- Department of Neurosurgery, New York Presbyterian Hospital, New York, United States.
DOI:10.25259/SNI_619_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Carnevale JA, Goldberg JL, Holland CE, Souweidane MM. Endoscopic removal of intraventricular neurocystercercosis. Surg Neurol Int 03-Feb-2021;12:38
How to cite this URL: Carnevale JA, Goldberg JL, Holland CE, Souweidane MM. Endoscopic removal of intraventricular neurocystercercosis. Surg Neurol Int 03-Feb-2021;12:38. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10563
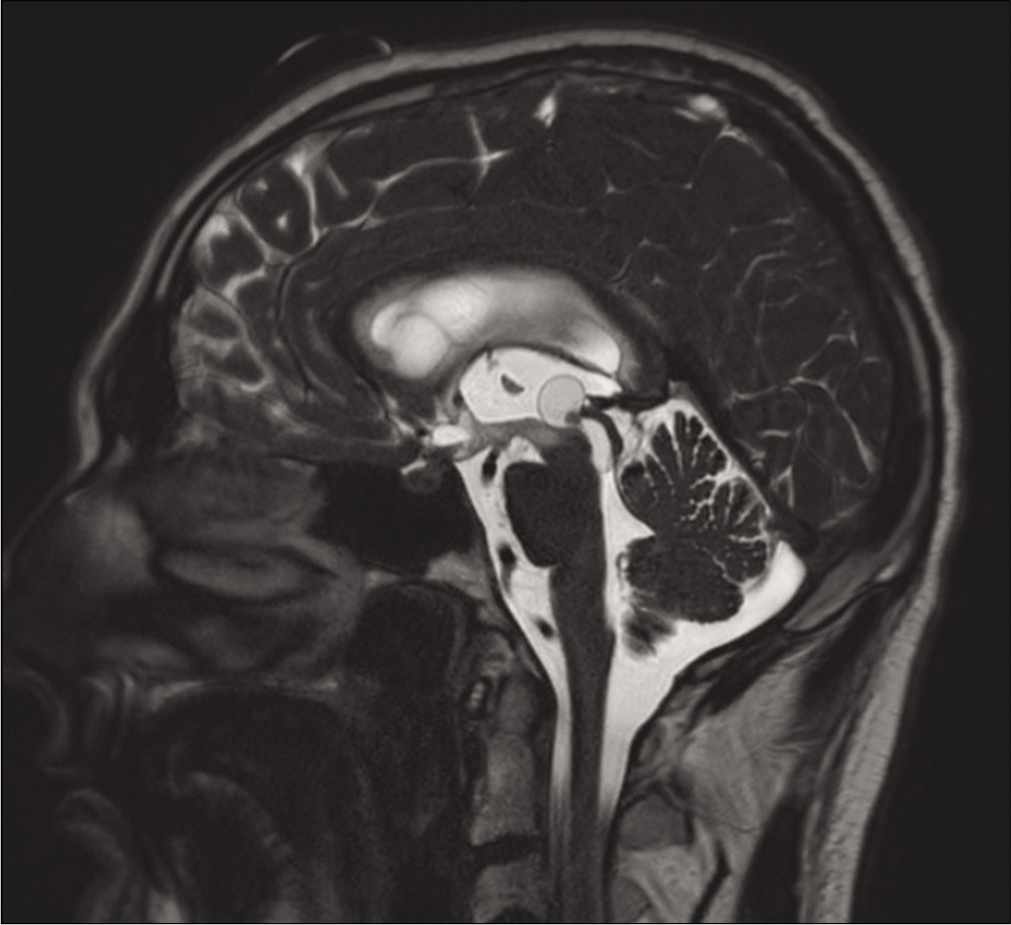
A 29-year-old male with extensive travel history presented with altered mental status and headaches. Head computed tomography imaging revealed obstructive hydrocephalus and an external ventricular drain was placed with neurologic improvement. Serum and cerebrospinal fluid (CSF) testing were nondiagnostic, including negative cysticerci antibodies. Magnetic resonance imaging revealed a cystic lesion centered in the posterior third ventricle obstructing the cerebral aqueduct [
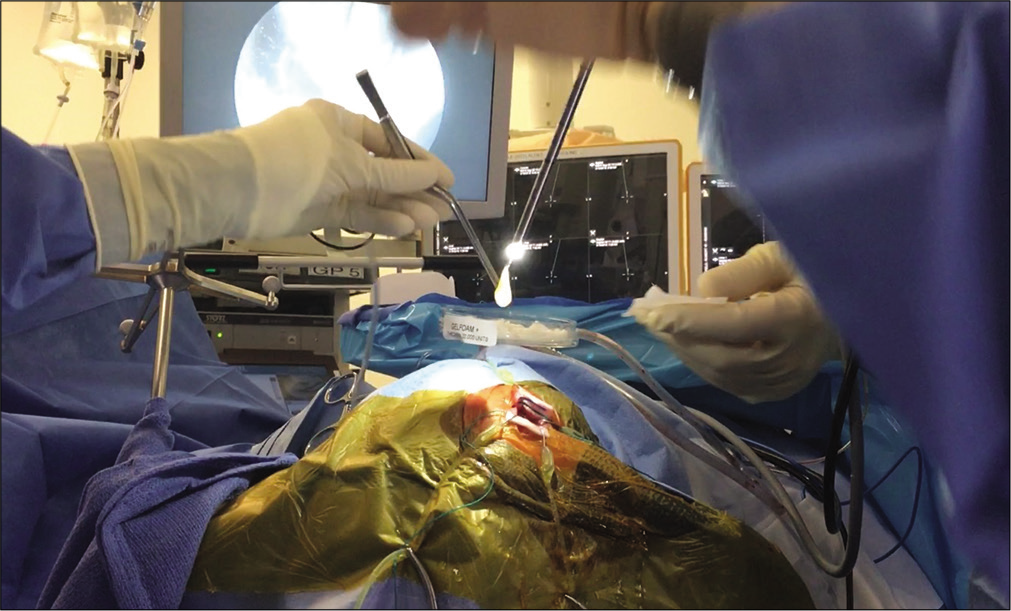
Video 1
Figure 1:
T2-weighted magnetic resonance imaging of the brain with a cystic lesion centered in the posterior floor of the third ventricle along the opening of the cerebral aqueduct, measuring approximately 1.3 × 1.0 × 1.7 cm. The mass demonstrated trace peripheral enhancement and a punctate