- Department of Neurosurgery, Faculty of Medicine, Cairo University, Cairo, Egypt.
DOI:10.25259/SNI_800_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed Elmallawany, Ahmed Ashry, Mohamed F. Alsawy. Endoscopic treatment of brain abscess. 28-Jan-2021;12:36
How to cite this URL: Mohamed Elmallawany, Ahmed Ashry, Mohamed F. Alsawy. Endoscopic treatment of brain abscess. 28-Jan-2021;12:36. Available from: https://surgicalneurologyint.com/surgicalint-articles/10547/
Abstract
Background: Treatment of brain abscess is still a subject of controversy. The main treatment is surgical, although medical therapy alone can be used for selected cases. The treatment of choice is aspiration, which may be performed with the aid of an endoscope or by freehand technique, with or without stereotactic or intraoperative ultrasound guidance. Excision is valuable in some cases. We are reporting our results of endoscopic approach in 12 patients.
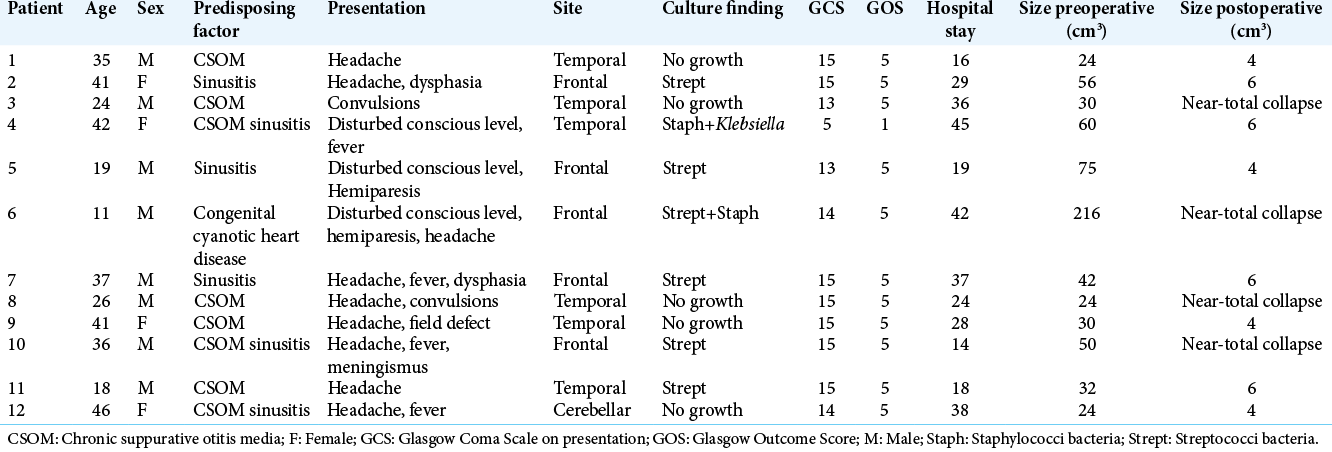
Methods: This study included 12 patients of brain abscesses treated between January 2015 and January 2018. All the cases except those with small abscesses (
Results: There were 11 patients with a history of chronic otitis media and one patient who suffered from congenital cyanotic heart disease. Glasgow Coma Score (GCS) was 5 in one patient, 13 in two cases, and 14–15 in 9 cases. There were one cerebellar, six temporal, and five frontal abscesses. All the patients recovered completely except one who died (GCS 5). There was no procedure-related complication. Hospital stay ranged from 14 to 45 days with an average of 28 days. The endoscopy aided visualization of multiloculations and septation in eight patients which allowed the opening of the septations and complete evacuation.
Conclusion: Endoscopic aspiration is safe, easy, and represents an effective way of treatment of brain abscess through proper visualization. It can be used for ensuring the complete aspiration of contents, control of any bleeding point, and also for multiloculated abscess to identify and open the septations which may not be possible in stereotactic or any other guided aspirations.
Keywords: Abscess, Endoscope, Loculation, Pus
INTRODUCTION
Despite the advances in the neurosurgical techniques, the development of potent broad-spectrum antibiotics, better culturing and organism isolation techniques, and the increasing quality of neuroradiological imaging, yet, brain abscess still represents a major health challenge in developing countries in particular, with debates and controversies in its management.[
Brain abscess is a focal infection occurring within the brain parenchyma starting as a localized cerebritis, converted subsequently to a lesion of pus collection surrounded by a vascularized capsule.[
Brain abscess remains a challenge in developing and developed countries, accounting for 8% of intracranial lesions in developing and 2% in developed countries. The management and etiology remain unclear and complex, hindering the improvement of treatment and outcome.[
The dynamics in brain abscess remains a struggle between the infectious organism and immunocompetence of the host during the evolution from stages of early then late cerebritis to early and late capsule formation.[
Two primary surgical management had been utilized in brain abscess, either aspiration or open craniotomy excision. Stereotactic aspiration, ultrasound-guided aspiration, and endoscopic aspiration are different treatment options that have been used.[
Endoscopic aspiration allows the neurosurgeon to directly visualize the aspiration of the abscess content, meticulous inspection of the walls, ensuring complete aspiration of the purulent material, and hence minimizing the morbidity and the need for retapping.[
We are reporting our results in the endoscopic-assisted management of brain abscess.
