- Departments of Neurosurgery, Kaiser Permanente Fontana Medical Center, Fontana, United States.
- Departments of Neurosurgery, Riverside University Health System, Riverside, California, United States.
Correspondence Address:
Samir Kashyap
Departments of Neurosurgery, Kaiser Permanente Fontana Medical Center, Fontana, United States.
DOI:10.25259/SNI-233-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Samir Kashyap, Bhagat Cheema, Vaninder Chhabra. Endoscopic resection of the third ventricular epidermoid cysts: A case review and review of literature. 07-Jun-2019;10:98
How to cite this URL: Samir Kashyap, Bhagat Cheema, Vaninder Chhabra. Endoscopic resection of the third ventricular epidermoid cysts: A case review and review of literature. 07-Jun-2019;10:98. Available from: http://surgicalneurologyint.com/surgicalint-articles/9349/
Abstract
Background:Epidermoid cysts are benign, congenital lesions that originate from ectodermal cells, they are most commonly found in the cerebellopontine angle, but rarely in the ventricular system. There is limited literature regarding the different microsurgical techniques utilized to approach these lesions.
Methods:A 63-year-old female with a recurrent third ventricular epidermoid cyst underwent gross total resection utilizing an endoscopic technique. We also reviewed the various endoscopic/microsurgical approaches and outcomes reported in literature.
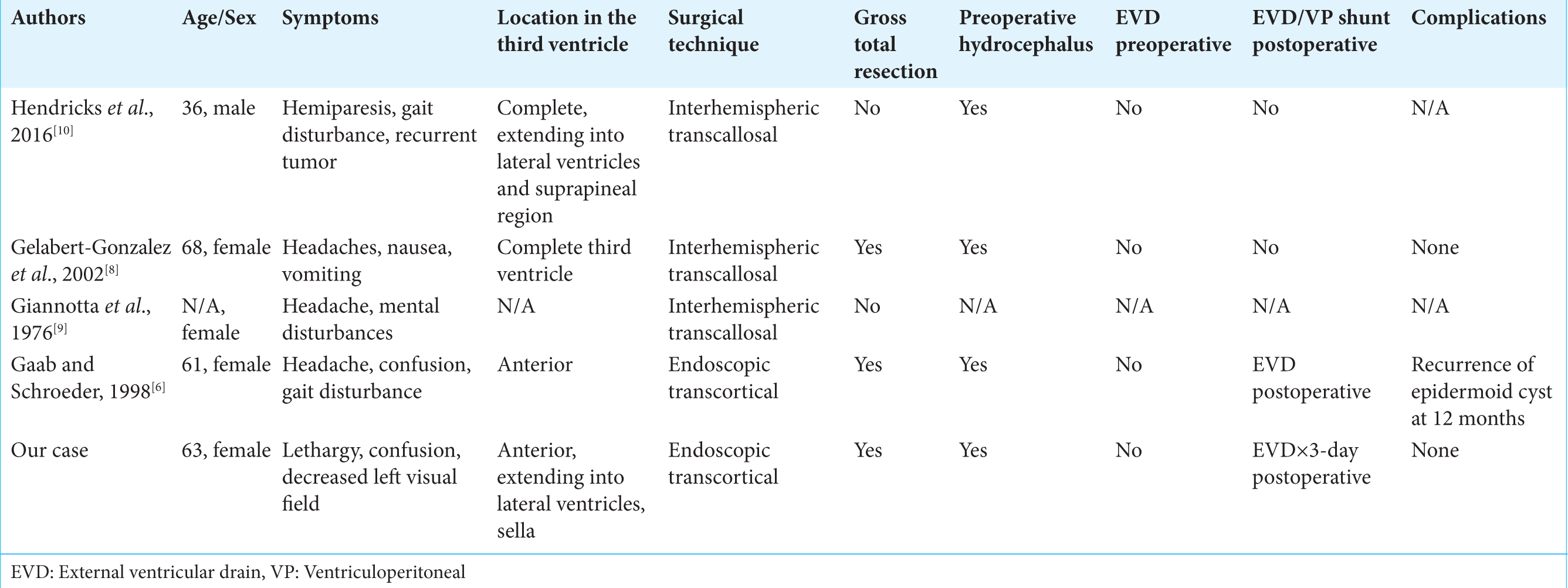
Results:We identified 15 cases, including our own. Nine of these were managed using microsurgical techniques, while six cases (including ours) were treated endoscopically; gross total resection was achieved in 10/15 cases (67%). Most commonly, surgeons utilized the interhemispheric transcallosal approach (five cases). Tumor recurrence was seen in two cases. Complications attributed to these resections included: disorders of the hypothalamic-pituitary axis (3) – diabetes insipidus, galactorrhea, and hypopituitarism; tumor recurrence (2); aseptic meningitis (1); and a transient Korsakoff syndrome (1).
