- Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
- Department of Pathological Anatomy, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
Correspondence Address:
M. Dobran
Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
DOI:10.4103/sni.sni_142_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: M. Dobran, D. Brancorsini, M. Della Costanza, V. Liverotti, F. Mancini, D. Nasi, M. Iacoangeli, M. Scerrati. Epidural scarring after lumbar disc surgery: Equivalent scarring with/without free autologous fat grafts. 01-Aug-2017;8:169
How to cite this URL: M. Dobran, D. Brancorsini, M. Della Costanza, V. Liverotti, F. Mancini, D. Nasi, M. Iacoangeli, M. Scerrati. Epidural scarring after lumbar disc surgery: Equivalent scarring with/without free autologous fat grafts. 01-Aug-2017;8:169. Available from: http://surgicalneurologyint.com/surgicalint-articles/epidural-scarring-after-lumbar-disc-surgery-equivalent-scarring-withwithout-free-autologous-fat-grafts/
Abstract
Background:To limit epidural fibrosis and prevent scar formation/nerve tethering that may contribute to chronic postoperative pain; some surgeons have utilized epidural autologous fat grafts following lumbar microdiscectomy.
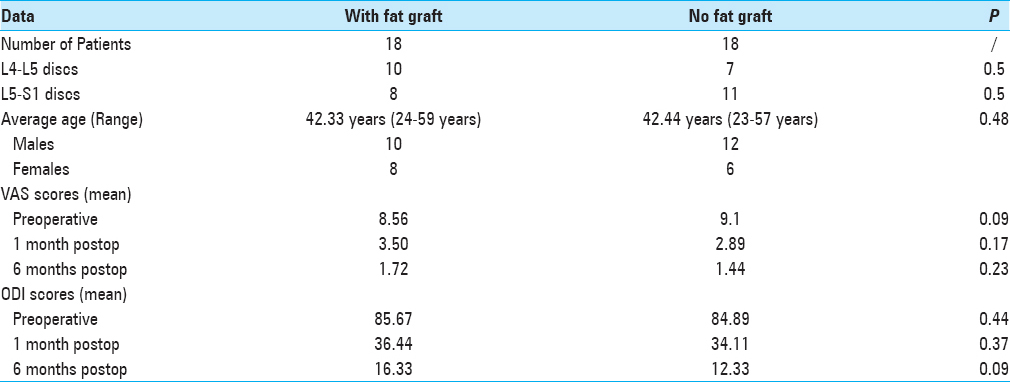
Methods:We investigated the correlation between post-microdiscectomy epidural scarring [including select magnetic resonance imaging (MRI) studies] and clinical outcomes in 36 patients operated for symptomatic. MRI documented L4-L5 and L5-S1 disk herniations with (18 patients) and without (18 patient) the application of free fat grafts. In addition, histological evaluation of the original fat grafts was performed in 4 patients requiring additional surgery.
Results:We found no clear association between the use of autologous graft fats and the clinical outcomes in this study.
Conclusion:In this preliminary study involving only 36 patients, the prospective randomized use of free autologous fat grafts did not appear to influence outcomes following microdiscectomy.
Keywords: Epidural fibrosis, failed back syndrome, microdiscectomy, post-discectomy syndrome
INTRODUCTION
Epidural fibrosis following spinal surgery occurs because fibrotic tissue replaces epidural fat. For many years, the application of free fat grafts after microdiscectomy had been widely used to prevent epidural scarring, but the results were controversial.[
MATERIALS AND METHODS
Lumbar microdiscectomies (interlaminar approaches) were performed at the L4-L5 (17 patients) and L5-S1 (19 patients) levels in 36 patients, with an average age of 39.4 years [
Outcomes, MRI, and statistical postoperative analyses
Preoperatively, all patients underwent MRI studies, as well as evaluations utilizing the visual analogue scale (VAS) and Oswestry Disability Index (ODI) scores. Postoperatively, the VAS and ODI were repeated at 1 and 6 months in all patients, whereas MRI studies were randomly obtained at 6 postoperative months in only 15 patients (8 without fat grafts and 7 with fat grafts). Statistics analyses were performed utilizing the paired t-test (a P value less than 0.05 was considered significant).
