- Department of Neurosurgery, The Jikei University Hospital, Minato-ku, Tokyo,
- Department of Neurosurgery, Japanese Red Cross Medical Center, Shibuya-ku,
- Department of Neurosurgery, The University of Tokyo Hospital, Hongo, Bunkyo-ku, Japan.
Correspondence Address:
Tomoya Suzuki, Department of Neurosurgery, The Jikei University Hospital, Nishishimbashi, Minato-ku, Tokyo, Japan.
DOI:10.25259/SNI_185_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tomoya Suzuki1, Toshikazu Kimura2, Hirotaka Hasegawa3, Koreaki Irie2, Sukwoo Hong2, Kostadin Karagiozov1, Shunsuke Ichi1. Elongated styloid process as a possible cause of distal carotid artery dissection after carotid endarterectomy using indwelling shunt: A case report. 25-Mar-2022;13:101
How to cite this URL: Tomoya Suzuki1, Toshikazu Kimura2, Hirotaka Hasegawa3, Koreaki Irie2, Sukwoo Hong2, Kostadin Karagiozov1, Shunsuke Ichi1. Elongated styloid process as a possible cause of distal carotid artery dissection after carotid endarterectomy using indwelling shunt: A case report. 25-Mar-2022;13:101. Available from: https://surgicalneurologyint.com/surgicalint-articles/11489/
Abstract
Background: A dissection beginning from a point distal to the endpoint of the carotid endarterectomy (CEA) is called distal carotid artery dissection (CAD), which is known as one of the significant surgical complications of CEA.
Case Description: We present a case of distal CAD as a perioperative complication after CEA using indwelling shunt. We estimated this pathophysiology to be caused by the mechanical conflict of the inflated balloon with the elongated styloid process.
Conclusion: Since a distal CAD can cause severe, irreversible neurological deficits, preoperative assessment of the styloid process should be routinely performed in CEA.
Keywords: Carotid artery dissection, Carotid endarterectomy, Eagle’s syndrome, Elongated styloid process
INTRODUCTION