Conclusion:Epidermoid cysts of the third ventricle are exceedingly rare, and surgical resection is generally well tolerated. Microsurgical transcortical, transcallosal, and endoscopic approaches each have advantages and disadvantages, and are associated with unique procedure-specific complications. Continuing technological improvement would favor endoscopic approaches for resection of tumors of the third ventricle in the future.
Keywords: Epidermoid cyst, Neuroendoscopy, Third ventricle
INTRODUCTION
Epidermoid cysts are benign, congenital lesions that originate from ectodermal cells.[
Clinical presentation
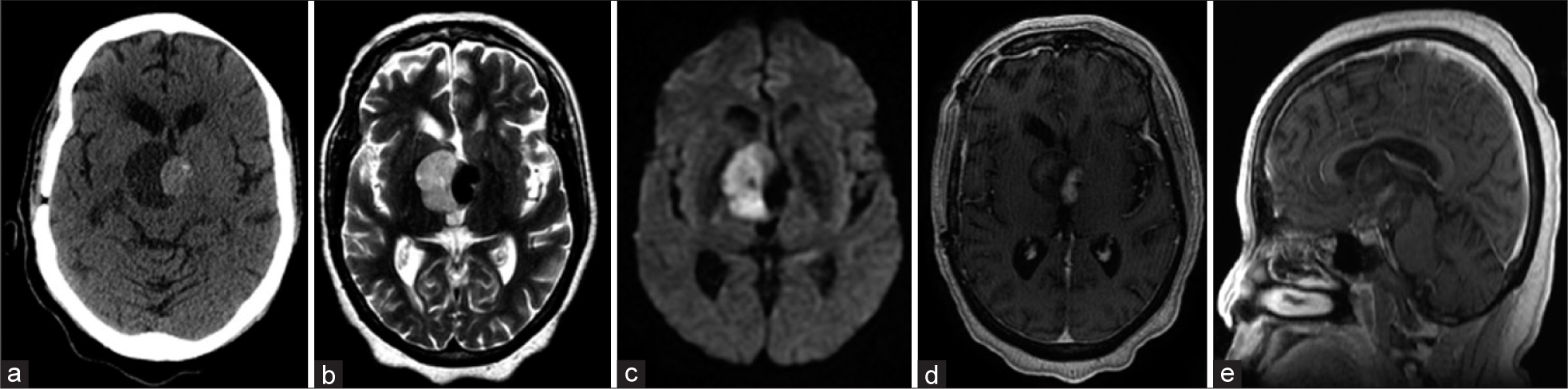
A 63-year-old female presented with several days of confusion/altered level of consciousness. She had a Glasgow Coma Score of 14, was lethargic, and demonstrated a left homonymous hemianopsia. In 2015, she had undergone a craniotomy for subtotal resection of an epidermoid cyst. Now, the computed tomography (CT) scan revealed a large mixed-density suprasellar mass effacing the third ventricle, with a notable increase in the size of the cyst [
Figure 1
Preoperative – *(a) Noncontrast computed tomography head demonstrating epidermoid cysts of the third ventricle. (b) Axial T2 sequence showing the cystic and solid components of the tumor. (c) Diffusion-weighted imaging showing the characteristic diffusion restriction associated with epidermoid cysts. (d) T1 postcontrast axial sequence showing enhancement of the solid component of the cyst with minimal enhancement within the cystic component. (e) T1 postcontrast sagittal sequence showing occupation of the third ventricle by the tumor.