RESULTS
Operative data and clinical outcome
For both groups, the mean operative time was 60 and the mean length of hospital stay was 4 days. The mean preoperative and all postoperative (1 month, 6 months) ODI and VAS scores remained comparable for both groups [
Epidural fibrosis on MRI and clinical outcome
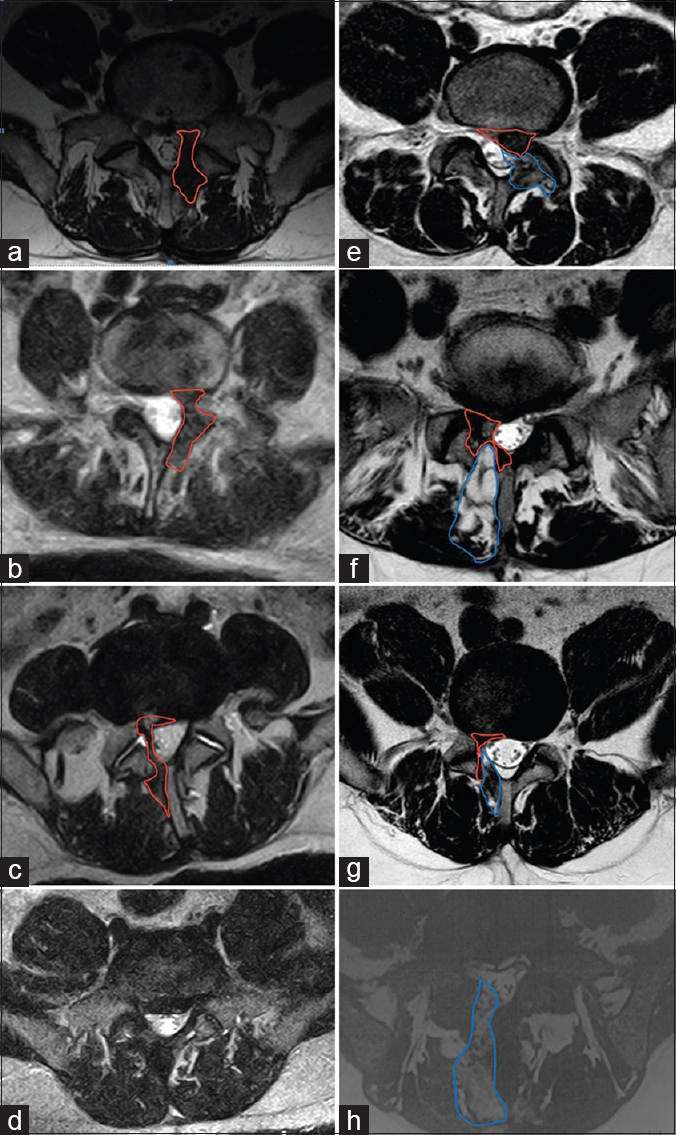
Select postoperative MRI scans were randomly performed in 15 patients (excluding the four patients operated on early after their first surgery for complications). These studies showed no correlation between epidural fibrosis and symptoms. In fact, 6 patients exhibited MR-documented focal compression of the dural sac but were asymptomatic (e.g., no symptoms, no deficits).