MATERIALS AND METHODS
This study was done prospectively in the neurosurgery department in our institute on patients suffering from intracranial abscesses including 12 patients of brain abscesses treated between January 2015 and January 2018. Local ethical committee approval was obtained. An informed written consent was obtained from all patients.
Detailed history and proper examination were performed in all cases. All the patients performed either CT with contrast or MRI with contrast before deciding the management to assess site, size, multiloculation, surrounding edema, mass effect, and its relation to the ventricles.
Blood culture and inflammatory markers (total leukocyte count [TLC], erythrocyte sedimentation rate [ESR], and C-reactive protein [CRP]) were drawn as baseline for further assessment of the response to treatment.
Indications for surgery included patients with an abscesses >3 cm in diameter with significant mass effect, proximity to the ventricles, poor neurological condition, multiloculated abscess, and progression while on proper medical treatment.
Cases with small abscesses (<3 cm in diameter), abscess containing foreign bodies, multiple abscesses, and suspected fungal abscess were excluded from our study.
All the surgical interventions were performed under general anesthesia.
The aim of surgery is to reduce the intracranial pressure, confirm the diagnosis, and obtain pus for organism isolation and antibiotic sensitivity guidance which will enhance the efficacy of medical and avoiding intraventricular rupture in abscesses in close proximity to the ventricles.
Procedure
We used the rigid endoscope (Gaab system, Karl Storz GmbH and Co., Tuttlingen, Germany) in all cases.
Aspiration thorough a single burr hole was done in all the cases. The shortest trajectory to the lesion was planned without traversing through eloquent neural or vascular structures. (Image guided technique was used in 3 cases when available).
After the proper burr hole is performed, the dura exposed within this burr hole is opened in a cruciate manner; and brain cannula is inserted to ensure the presence of abscess and to obtain an undiluted specimen of pus. About 5 ml of pus should be aspirated which would be sent for Gram stain, cultures (aerobic and anaerobic), acid-fast stain for mycobacterium, TB, and fungal culture and sensitivity.
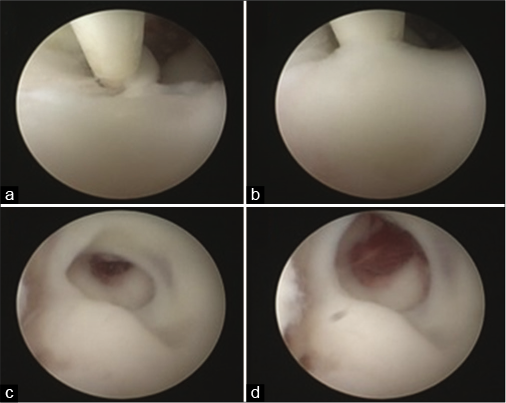
The sheath is then introduced through the performed burr hole into the abscess cavity followed by the working channel. The endoscopic view might be poor initially but later on it improves with frequent irrigation. Pus is then aspirated by gentle suction. The irrigation process must be done slowly through the irrigation channel of the sheath with maintaining the other channel open to guard against sudden increase in intracranial pressure. Simple suction tubes with small sizes were used to aspirate the fluidly parts of the content. They are soft and can be directed by moving the tip of the endoscope to the desired point. For the thicker parts, we fragmented them with the aid of the tip of Fogarty tube, followed by increasing the irrigation and then aspiration [
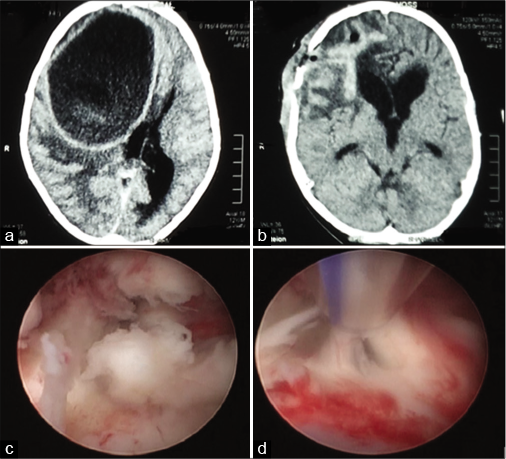
Figure 1:
(a) Preoperative CT showing the large abscess with mass effect. (b) Postoperative CT demonstrates the successful evacuation of the abscess using endoscopic techniques with resolution of the mass effect. (c) An intraoperative picture after proper irrigation which shows thick contents. (d) An intraoperative image showing the use of suction tube to aspirate thick contents.
