- Department of Basic Sciences, School of Osteopathic Medicine, Touro University Nevada, Henderson, Nevada, United States.
- Department of Neurosurgery, University of California San Diego School of Medicine, San Diego, California, United States.
Correspondence Address:
Omron Hassan
Department of Neurosurgery, University of California San Diego School of Medicine, San Diego, California, United States.
DOI:10.25259/SNI_166_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Omron Hassan, Courtney S. Lewis, Likitha Aradhyula, Brian R. Hirshman, Martin H. Pham. Engorged venous plexus mimicking adjacent segment disease: Case report and review of the literature. 09-May-2020;11:104
How to cite this URL: Omron Hassan, Courtney S. Lewis, Likitha Aradhyula, Brian R. Hirshman, Martin H. Pham. Engorged venous plexus mimicking adjacent segment disease: Case report and review of the literature. 09-May-2020;11:104. Available from: https://surgicalneurologyint.com/surgicalint-articles/10007/
Abstract
Background: An engorged venous plexus may mimic nerve compression from a herniated disk on the magnetic resonance (MR) studies as they both have similar signal intensities. During a laminectomy, if an engorged venous plexus is encountered instead of a disk herniation, there may be marked unanticipated bleeding.
Case Description: A 58-year-old female who had a prior anterior lumbar interbody fusion later returned with recurrent radiculopathy. Adjacent segment disease from a spinal disk herniation was suspected based on the surgical history, physical examination, and imaging (MRI) findings. Rather than a disk, an engorged venous plexuses (EVP) was encountered intraoperatively.
Conclusion: Here, we discussed our findings regarding a lumbar EVP rather than a herniated disk and reviewed the current literature. Although rare, a higher index of suspicion for these vascular malformations based on combined historical information and MRI studies should allow one to better detect and/or anticipate an EVP rather than a routine disk.