In carotid endarterectomy (CEA), indwelling intraoperative shunt is commonly used to avoid cerebral ischemia, though the risks and benefits in applying it has long been discussed.[
Vascular Eagle syndrome is a rare condition caused by extra-arterial stress from an elongated styloid process or a calcified styloid ligament and leads to transient ischemic attacks, cerebral ischemia, or CAD.[
Here, we present a case of distal CAD as a perioperative complication after CEA using indwelling shunt, which appears to be caused by an extended styloid process.
CASE DESCRIPTION
A 69-year-old male developed gradual right hand weakness and dysarthria. He had a medical history of hypertension. Brain magnetic resonance imaging (MRI) demonstrated an acute watershed infarction in the left hemisphere. Carotid MRI and computed tomography (CT) angiography confirmed severe stenosis with marked calcification [
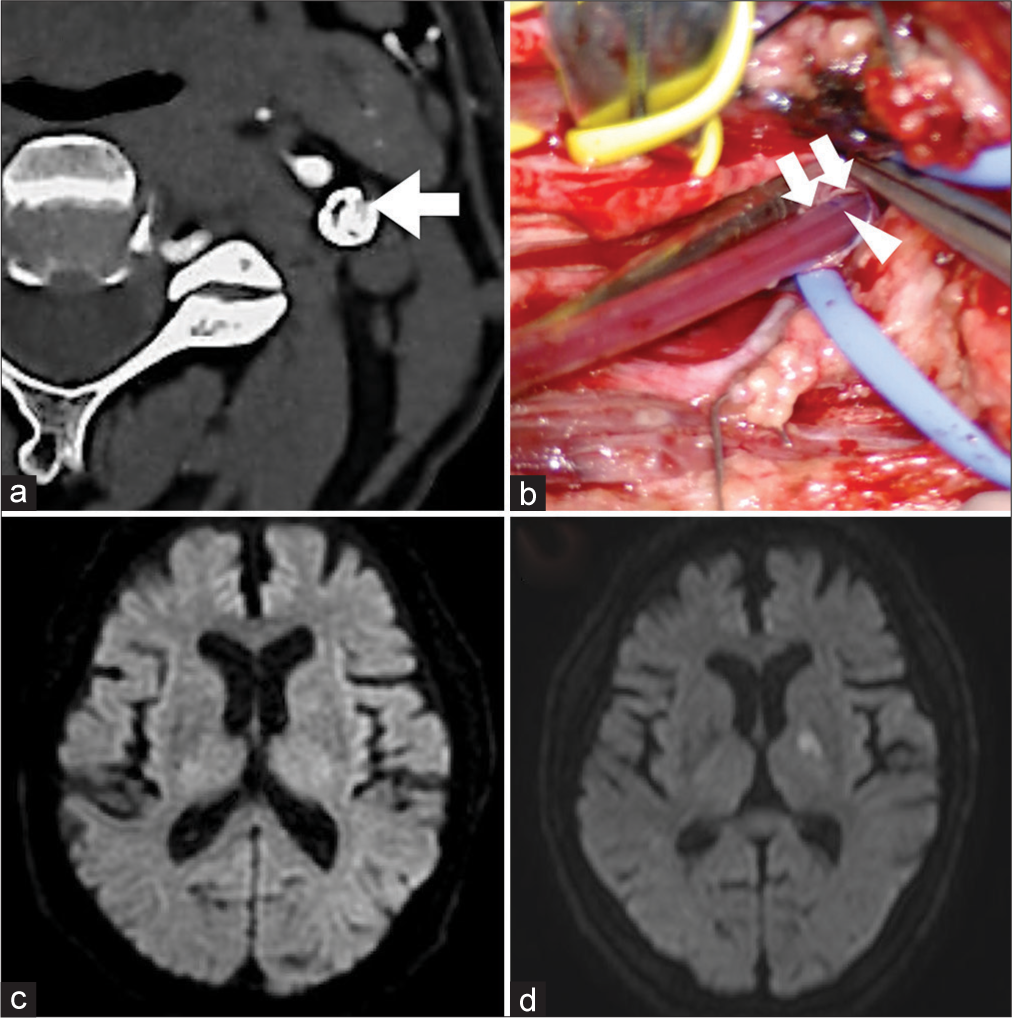
Figure 1:
(a) Computed tomography angiography showed internal carotid artery (ICA) stenosis with marked calcification. The arrow indicates the narrowed inner lumen of ICA. (b) After endarterectomy. Arrow head shows the marker of the internal shunt which is 3 centimeters apart from the end. Double arrows show the edge of the intima. (c) No new cerebral infarction was confirmed by brain MRI on POD 1. (d) On POD 7, the patient developed dysarthria and right-sided hemiplegia. Brain MRI showed acute infarction at the left posterior limb of internal capsule.
We performed CEA under general anesthesia with intraoperative somatosensory evoked potential monitoring, which is a standard practice at our institution. The neck was hyperextended, slightly tilted to the right. As the cerebral cross flow during carotid clamping was suspected to be low, we placed an indwelling arterial shunt (Furui’s Double-Balloon Internal Shunt system, Inter Medical, Aichi, Japan). The shunt was inserted smoothly, the balloon was inflated with 0.4 ml saline and after placement, the patency of the shunt was confirmed. Endarterectomy was completed, and as the distal end of the plaque was smoothly resected, we did not add a tacking suture [