Medications regimen
Broad-spectrum antimicrobial agents were used initially through intravenous route. They included vancomycin + third-generation cephalosporin + metronidazole. This triple therapy was continued until the results of the cultures appeared and then changed accordingly. The administration through intravenous route was continued for 4–6 weeks followed by oral antibiotics for another 4 weeks. Dehydrating measures were needed in cases with massive brain edema causing impairment of sensorium. Antiepileptic therapy was given pre- and postoperative.
Repeat CT scan was done in all cases within 1 and 4 weeks after surgery with follow-up of liver and kidney functions, ESR, CRP, and TLC. Follow-up ranged between 3 and 6 months.
RESULTS
Age and sex distribution
There were 8 males (66.7%) and 4 females (33.3%), with male-to-female ratio (2:1), ranging in age from 11 to 46 years (median 28.5years) at time of presentation.
Source of infection
There were 11 patients with either chronic otitis media, sinusitis, or both and only one patient suffered from congenital cyanotic heart disease.
Site of infection
The most common location was the temporal lobe 50% (6 cases) followed by the frontal lobe 42% (5 cases) and only 1 cerebellar abscess.
Mastoid surgery was done as a separate procedure after endoscopic surgery during the hospital stay.
Endoscopic view
We encountered multiloculations of the abscess cavity in 8 (66.7%) cases in which the septation in the cavity was opened endoscopically and complete evacuation of the purulent material was performed. The duration of surgery ranged from 60 to 90 min including the installation of the endoscopic set and the navigation if used together with the procedure duration itself. No redo surgery was done in our series.
Pathogen
Cultures revealed no growth in 42% (5 cases) while microorganisms were demonstrated in 7 (58%) patients; streptococcal was most frequent (42%); mixed infection occurred in 16% of abscesses.
At the time of presentation
About 75% of patients complained of headache, 33% had fever or other signs of meningeal irritation, 17% of patients complained of epilepsy, and focal neurological deficits were present in 42% of patients.
Glasgow coma score (GCS)
It was 5 in one patient, 13 in two cases, and 14–15 in nine cases.
Hospital stay
Hospital stay ranged from 14 to 45 days with an average of 28 days. The relatively long hospital stay is due to the fact that most of the patients’ accommodations were far away from our center with poor access to health-care facilities that could provide them the needed intravenous antibiotics treatment, together with the financial restrains that render the patients from continuation of the oral therapy thereafter.
Outcome
All the patients recovered completely except one who died from sepsis following complicated chest infection (with initial GCS 5). There was no procedure-related complication.
Case presentation
An 11-year-old boy, known to have congenital cyanotic heart disease, presented to the emergency room by disturbance of conscious level with a history of headache and left-sided heaviness. On examination, GCS was 14 with left-sided hemiparesis. Motor power was Grade 3 in the left upper limb and Grade 4 in the left lower limb. CT brain was done revealing large right frontal abscess with significant mass effect. The patient underwent emergency evacuation of the abscess through endoscopic approach through a burr hole in the right frontal bone. The abscess contents were evacuated successfully with the aid of the endoscopic visualization after proper irrigation was done. The introduction of suction tubes allowed the removal of thick contents to ensure proper evacuation. GCS and hemiparesis improved markedly postoperatively, the patient stayed in the hospital till completion of the treatment regimen then he was discharged and followed up.
DISCUSSION
There is a constant debate among neurosurgeons regarding the best strategy for brain abscess management whether minimally invasive aspiration or complete excision. Although simple aspiration through a burr hole had been the gold standard of treatment for being highly effective, less morbid, and with shorter hospital stay,[
The obsession of recurrence usually pushes some neurosurgeons to adopt the complete excision policy.[
However, this option seems to be unsuitable in some cases such as deeply seated abscess, multiple abscesses, or abscess in eloquent brain area where excision should not be considered.[
The endoscopic aspiration and lavage can conciliate between both parties, being minimally invasive procedure, and in the same time, it can promote the speedy recovery without recurrences by overcoming the multiloculation of the abscess cavity, plus ensuring of complete aspiration of the content by visual confirmation, which, in turn, would decrease the number of cases in which excision is required. In this concern, we did not encounter any recurrence in our cases despite the presence of multiloculation of abscess cavity in 8 cases (66.7%). We dealt with these loculations by opening of the septations under visual control, making the treatment of multiloculated abscess a doable endoscopic procedure, and abolishing the need of reverting to excision through a craniotomy. Similar results were obtained by Yadav et al. who have no recurrences in their series utilizing the endoscopy.[
Of course, one can feel more safe with endoscopic management rather than the blind stereotactic aspiration. The blessing of visualization in endoscopy cannot be missed. Despite the prefixed fears from the thick contents of the cavity that might render proper vision, yet with continuous lavage and patience, the picture starts to clear out permitting the procedure completion with high degree of safety and confidence. Moreover, we can avoid the potential drawbacks of deficient direct visual control that may happen in the standalone stereotactic procedures like the unseen collapse of capsule postaspiration which might lead to catheter slippage outside the abscess cavity.[
Being challenging to locate the brain abscesses, there are several reports in the literature about navigating options such as stereotactic control,[
The thick texture of the pus can raise the concern about the efficacy of endoscopic instruments to accomplish the aspiration of the contents within the abscess cavity. In fact, we used effective, easy to handle, and nonexpensive tools, adding no extra expenses in the developing countries which, in turn, makes the endoscopic procedures more affordable. In difficult cases, one can use ultrasonic aspiration in combination with endoscopy as reported by Spennato et al.[
Postoperative bleeding in brain abscess can occur and may be attributed to inflammation and hypoxic damage of the weak neovascularity of the brain abscess lacking supportive tissues,[
Finally, our results and experience in the endoscopic treatment of brain abscess were encouraging and we advocate it as an effective and safe way of treatment.