Keywords: Adjacent segment disease, Epidural venous plexus, Lumbar radiculopathy
INTRODUCTION
Patients, who previously had spinal fusions, may develop recurrent lumbar radiculopathy due to adjacent-level disk herniations. However, new adjacent level disease may occasionally be attributed to engorged venous plexuses (EVP) rather than new disk herniations.[
Here, we present a 58-year-old female patient who had previously undergone an anterior lumbar interbody fusion (ALIF) but later returned with lumbar radiculopathy. Although adjacent segment disease from a new spinal disk herniation was suspected, particularly based on relatively routine MRI findings, an EVP was discovered intraoperatively and was appropriately excised.
CASE REPORT
Clinical presentation
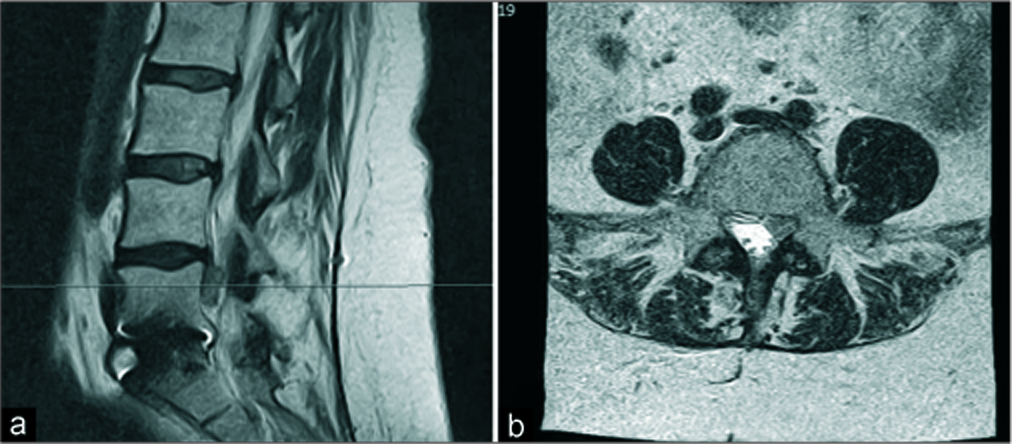
A 58-year-old female presented with the left lower radiculopathy. Seven years ago, she had a prior L5-S1 ALIF. On examination she had decreased the left lower-extremity 1/5 motor function in the tibialis anterior and extensor hallucis longus distributions, plus a 3/5 in the gastrocnemius. The MRI showed what appeared to be an L4-L5 left-sided disk herniation above the level of her prior fusion (i.e., adjacent L4-L5 segment disk disease) [
Operative course
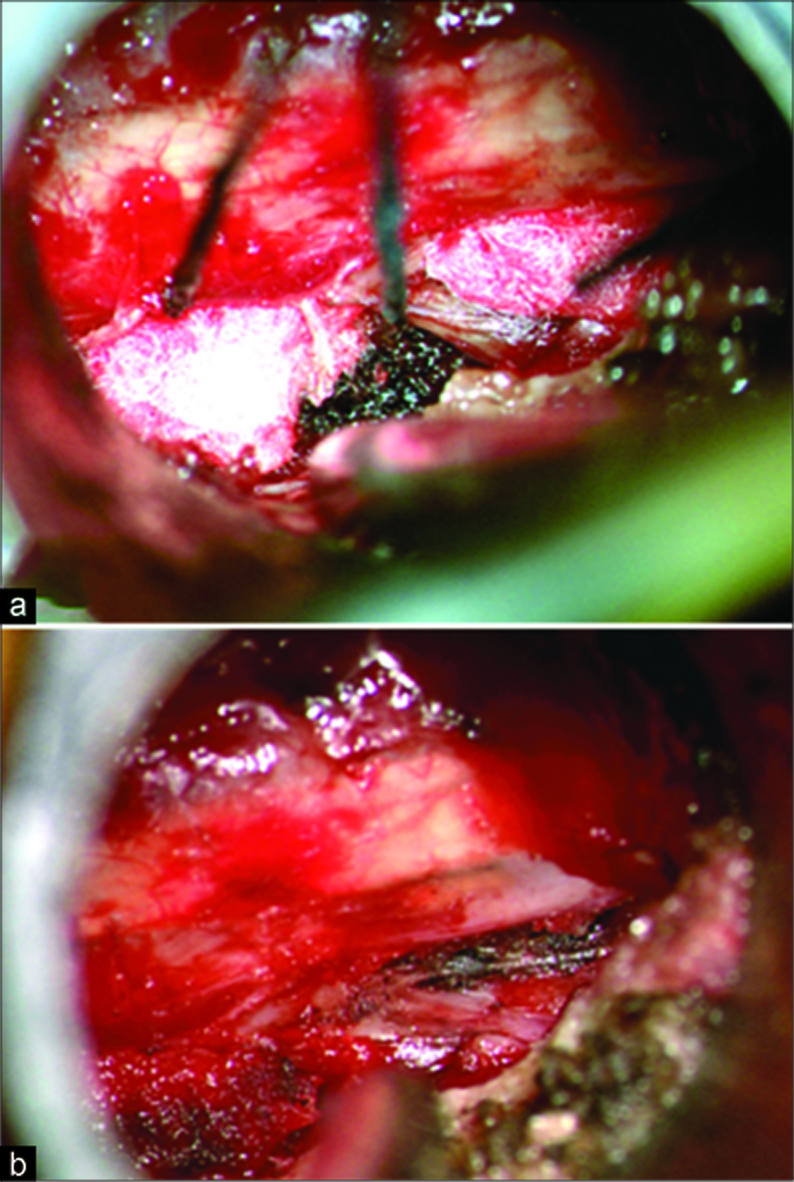
She subsequently underwent an L4-L5 left-sided minimally invasive microdiscectomy. After the laminotomy was completed and nerve root identified, there was a large venous plexus in the nerve root axilla extending ventrally and laterally. This was successfully coagulated with bipolar cautery. Due to the fragility of the plexus and recurrent venous bleeding, multiple hemostatic agents were repeatedly employed to control the bleeding [
Figure 2:
Intraoperative view down the minimally invasive tubular retractor showing (a) the lateral edge of the dural and nerve root with cottonoids and Surgicel® hemostatic material at both the nerve root shoulder and axilla after encountering copious venous bleeding. (b) View of the nerve root after exploration which demonstrated no herniated disk bulge or fragment.
