- Department of General Surgery, Central Michigan University College of Medicine, Michigan, United States.
- Department of Neurological Surgery, University Hospitals Cleveland Medical Center, Cleveland, Ohio, United States.
- Department of Neuroscience, Ascension St. Mary’s Hospital, Saginaw, Michigan, United States.
Correspondence Address:
Joseph G. Adel, MD, FAANS, Department of Neuroscience, Ascension St. Mary’s Hospital, Saginaw, Michigan, United States.
DOI:10.25259/SNI_740_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Danielle Hebert1, Theresa A. Elder2, Joseph G. Adel3. Emergent carotid endarterectomy and mechanical thrombectomy in tandem occlusion. 11-Nov-2022;13:521
How to cite this URL: Danielle Hebert1, Theresa A. Elder2, Joseph G. Adel3. Emergent carotid endarterectomy and mechanical thrombectomy in tandem occlusion. 11-Nov-2022;13:521. Available from: https://surgicalneurologyint.com/surgicalint-articles/11995/
Abstract
Background: Acute tandem occlusions, or occlusions of the extracranial portion of the internal carotid artery (ICA) with concurrent thromboembolism of the intracranial ICA or middle cerebral artery, poses a major clinical challenge, with patients suffering worse outcomes compared to those with single occlusions. Management of these lesions generally includes a combination of mechanical thrombectomy (MT) of the intracranial occlusion and stenting of the extracranial carotid lesion. In this manuscript, we describe a successful surgical method for achieving revascularization of tandem occlusions in the rare circumstance that the proximal lesion cannot be crossed endovascularly to gain intracranial access.
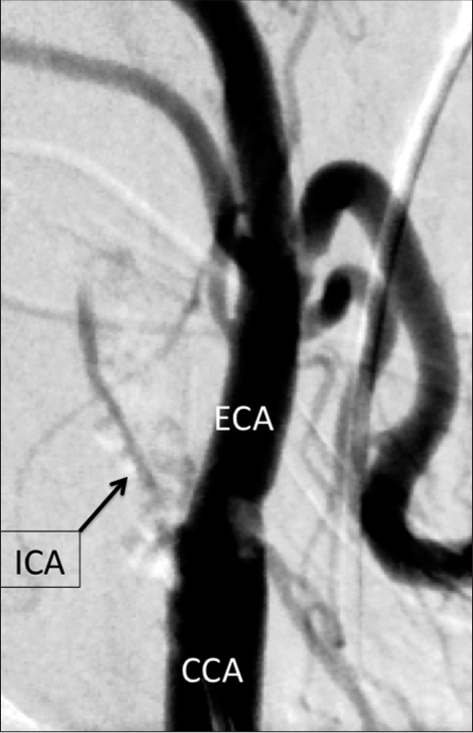
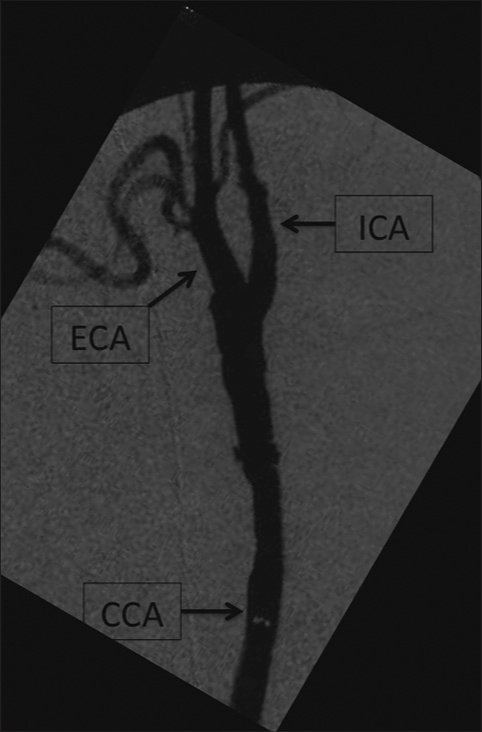
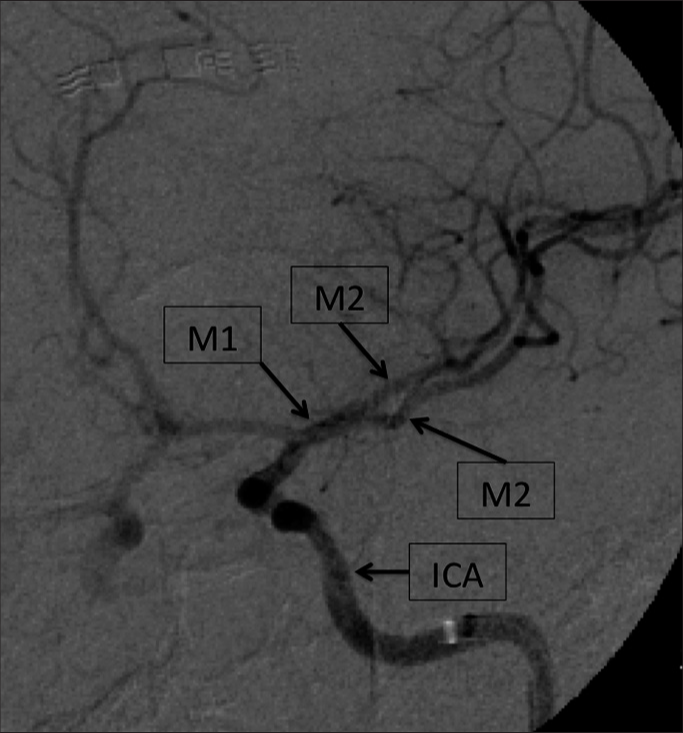
Methods: Despite using our institution’s standard protocol for achieving revascularization of such lesions, the extracranial occlusion could not be crossed endovascularly, and the case was converted to an emergent carotid endarterectomy (CEA) in the operating room. Once the endarterectomy was complete, intraoperative MT was performed before cervical incision closure to revascularization.