Postoperatively, no neurological deficit was observed. No new cerebral infarction was confirmed by brain MRI on postoperative day (POD) 1 [
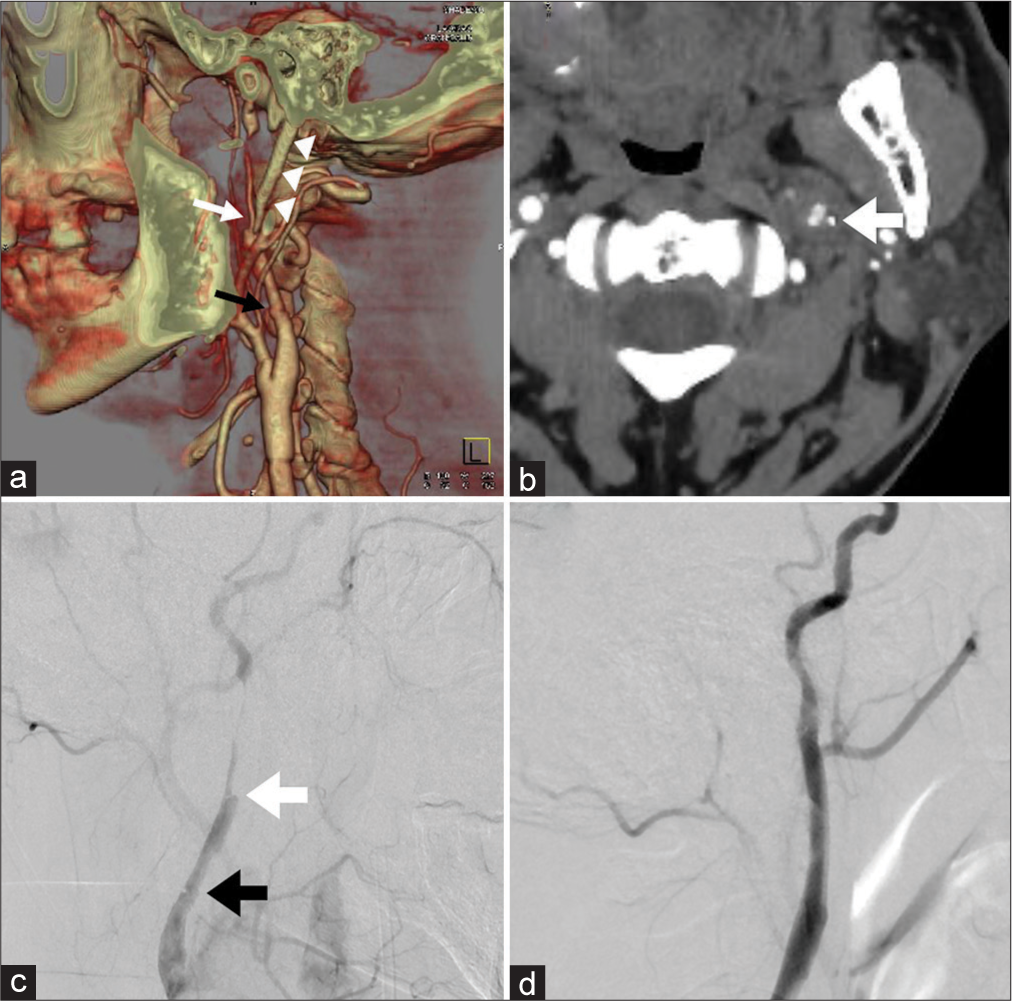
Figure 2:
(a) The post-operative segment of the carotid artery was patent without stenosis on computed tomography angiography, while severe stenosis of the left internal carotid artery (ICA) (white arrow) was observed 2.5 cm distal to the endpoint of carotid endarterectomy (CEA) (black arrow), which suggested distal carotid artery dissection (CAD). The tip of styloid process (arrow heads) located at the beginning of the stenosis. (b) On axial image, the tip of the elongated styloid process (arrow) was adjacent to the ICA. (c) Carotid artery angiography also showed severe stenosis (white arrow) beginning 2.5 cm distal to the endpoint of CEA (black arrow) and confirmed distal CAD, which extended about 3 cm additionally distally. (d) Anterograde blood flow was restored after the two stent placements.
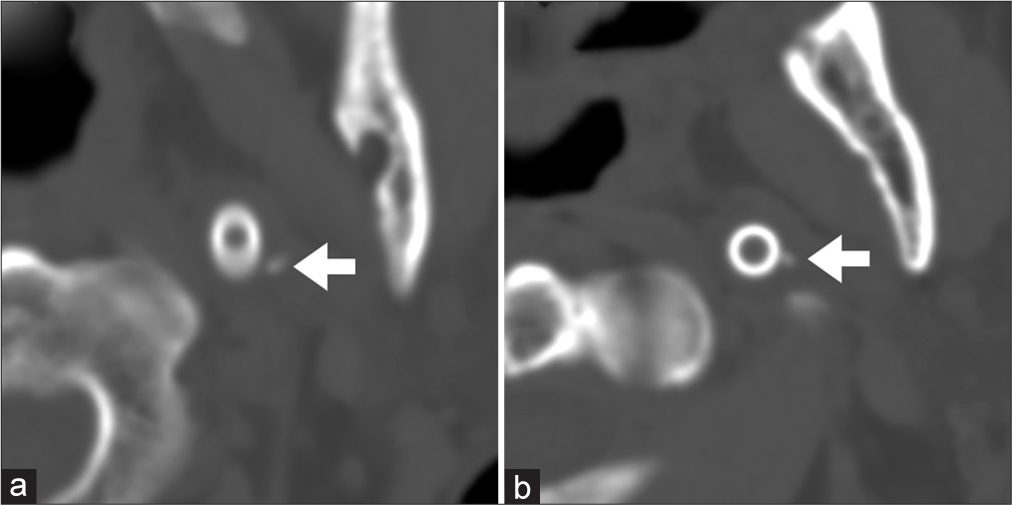
Dysarthria and right-sided hemiplegia improved after the operation and the postoperative course was uneventful. By dynamic assessment with CT for exploration of the pathogenesis, we reproducibly confirmed the tip of the styloid process approaching toward the ICA by moving the head from the neutral neck position to the extended position [
Patient consent was obtained. IRB/Ethics Committee review/ approval is not required.
Figure 3:
(a) Computed tomography (CT) shows that the tip of the styloid process (arrow) apart from the internal carotid artery (ICA) (represented by the cross section of the stent) in neutral neck position. (b) Dynamic CT shows that the tip of the styloid process (arrow) comes close to the ICA by neck extension.