Outcome and follow-up
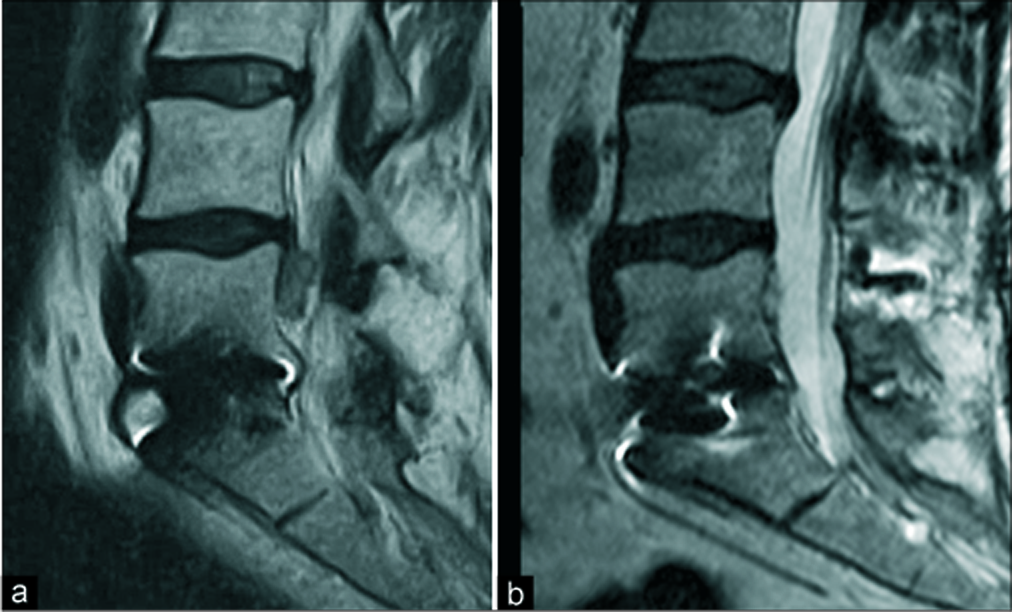
Postoperatively, she reported immediate improvement of her foot strength and resolution of her left lower extremity and buttock pain. She was discharged on postoperative day 1 after a follow-up MRI confirmed an EVP as the ultimate etiology of her radiculopathy [
DISCUSSION
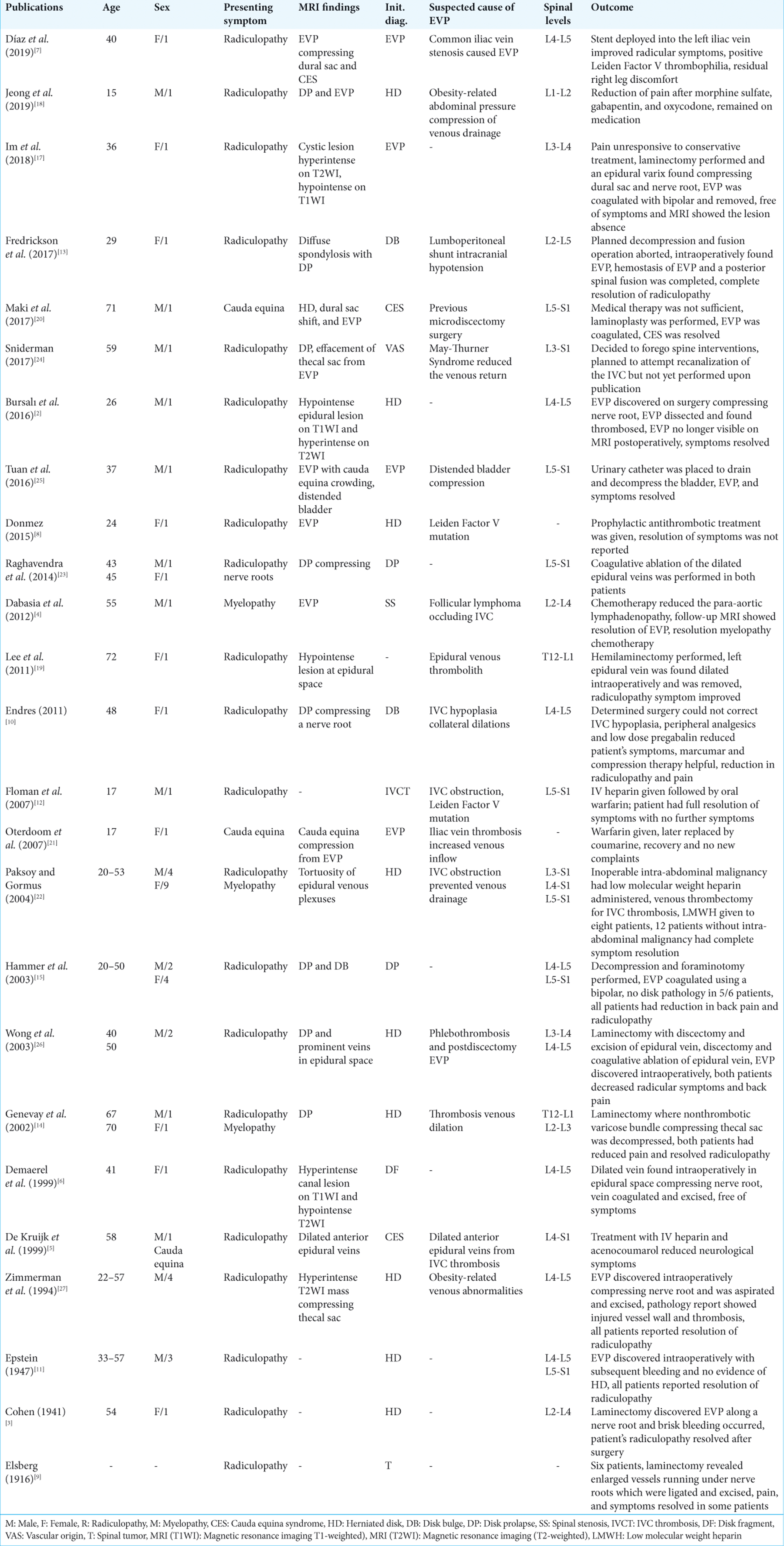
A review of the English-language literature demonstrated 25 reports ranging in publication year between 1916 and 2019 that described patients with EVPs who presented similarly to those with lumbar disk herniations [
Location and pathology of EVPs
EVPs are variously attributed to IVC thrombosis/hypoplasia and iliac vein stenosis. EVPs in the lumbar region represent dilations of the vertebral venous plexus system resulting from either increased blood flow or disrupted venous drainage. Notably, EVP at the cervical and thoracic levels have different regional etiologies.[
Encountering unanticipated EVPs during lumbar surgery
Although rare, clinicians should consider EVPs in their differential diagnosis when encountering patients with radiculopathy who also have a history of obesity, vascular conditions, current pregnancy, or are taking oral contraceptives.[
Differentiating between EVP and disk on MRI
Differentiating between EVPs and herniated disks can be difficult, as both have similar MRI appearances. However, lumbar disk herniations typically appear hypo/hyperintense on MRI reflecting their water content.[
CONCLUSION
We report a 58-year-old female with a lumbar EVP above the level of a prior L5-S1 ALIF. Although rare, EVP should be anticipated if additional EVP-related MRI findings are present.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
There were no conflicts of interest or sources of funding for this work.
References
1. Amano E, Ozaki K, Egawa S, Suzuki M, Hirai T, Ishibashi S. Dynamic spinal compression revealed by computed tomography myelography in overshunting-associated myelopathy: A case report. Medicine (Baltimore). 2018. 97: e0082-
2. Bursalı A, Akyoldas G, Guvenal AB, Yaman O. Lumbar epidural varix mimicking disc herniation. J Korean Neurosurg Soc. 2016. 59: 410-3
3. Cohen I. Extradural varix simulating herniated nucleus pulposus. J Mt Sinai Hosp N Y. 1941. 8: 136-8