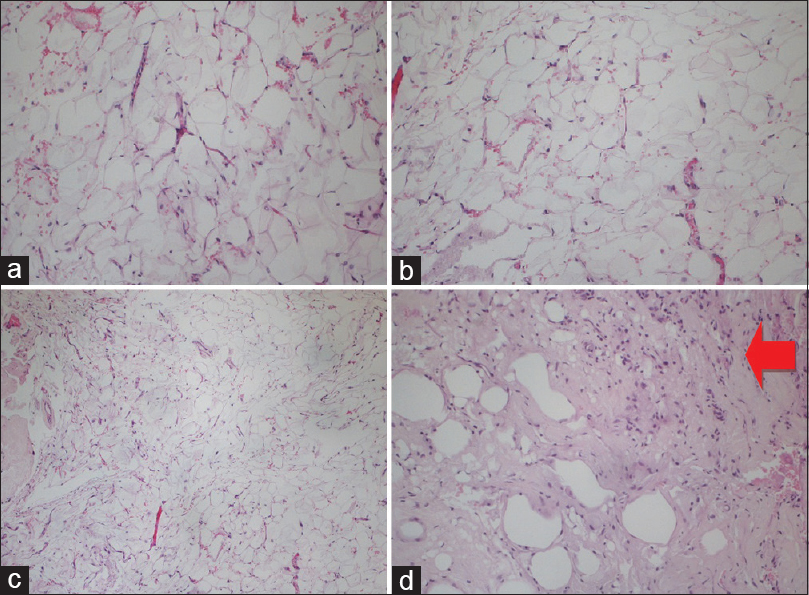
Postoperative complications and histological evaluation of the fat graft
One month post-operatively, 1 patient required secondary surgery (laminectomy/fusion) to address a lumbar fracture.[
DISCUSSION
The epidural fibrosis around dura mater and nerve roots at the operative site after microdiscectomy is a possible cause of failed back syndrome. Nerve fibers encased in collagenous scar tissue suffer an increase in neural tension, impairment of axoplasmic transport, and restriction of arterial supply and venous return. Compression of nerve tissue can induce clinical symptoms such as numbness, pain, and muscle weakness.[
In this series, the histology of the removed fat graft in 2 patients showed normal amounts of fibroblasts in the fat graft, whereas a third showed colonization by fibroblasts.
In the present study, the absence of the autologous free fat graft in microdiscectomy was not correlated with scar formation on select MRI images [
Figure 2
Axial MRI T2W images at the level of surgical access. (a-c) Patients operated without autologous graft-fat with evidence of scar tissue formation (red line). (d) Patient operated without autologous graft-fat without sign of scar tissue. (e-g) Patients operated with positioning of autologous fat-graft (blue line) and evidence of scar formation (red line) (h) Patient operated with positioning of autologous fat-graft (blue line), without sign of scar tissue formation
CONCLUSION
In conclusion, as documented in this study, the use of peridural free fat grafts following lumbar microdiscectomy did not change the clinical outcome. Furthermore, select MRI images documented that free autologous fat grafts did not prevent postoperative scar formation. Moreover, the main cause of persistence of pain after microdiscectomy in our series was related to insufficiency of first surgery (inadequate disc removal/nerve root decompression), as demonstrated in the three patients with early disc herniation recurrences.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Annertz M, Jonsson B, Strömqvist B, Holt S. No relationship between epidural fibrosis and sciatica in the lumbar postdiscectomy syndrome: A study with contrast-enhanced magnetic resonance imaging in symptomatic and asymptomatic patients. Spine (Phila Pa 1976). 1995. 20: 449-53
2. Coskun E, Suzer T, Topuz O, Zencir M, Pakdemirli E, Tahta K. Relationships between epidural fibrosis, pain, disability, and psychological factors after lumbar disc surgery. Eur Spine J. 2000. 9: 218-23
3. Dobran M, Iacoangeli M, Nasi D, Nocchi N, Di Rienzo A, Di Somma L. Posterior titanium screw fixation without debridemenet of infected tissue for the treatment of thoracolumbar spontaneous pyogenic spondylodiscitis. Asian Spine J. 2016. 10: 465-71
4. Dobran M, Iacoangeli M, Di Somma LGM, Di Rienzo A, Colasanti R, Nocchi N. Neurological outcome in a series of 58 patients operated for traumatic thoracolumbar spinal cord injuries. Surg Neurol Int. 2014. 5: S329-32
5. Dobran M, Nasi D, Brunozzi D, Di Somma L, Gladi M, Iacoangeli M. Treatment of unstable thoracolumbar junction burst fractures: Short-segment pedicle fixation with inclusion of fracture level versus long-term instrumentation. Acta Neurochir (Wien). 2016. 158: 1883-9
6. Geisler FH. Prevention of peridural fibrosis: Current methodologies. Neurol Res. 1992. 21: S9-22
7. Martin-Ferrer S. Failure of autologous fat grafts to prevent post operative epidural fibrosis in surgery of the lumbar spine. Neurosurgery. 1989. 24: 718-21
8. Merrild U, Sogaard IB. Sciatica caused by perifibrosis of the sciatic nerve. J Bone Joint Surgery. 1986. 68: 706-