DISCUSSION
CAD is a rare but well-known complication of CEA, which occurs due to intimal flap detachment at the distal end of the endarterectomy.[
While indwelling shunt placement is helpful in performing safe manipulation in low ischemic tolerance cases, few severe surgical complications such as common CAD, traumatic ICA aneurysm, and distal ICA rupture have been reported.[
In a previous case report of vascular Eagle syndrome, Farhat et al. performed a dynamic angiography, which showed focal flow restriction on turning the head to the left, a position that habitually led to a transient ischemic attack. (Farhat) We confirmed the tip of the styloid process reaching toward the ICA by turning the neck from neutral to extended position in postoperative evaluation [
Since the lesion was apart from the distal end of endarterectomy, and extended distal to the Blaisdell’s line, we selected CAS rather than open exploration. There have been reports of CAS for CAD after CEA, in which normal anterograde blood flow was recovered, although the stent deployment is not so easy as it is difficult to identify the correct lumen.[
An elongated styloid process may be a risk factor for surgical complication after CEA using an indwelling shunt, we should assess its length and position preoperatively. If an elongated styloid process is detected, the necessity of shunt placement should be discussed and a hyperextended neck position might be avoided to prevent CAD. As styloidectomy can be performed through the same exposure with slight extension of the standard longitudinal incision parallel to the anterior border of the sternocleidomastoid muscle, it might be considered as an option when performing CEA.
CONCLUSION
A case of distal CAD after CEA due to indwelling shunt and elongated styloid process was observed and analyzed. Since a distal CAD can cause severe, irreversible neurological deficits, preoperative assessment of the styloid process should be routinely performed in CEA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anzuini A, Briguori C, Roubin GS, Pagnotta P, Rosanio S, Airoldi F. Emergency stenting to treat neurological complications occurring after carotid endarterectomy. J Am Coll Cardiol. 2001. 37: 2074-9
2. Bandyk DF, Thiele BL. Safe intraluminal shunting during carotid endarterectomy. Surgery. 1983. 93: 260-3
3. Calhoun TR, Kitten CM. Proximal shunt dissection: A potential problem in carotid endarterectomy. Tex Heart Inst J. 1985. 12: 359-61
4. Eagle WW. Symptomatic elongated styloid process report of two cases of styloid process-carotid artery syndrome with operation. Archiv Otolaryngol. 1949. 49: 490-503
5. Farhat HI, Elhammady MS, Ziayee H, Aziz-Sultan MA, Heros RC. Eagle syndrome as a cause of transient ischemic attacks: Case report. J Neurosurg. 2009. 110: 90-3
6. Halsey JH. Risks and benefits of shunting in carotid endarterectomy. The International Transcranial Doppler Collaborators. Stroke. 2018. 23: 1583-7
7. Hooker JD, Joyner DA, Farley EP, Khan M. Carotid stent fracture from stylocarotid syndrome. J Radiol Case Rep. 2016. 10: 1-8
8. Illuminati G, Caliò FG, Pizzardi G, Vietri F. Internal carotid artery rupture caused by carotid shunt insertion. Int J Surg Case Rep. 2015. 14: 89-91
9. Katsuno M, Tanikawa R, Hashimoto M, Matsuno A. Distal internal carotid artery dissection due to the carotid shunt during carotid endarterectomy. Br J Neurosurg. 2015. 29: 862-4
10. Loftus CM, Dyste GN, Reinarz SJ, Hingtgen WL. Distal cervical carotid dissection after carotid endarterectomy: A complication of indwelling shunt?. Neurosurgery. 1986. 19: 441-5
11. Ogura T, Mineharu Y, Todo K, Kohara N, Sakai N. Carotid artery dissection caused by an elongated styloid process: Three case reports and review of the literature. NMC Case Rep J. 2015. 2: 21-5
12. Riles TS, Imparato AM, Jacobowitz GR, Lamparello PJ, Giangola G, Adelman MA. The cause of perioperative stroke after carotid endarterectomy. J Vasc Surg. 1994. 19: 206-16
13. Sundt TM, Sharbrough FW, Marsh WR, Ebersold MJ, Piepgras DG, Messick JM. The risk-benefit ratio of intraoperative shunting during carotid endarterectomy: Relevancy to operative and postoperative results and complications. Ann Surg. 1986. 203: 196-204
14. Sveinsson O, Kostulas N, Herrman L. Internal carotid dissection caused by an elongated styloid process (Eagle syndrome). BMJ Case Rep. 2013. 2013: bcr2013009878
15. Takahashi T, Ikeda G, Igarashi H, Konishi T, Araki K, Hara K. Emergent carotid artery stenting for cervical internal carotid artery injury during carotid endarterectomy: A case report. Surg Neurol Int. 2021. 12: 109
16. Tamaki T, Yoji N, Saito N. Distal cervical carotid artery dissection after carotid endarterectomy: A complication of indwelling shunt. Int J Vasc Med. 2010. 2010: 816937
17. Troisi N, Dorigo W, Pulli R, Pratesi C. A case of traumatic internal carotid artery aneurysm secondary to carotid shunting. J Vasc Surg. 2010. 51: 225-7