Results: The patient recovered well postoperatively and was discharged with NIHSS of 2 due to minor facial palsy and minor dysarthria. Thirty-day follow-up revealed resolution of the prior neurologic deficits and an mRS of 1.
Conclusion: Emergent CEA should be considered in the rare circumstance of being unable to cross the cervical occlusion during management of acute ischemic stroke with tandem occlusion.
Keywords: Carotid occlusion, Endarterectomy, Endovascular, Ischemic stroke, Mechanical thrombectomy, Tandem occlusion
INTRODUCTION
Management of acute tandem occlusions, or occlusions of the extracranial portion of the internal carotid artery (ICA) with concurrent thromboembolism of the intracranial ICA or middle cerebral artery (MCA), poses a major clinical challenge. Approximately 10–15% of large vessel occlusions resulting in acute ischemic stroke (AIS) are related to tandem occlusions; however, despite their prevalence, an optimal management strategy has not been reached.[
Current endovascular therapeutic strategies include recanalization of the intracranial occlusion through mechanical thrombectomy (MT) followed by stenting of the extracranial ICA (head-first), and the reverse, extracranial stenting followed by intracranial MT (neck-first). Cirillo et al. found that endovascular ICA stenting used in management of tandem occlusions led to improved revascularization and had improved long-term morbidity and mortality when compared to non-stenting techniques.[
At our institution, a comprehensive stroke center, we have adopted the head-first paradigm, as described previously.[
CASE PRESENTATION
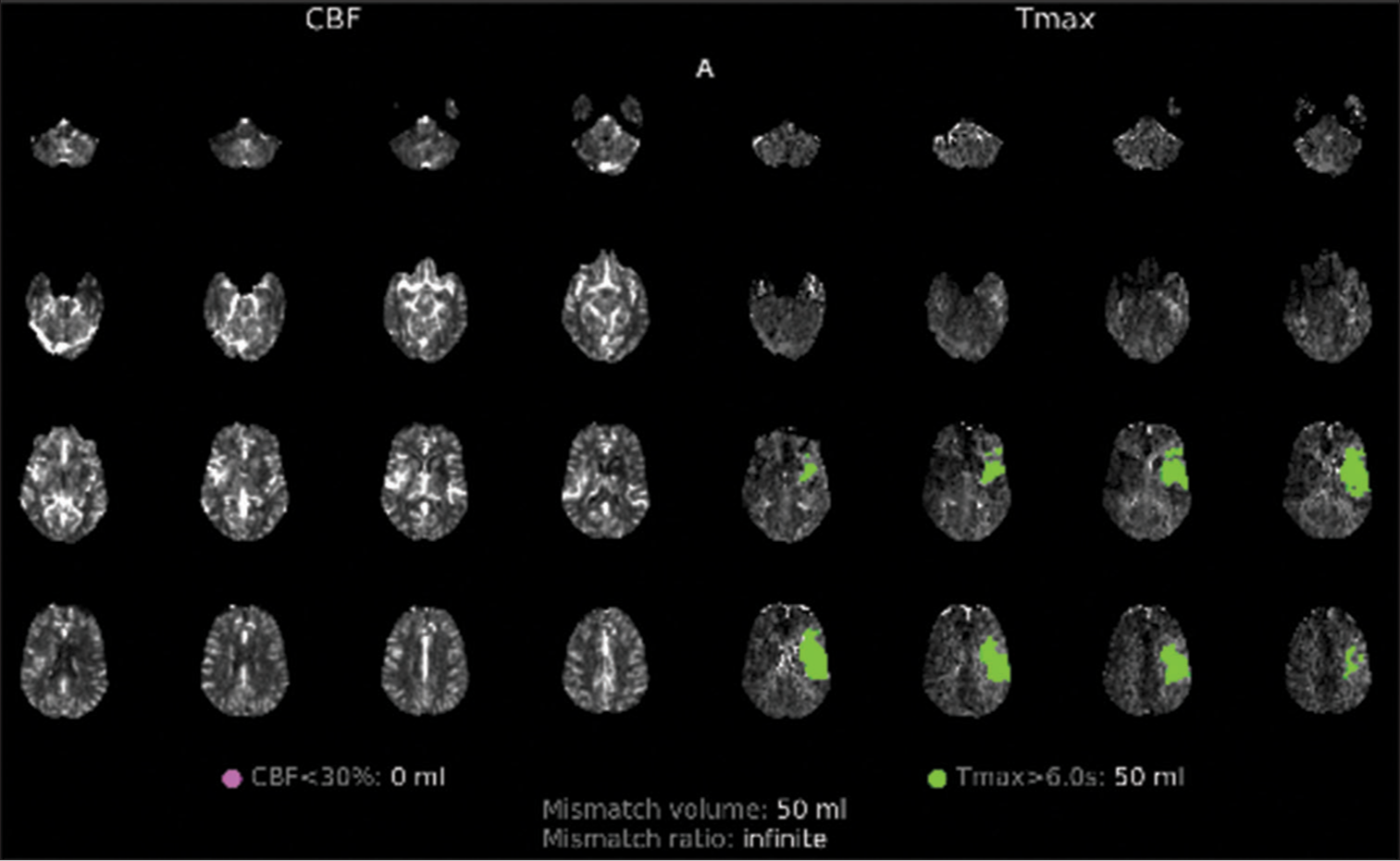
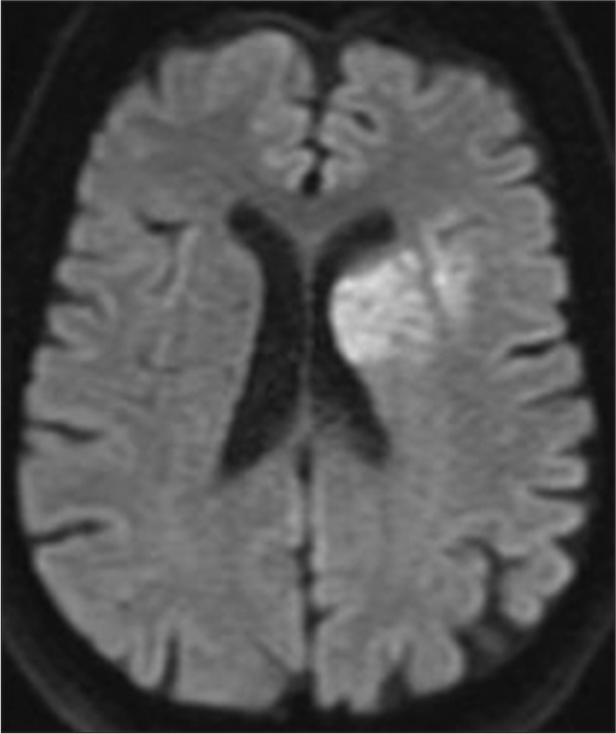