Surgical management
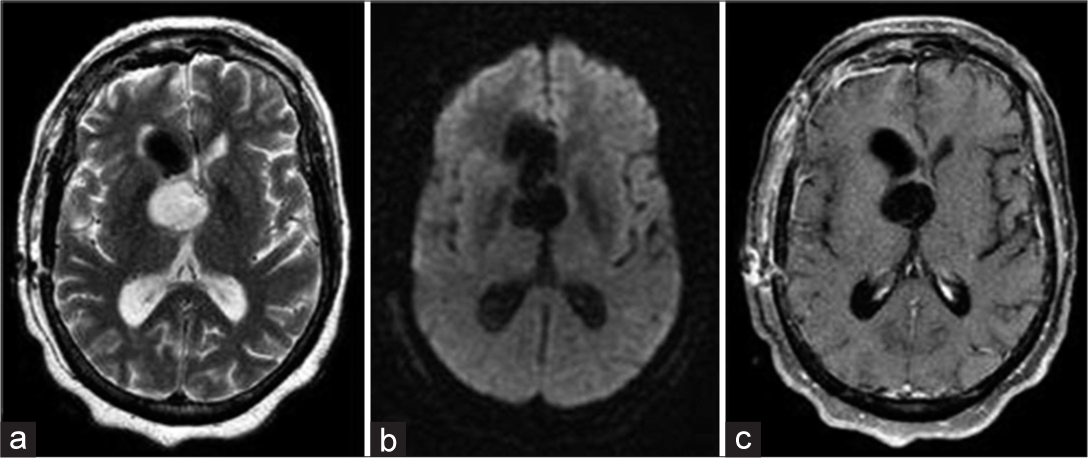
Through a small, elliptical right frontal craniotomy and corticectomy, the third ventricle was entered using an 11.5 mm Thoracoport with the assistance of stereotactic navigation. An endoscope was placed down the port and through the foramen of Monroe; tumor was identified as adherent to the floor of the third ventricle. An Angiocath, attached to a syringe, was utilized to drain the cyst. Pulsatile bacitracin/normal saline irrigation was then utilized to flush the ventricular system, and the cyst contents were gently suctioned and removed. Liliequist’s membrane was identified, and additional tumor was noted to be deep to the membrane. When it was opened, keratin fragments were mobilized with pulsatile irrigation. Endoscopic biopsy instruments then afforded removal of more adherent tissue. The remaining fragments that had settled in the occipital horn were also mobilized and removed. A ventricular catheter was then left in place as the Thoracoport was removed. Postoperatively, the patient exhibited a left gaze preference (without a residual field cut) that persisted. Imaging consistant with gross total resection [
DISCUSSION
Review of literature
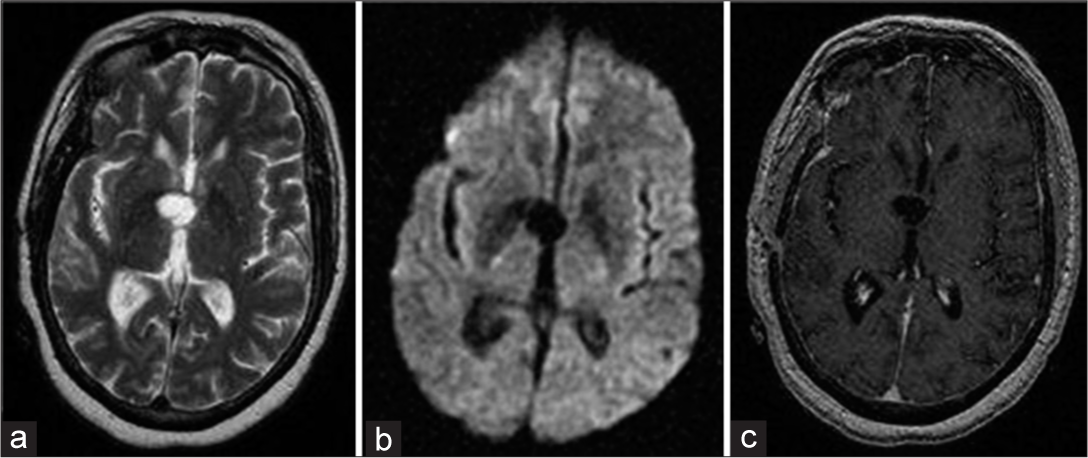
A review of literature, including our case, yielded 15 cases undergoing resection of the third ventricular epidermoid cysts [
Anatomy and pathophysiology of epidermoid tumors
Epidermoid cysts are slow-growing, benign lesions that comprise 0.2%–1.8% of all intracranial tumors.[
Clinical, radiographic diagnosis, and treatment of the third ventricular epidermoid tumors
These lesions are typically incidental findings on CT, but magnetic resonance imaging is often the optimal confirmatory test.[
Surgical approaches to the third ventricle
There are three essential approaches to the third ventricle: transcortical, transcallosal, and endoscopic. The transcortical approach traditionally utilizes entry to the ventricle through a right frontal trajectory. There are, however, three variations of this approach utilizing a frontal, parietal, or middle temporal gyrus trajectory.[
CONCLUSION
There are various microsurgical and endoscopic techniques for approaching epidermoid cysts/tumors in the third ventricle. The aim is to limit disruption of normal tissue and injury to the limbic system, while still providing adequate surgical exposure. In our case and reviewing the literature, we noted gross total resection of these lesions could be achieved in 83% of endoscopic cases (5/6), compared to 3/5 utilizing the interhemispheric approach. Further, advances in endoscopy may eventually establish this technique as the new standard of care for the surgical management of the third ventricular epidermoid cysts.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bikmaz K, Dinc C, Cakabay M, Iplikcioglu AC. Epidermoid cyst of the cavum septum pellucidum. Acta Neurochir (Wien). 2007. 149: 1271-2
2. Brandão FR, Black P, Filho H. Approaches to the third ventricle. Braz Arch Neurosurg. 2012. 31: 3-9
3. Caldarelli M, Massimi L, Kondageski C, Di Rocco C. Intracranial midline dermoid and epidermoid cysts in children. J Neurosurg. 2004. 100: 473-80
4. Chowdhury FH, Haque MR, Sarker MH. Intracranial epidermoid tumor; Microneurosurgical management: An experience of 23 cases. Asian J Neurosurg. 2013. 8: 21-8