4. Dabasia H, Rahim N, Marshall R. Neurogenic claudication without spinal stenosis arising as a result of lumbar epidural varices. J Bone Joint Surg Br. 2012. 94: 1292-4
5. de Kruijk J, Korten A, Boiten J, Wilmink J. Acute cauda equina syndrome caused by thrombosis of the inferior vena cava. J Neurol Neurosurg Psychiatry. 1999. 67: 827-8
6. Demaerel P, Petré C, Wilms G, Plets C. Sciatica caused by a dilated epidural vein: MR findings. Eur Radiol. 1999. 9: 113-4
7. Díaz CT, Allegue NA, Sala DG, Martins GG, Torremorell MB, Montoya SB. Cauda equina syndrome caused by epidural venous plexus engorgement in a patient with may-thurner syndrome. Ann Vasc Surg. 2019. 60: 480.e7-480.e11
8. Donmez FY. Epidural venous plexus engorgement: What lies beneath?. Case Rep Radiol. 2015. 2015: 965106-
9. Elsberg CA. The surgical significance and operative treatment of enlarged and varicose veins of the spinal cord. Am J Med Sci. 1916. 151: 78-86
10. Endres S. Epidural varicosis as a possible cause of radicular pain: A case report. J Med Case Rep. 2011. 5: 537-
11. Epstein BS. Low back pain associated with varices of the epidural veins simulating herniation of the nucleus pulposa. Am J Roentgenol Radium Ther. 1947. 57: 736-40
12. Floman Y, Smorgick Y, Rand N, Bar-Ziv J. Inferior vena cava thrombosis presenting as lumbar radiculopathy. Am J Phys Med Rehabil. 2007. 86: 952-5
13. Fredrickson VL, Patel A, Pham MH, Strickland BA, Ohiorhenuan I, Chen T. Spine surgery complicated by an engorged lumbar epidural venous plexus from cerebrospinal fluid overshunting: A case report and review of the literature. World Neurosurg. 2018. 111: 68-72
14. Genevay S, Palazzo E, Huten D, Fossati P, Meyer O. Lumboradiculopathy due to epidural varices: Two case reports and a review of the literature. Joint Bone Spine. 2002. 69: 214-7
15. Hammer A, Knight I, Agarwal A. Localized venous plexi in the spine simulating prolapse of an intervertebral disc: A report of six cases. Spine (Phila Pa 1976). 2003. 28: E5-12
16. Hanley EN, Howard BH, Brigham CD, Chapman TM, Guilford WB, Coumas JM. Lumbar epidural varix as a cause of radiculopathy. Spine (Phila Pa 1976). 1994. 19: 2122-6