The patient is a 78-year-old who awakened with aphasia and right hemiparesis. When symptoms persisted, he presented to an outside hospital and was not a candidate for tPA given unknown onset of symptoms. Of note is the patient had suffered sudden loss of vision in the left eye 2 weeks before presentation, was started on aspirin, evaluated by ophthalmology as an outpatient, and was thought to be an ischemic etiology, so a carotid ultrasound was ordered but had not been completed by the time of his presentation. Computed tomography (CT) angiography/CT perfusion was completed (Time 00:00) revealing cervical carotid occlusion and tandem left MCA-M2 occlusion with no core infarct and 50 ml of ischemic penumbra [
DISCUSSION
In our case, proceeding with an emergent CEA was the reason MT was feasible. Although not classically performed in the setting of tandem occlusions, CEA served as a crucial step in the management of this patient. As stated previously, thrombolysis has poor efficacy in patients with tandem occlusions and the endovascular technique is superior.[
To consider introducing emergent CEA as a management option, the treating facility has to be equipped for rapid conversion to operative intervention. For patients undergoing urgent CEAs, the rate of perioperative complication is higher than those who undergo elective CEA, and this is especially true regarding neurologic and cardiac complications.[
Despite the good neurologic outcome, the time to achieve reperfusion was suboptimal and leaves room for improvement. Had emergent CEA been a prior consideration, we would have saved significant time to achieve revascularization. Less time would have been spent on the failed attempts at coursing the occlusion, the OR would have been notified sooner, and a few minutes could have been saved in every step to achieve reperfusion had we have this approach planned for and protocoled previously. Similar to direct carotid puncture for difficult access, since it became a consideration, our preparedness and ability to safely utilize it became more timely and efficient.
CONCLUSION