5. D’Angelo VA, Galarza M, Catapano D, Monte V, Bisceglia M, Carosi I. Lateral ventricle tumors: Surgical strategies according to tumor origin and development-a series of 72 cases. Oper Neurosurg. 2005. 56: 36-45
6. Gaab MR, Schroeder HW. Neuroendoscopic approach to intraventricular lesions. J Neurosurg. 1998. 88: 496-505
7. Gaab MR, Schroeder HW. Neuroendoscopic approach to intraventricular lesions. Neurosurg Focus. 1999. 6: e5-
8. Gelabert-González M, García-Allut A, González-García J, Martínez-Rumbo R. Epidermoid tumor of the third ventricle. Neurocirugía. 2002. 13: 389-92
9. Giannotta SL, Pauli F, Farhat SM. Epidermoid cyst of the third ventricle. Surg Neurol. 1976. 5: 164-6
10. Hendricks BK, Cohen-Gadol AA. Resection of large recurrent third ventricular epidermoid tumors through the posterior interhemispheric transcallosal approach. Neurosurg Focus. 2016. 40:
11. Iaconetta G, Samii M. Third ventricle epidermoid cyst. Br J Neurosurg. 2001. 15: 529-30
12. Kontoangelos K, Economou M, Maltezou M, Kandaraki A, Papadimitriou GN. Depressive symptomatology and pineal epidermoid cyst: A case report. Acta Neuropsychiatr. 2013. 25: 240-2
13. Koumtchev YN, Kalnev YN, Gozmanov YN, Zaprianov YN. Recurrence of epidermoid cyst in the third ventricle. Case report. Folia Med (Plovdiv). 2002. 44: 97-9
14. Kumar A, Singla R, Sharma BS. Anterior third ventricular epidermoid presenting with diabetes insipidus. Neurol India. 2014. 62: 86-8
15. Man R. A rare case of third ventricular epidermoid cyst as seen by newer MRI sequences. Int Neuropsychiatr Dis J. 2014. 2: 68-77
16. Meng L, Yuguang L, Shugan Z, Xingang L, Chengyuan W. Intraventricular epidermoids. J Clin Neurosci. 2006. 13: 428-30
17. Nagasawa D, Yew A, Safaee M, Fong B, Gopen Q, Parsa AT. Clinical characteristics and diagnostic imaging of epidermoid tumors. J Clin Neurosci. 2011. 18: 1158-62
18. Osborn AG, Preece MT. Intracranial cysts: Radiologic-pathologic correlation and imaging approach. Radiology. 2006. 239: 650-64
19. Paz DA, da Costa MD, Rodrigues TP, Riechelmann GS, Suriano ÍC, Zymberg ST. Endoscopic treatment of a third ventricular epidermoid cyst. World Neurosurg. 2017. 99: 813.e7-11
20. Perneczky A, Kindel S, Kanno T, Tschabitscher M, Reisch R.editorsKeyhole Approaches in Neurosurgery: Concept and Surgical Technique. Vol. 1. New York: Springer Science and Business Media; p.
21. Powell MP, Torrens MJ, Thomson JL, Horgan JG. Isodense colloid cysts of the third ventricle: A diagnostic and therapeutic problem resolved by ventriculoscopy. Neurosurgery. 1983. 13: 234-237
22. Reddy P, Jiacheng S, Xunning H, Ma Z. Intracranial epidermoid cyst: Characteristics, appearance, diagnosis, treatment and prognosis. Sci Lett. 2015. 3: 102-10
23. Riviérez M, Ridarch A, Landau-Ossondo M, Randrianbololona J. Epidermoid cyst of the third ventricle. Report of a case. Neurochirurgie. 1998. 44: 283-6
24. Santosh IP, Rajshekhar V. Galactorrhea as the sole presenting symptom of a posterior third ventricular epidermoid cyst. Surg Neurol. 2001. 55: 46-9
25. Schroeder HW, Oertel J, Gaab MR. Endoscope-assisted microsurgical resection of epidermoid tumors of the cerebellopontine angle. J Neurosurg. 2004. 101: 227-32
26. Shimizu Y, Aihara H, Fukawa O, Ishii M. Epidermoid of the third ventricle--report of a case. No Shinkei Geka. 1985. 13: 71-6
27. Smith KA, Chamoun R. Endoscopic resection of an intraventricular epidermoid cyst of the third ventricle. Neurosurg Q. 2014. 24: 229-31
28. Yaşargil MG, Abernathey CD, Sarioglu AC. Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989. 24: 561-7