17. Im IK, Son ES, Kim DH. Lumbar epidural varix causing radicular pain: A case report and differential diagnosis of lumbar cystic lesions. PM R. 2018. 10: 1283-7
18. Jeong HJ, Sim WS, Park HJ, Lee SH, Oh MS, Cho MK. Severe lumbar radiculopathy with epidural venous plexus engorgement in a morbidly obese pediatric patient: A case report. Medicine (Baltimore). 2019. 98: e16842-
19. Lee YS, Choi ES, Kim JO, Ji JH. A rare calcified thrombosis of the dilated epidural venous plexus presenting with lumbar radiculopathy: A case report. Spine J. 2011. 11: e28-31
20. Maki Y, Takayama M, Hayashi H, Yokoyama Y, Agawa Y. Cauda equina syndrome due to dural sac shift with engorgement of the epidural venous plexus: Rare complication after lumbar microdiscectomy. World Neurosurg. 2017. 104: e15-1048
21. Oterdoom DL, de Jong BM, Hoogland PV, Groen RJ. Transient cauda equina compression syndrome and headache caused by internal vertebral venous plexus engorgement in a teenage female with vena cava inferior agenesis and iliac vein thrombosis. J Neurol Neurosurg Psychiatry. 2007. 78: 1283-4
22. Paksoy Y, Gormus N. Epidural venous plexus enlargements presenting with radiculopathy and back pain in patients with inferior vena cava obstruction or occlusion. Spine (Phila Pa 1976). 2004. 29: 2419-24
23. Raghavendra V, Haridas P, Kumar A, Ajith k. Spinal epidural varices, a great mimic of intervertebral disc prolapse-a case series. J Orthop Case Rep. 2014. 4: 3-5
24. Sniderman M. Epidural injections contraindicated for lumbar radiculopathy in may-thurner syndrome: A case report. A A Case Rep. 2018. 9: 294-6
25. Tuan AS, Nabavizadeh SA, Pukenas B, Mohan S, Learned KO. Reversible dilatation of lumbar epidural venous plexus secondary to pelvic venous compression: Mimicker of pathology. BJR Case Rep. 2017. 3: 20150287-
26. Wong CH, Thng PL, Thoo FL, Low CO. Symptomatic spinal epidural varices presenting with nerve impingement: Report of two cases and review of the literature. Spine (Phila Pa 1976). 2003. 28: E347-50
27. Zimmerman GA, Weingarten K, Lavyne AM. Transient cauda equina compression syndrome and headache caused by internal vertebral venous plexus engorgement in a teenage female with vena cava inferior agenesis and iliac vein thrombosis. J Neurosurg. 1994. 80: 914-8