focus of internal susceptibility, which may reflect internal calcification. The scan further characterized the known ventriculomegaly with periventricular T2 hyperintensities consistent with transependymal cerebrospinal fluid flow, further supporting the diagnosis of obstructive hydrocephalus.
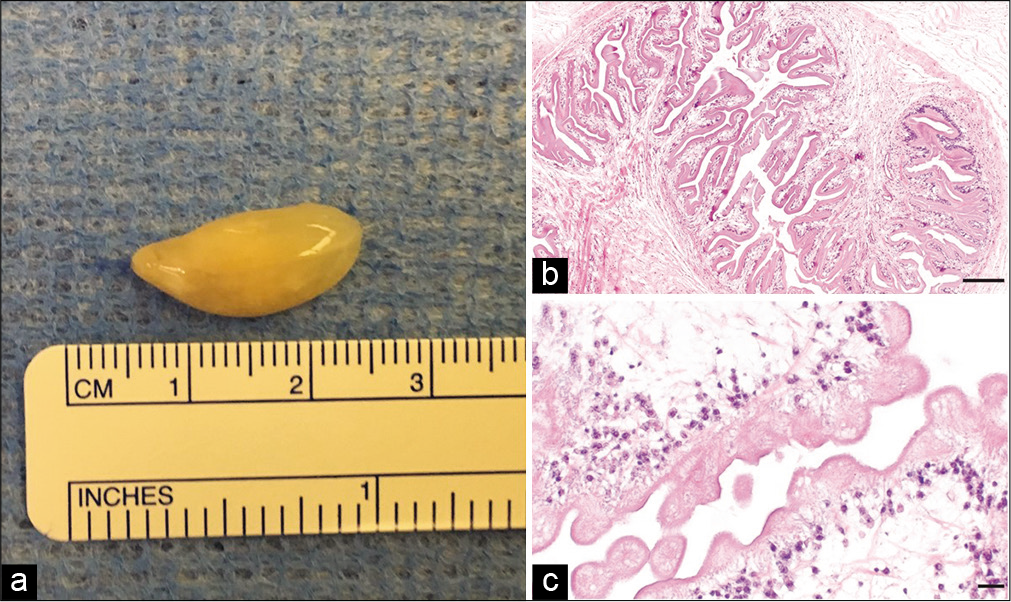
Figure 3:
(a) Grossly, the specimen is a smooth surface, yellowed cyst with a central portion of more firm nodularity. Microscopically at low (b – scale bar 200 um) and high (c – scale bar 20 um) power on H&E staining, the specimen exhibited the structure of a tapeworm with a morphology consistent with Taenia Solium, the parasitic etiology of neurocystercercosis.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
www.surgicalneurologyint.com
References
1. Cuetter AC, Garcia-Bobadilla J, Guerra LG, Martinez FM, Kaim B. Neurocysticercosis: Focus on intraventricular disease. Clin Infect Dis. 1997. 24: 157-64
2. Gripper LB, Welburn SC. Neurocysticercosis infection and disease-a review. Acta Trop. 2017. 166: 218-24
3. Jensen TO, Post JJ. Intraventricular neurocysticercosis: Presentation, diagnosis and management. Asian Pac J Trop Med. 2016. 9: 815-8
4. Zhenye L, Chuzhong L, Xuyi Z, Songbai G, Peng Z, Jiwei B. Ventriculoscopic approach for intraventricular neurocysticercosis: A single neurosurgical center’s experience. World Neurosurg. 2017. 107: 853-9