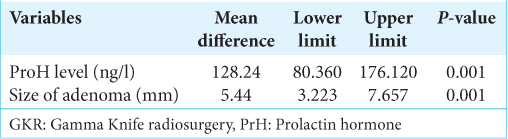
The PrH level pre- and post-GKR mean difference was 128.24 ng/l (P = 0.001) [
Regarding the size of Prs (in mm), pre- and post-GKR, the mean difference was 5.44 (P = 0.001) [
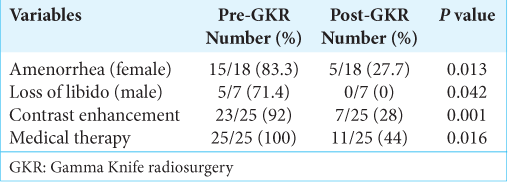
There was a statistically significant improvement in amenorrhea, loss of libido, contrast enhancement of the Prs on MRI, and need for medical treatment post-GKR [
Complications
Only 3/25 patients (12%) had transient visual deterioration that eventually improved within 2 months post-GKR.
DISCUSSION
PrH level
In our study, the pre-GKR PrH level was 123–456 ng/l (mean = 250.24 ng/l, median = 250 ng/l). The PrH level after 6 months post-GKR was 35–277 ng/l (mean = 122 ng/l). The mean difference was 128.24 ng/l (lower limit = 80.360 ng/l, and upper limit = 176.120 ng/l) which was statistically significant (P = 0.001). This improvement in the PrH level ranged from a significant reduction to complete normalization.
Other comparative studies showed variable results. Some studies showed significant improvement of patient’s PrH level after GKR. A study by Rahn et al. showed normalization of PrH level after GKR in 3/5 cases and a significant decrease in PrH in the other 2/5 cases.[
Size of adenomas
In our study, the size of pituitary adenomas was measured in the patients. The pre-GKR size of the adenomas was 11–29 mm (mean = 19.08 mm), and the post-GKR size of the adenoma was 4–25 mm (mean = 13.64 mm). The mean difference was 5.44 mm (upper limit = 3.223 mm and lower limit = 7.657 mm) which was statistically significant (P = 0.001). Other studies showed comparative results. Landolt et al. reported tumor size control in all of their cases.[
Contrast enhancement of adenoma
In this study, MRI contrast enhancement pre-GKR was present in 23/25 patients (92%), and post-GKR was present in 7/25 patients (28%). This was statistically significant (P = 0.001). Unfortunately, no other comparative studies were available in this setting.
Loss of libido and amenorrhea
In this study, amenorrhea was present in 15/18 female patients (83.3%) and loss of libido in 5/7 male patients (71.4%), preGKR. Post-GKR amenorrhea recovered in 13/18 female patients (72.3%), and all 7 male patients (100%) recovered from loss of libido. This significant clinical improvement is comparable with other study resulted by Ježková et al. and Witt et al.[
Medical treatment
Our study showed a statistically significant improvement regarding the dose of the dopamine agonist required for patients with prolactinoma post-GKR. In our study, 11/25 patients (44%) continued on medical treatment and no medical treatment was needed in the other 14/25 patients (56%). These results are comparative with other studies.[
Complications
In our study, only 3/25 patients (12%) had transient visual deterioration that eventually improved within 2 months post-GKR. This may be explained by the effect of edema and free radicals that resulted from the radiation. This finding is very comparative with the main series in this setting, and furthermore, it is better than the results of other series.[
CONCLUSION
The study provided a baseline study in Iraq for pituitary Prs treatment using the GKR. The study showed that the GKR is safe and effective modality in the management of pituitary Prs.
GKR can offer a worthwhile therapeutic option in patients with Prs who cannot achieve normal PrH levels with dopamine agonists and microsurgery. Although medical treatment is the first line in the management of pituitary Prs, and surgery is the next line, the side effects of medical management and the complications associated with surgery make the GKR a good option in the management of pituitary Prs. Future prolonged series may be required for better assessment of the discontinuation of medical treatment in patients with Prs after GKR.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asa SL.editors. Tumors of the Pituitary Gland. Atlas of Tumor Pathology. Fascicle 22. Washington DC: Armed Forces Institute of Pathology; 2009. p.
2. Fernandez A, Karavitaki N, Wass JA. Prevalence of pituitary adenomas: A community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin Endocrinol (Oxf). 2010. 72: 377-82
3. Ježková J, Hána V, Kršek M, Weiss V, Vladyka V, Liščák R. Use of the Leksell gamma knife in the treatment of prolactinoma patients. Clin Endocrinol (Oxf). 2009. 70: 732-41
4. Landolt AM, Lomax N, Haller D, Scheib S, Schubiger O, Siegfried J. Stereotactic radiosurgery for recurrent surgically treated acromegaly: Comparison with fractionated radiotherapy. J Neurosurg. 1998. 88: 1002-8
5. Laws ER, Vance ML. Radiosurgery for pituitary tumors and craniopharyngiomas. Neurosurg Clin N Am. 1999. 10: 327-36
6. Lim YL, Leem W, Kim TS, Rhee BA, Kim GK. Four years’ experiences in the treatment of pituitary adenomas with gamma knife radiosurgery. Stereotact Funct Neurosurg. 1998. 70: 95-109
7. Morange I, de Boisvilliers F, Chanson P, Lucas B, DeWailly D, Catus F. Slow release lanreotide treatment in acromegalic patients previously normalized by octreotide. J Clin Endocrinol Metab. 2014. 79: 145-51
8. Rahn T, Thoren M, Werner S, Faglia G, Beck-Peccoz P, Ambrosi B, Travaglini P, Spada A.editors. Stereotactic radiosurgery in pituitary adenomas. Pituitary Adenomas: New Trends in Basic and Clinical Research. New York: Excerpta Medica Inc.; 1991. p. 303-12
9. Sheehan JP, Starke RM, Mathieu D, Young B, Sneed PK, Chiang VL. Gamma Knife radiosurgery for the management of nonfunctioning pituitary adenomas: A multicenter study. J Neurosurg. 2013. 119: 446-56
10. Witt TC, Kondziolka D, Flickinger JC, Lunsford LD.editors. Gamma knife radiosurgery for pituitary tumors. Gamma Knife Brain Surgery. Basel: Karger Publishers; 1998. 14: 114-27
11. Wong A, Eloy JA, Couldwell WT, Liu JK. Update on prolactinomas. Part: 2 Treatment and management strategies. J Clin Neurosci. 2015. 22: 1568-74