CONCLUSION
Endoscopic aspiration of brain abscesses can help in complete aspiration of contents together with the ability to control any bleeding points. It can be used in multiloculated abscess safely and effectively due to the advantages of proper visualization provided by the endoscope, which, in turn, can omit the need of craniotomy and excision.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Atiq M, Ahmed US, Allana SS, Chishti KN. Brain abscess in children. Indian J Pediatr. 2006. 73: 401-4
2. Bhand AA. Brain abscess-diagnosis and management. J Coll Physicians Surg Pak. 2004. 14: 407-10
3. Boviatsis EJ, Kouyialis AT, Stranjalis G, Korfias S, Sakas DE. CT-guided stereotactic aspiration of brain abscesses. Neurosurg Rev. 2003. 26: 206-9
4. Chowdhury F, Haque M, Sarkar M, Chowdhury SM, Hossain Z, Ranjan S. Brain abscess: Surgical experiences of 162 cases. Neuroimmunol Neuroinflamm. 2015. 2: 153
5. Ciurea AV, Stoica F, Vasilescu G, Nuteanu L. Neurosurgical management of brain abscesses in children. Childs Nerv Syst. 1999. 15: 309-17
6. Fritsch M, Manwaring KH. Endoscopic treatment of brain abscess in children. Minim Invasive Neurosurg. 1997. 40: 103-6
7. Gajdhar M, Yadav YR. A case of thalamic abscess treated by endoscopic surgery. Neurol India. 2005. 53: 345-6
8. Hakan T. Management of bacterial brain abscesses. Neurosurg Focus. 2008. 24: E4
9. Hellwig D, Bauer BL, Dauch WA. Endoscopic stereotactic treatment of brain abscesses. Acta Neurochir Suppl. 1994. 61: 102-5
10. Longatti P, Perin A, Ettorre F, Fiorindi A, Baratto V. Endoscopic treatment of brain abscesses. Childs Nerv Syst. 2006. 22: 1447-50
11. Miranda HA, Leones SM, Elzain MA, Moscote-Salazar LR. Brain abscess: Current management. J Neurosci Rural Pract. 2013. 4: S67-81
12. Muzumdar D, Jhawar S, Goel A. Brain abscess: An overview. Int J Surg. 2011. 9: 136-44
13. Ortega-Martínez M, Cabezudo JM, Fernández-Portales I, Gómez-Perals L, Rodríguez-Sánchez JA, García-Yagüe L. Pyogenic brain abscesses: Experience with 60 consecutive cases. Neurocirugia (Astur). 2006. 17: 23-33
14. Ozgural O, Al-Beyati ES, Kahilogullari G. MR navigation and tractography-assisted transcranial neuroendoscopic aspiration of pediatric thalamic abscess. Pediatr Neurosurg. 2019. 54: 354-8
15. Patel K, Clifford DB. Bacterial brain abscess. Neurohospitalist. 2014. 4: 196-204
16. Sharma BS, Gupta SK, Khosla VK. Current concepts in the management of pyogenic brain abscess. Neurol India. 2000. 48: 105-11
17. Spennato P, Aliberti F, Colaleo F, Mirone G, di Martino G, Cinalli G. Endoscopic ultrasonic aspiration of brain abscess. Childs Nerv Syst. 2018. 34: 1579-82
18. Wilson HL, Kennedy KJ. Scedosporium apiospermum brain abscesses in an immunocompetent man with silicosis. Med Mycol Case Rep. 2013. 2: 75-8
19. Yadav Y, Sinha M, Neha Parihar V. Endoscopic management of brain abscesses. Neurol India. 2008. 56: 13-6