This case highlights how the emergent CEA made reperfusion of the tandem occlusion possible and did not result in adverse events. We believe, this option is important to consider in the rare circumstance of being unable to cross a cervical occlusion in the setting of tandem occlusion during management of AIS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cirillo L, Romano DG, Vornetti G, Frauenfelder G, Tamburrano C, Taglialatela F. Acute ischemic stroke with cervical internal carotid artery steno-occlusive lesion: Multicenter analysis of endovascular approaches. BMC Neurol. 2021. 21: 362
2. Elder TA, Verhey LH, Schultz H, Smith ES, Adel JG. Cervical carotid occlusion in acute ischemic stroke: Should we give tPA?. Surg Neurol Int. 2022. 13: 177
3. Haussen DC, Turjman F, Piotin M, Labreuche J, SteglichArnholm H, Holtmannspotter M. Head or neck first? Speed and rates of reperfusion in thrombectomy for tandem large vessel occlusion strokes. Interv Neurol. 2020. 8: 92-100
4. Howell SJ. Carotid endarterectomy. Br J Anaesth. 2007. 99: 119-31
5. Kappelhof M, Marquering HA, Berkhemer OA, Majoie CB. Intra-arterial treatment of patients with acute ischemic stroke and internal carotid artery occlusion: A literature review. J Neurointerv Surg. 2015. 7: 8-15
6. Karkos CD, Hernandez-Lahoz I, Naylor AR. Urgent carotid surgery in patients with crescendo transient ischaemic attacks and stroke-in-evolution: A systematic review. Eur J Vasc Endovasc Surg. 2009. 37: 279-88
7. Kim YS, Garami Z, Mikulik R, Molina CA, Alexandrov AV, CLOTBUST Collaborators. Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion. Stroke. 2005. 36: 869-71
8. Lockau H, Liebig T, Henning T, Neuschmelting V, Stetefeld H, Kabbasch C. Mechanical thrombectomy in tandem occlusion: Procedural considerations and clinical results. Neuroradiology. 2015. 57: 589-98
9. Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J. Tandem internal carotid artery/ middle cerebral artery occlusion: An independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006. 37: 2301-5
10. Zhu F, Hossu G, Soudant M, Richard S, Achit H, Beguinet M. Effect of emergent carotid stenting during endovascular therapy for acute anterior circulation stroke patients with tandem occlusion: A multicenter, randomized, clinical trial (TITAN) protocol. Int J Stroke. 2021. 16: 342-8