- Department of Neurosurgery, Getúlio Vargas University Hospital, Federal University of Amazonas, Manaus,
- Department of Neurosurgery, Santa Casa de São Paulo, São Paulo,
- Faculty of Medicine, Faculdade Metropolitana de Manaus, Manaus,
- Division of Neurosurgery, Hospital das Clínicas, University of São Paulo Medical School, São Paulo,
- Department of Neurology, Hospital Samaritano de São Paulo, São Paulo, Brazil.
Correspondence Address:
Daniel Buzaglo Gonçalves, Faculty of Medicine, Federal University of Amazonas, Manaus, Amazonas, Brazil.
DOI:10.25259/SNI_485_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniel Buzaglo Gonçalves1, Maria Izabel Andrade dos Santos1, Lucas de Cristo Rojas Cabral1, Louise Makarem Oliveira1, Gabriela Campos da Silva Coutinho1, Bruna Guimarães Dutra1, Rodrigo Viana Martins2, Franklin Reis1,3, Wellingson Silva Paiva4,5, Robson Luis Oliveira de Amorim1,4. Esthetics outcomes in patients submitted to pterional craniotomy and its variants: A scoping review. 13-Sep-2021;12:461
How to cite this URL: Daniel Buzaglo Gonçalves1, Maria Izabel Andrade dos Santos1, Lucas de Cristo Rojas Cabral1, Louise Makarem Oliveira1, Gabriela Campos da Silva Coutinho1, Bruna Guimarães Dutra1, Rodrigo Viana Martins2, Franklin Reis1,3, Wellingson Silva Paiva4,5, Robson Luis Oliveira de Amorim1,4. Esthetics outcomes in patients submitted to pterional craniotomy and its variants: A scoping review. 13-Sep-2021;12:461. Available from: https://surgicalneurologyint.com/surgicalint-articles/11110/
Abstract
Background: Highly performed nowadays, the pterional craniotomy (PC) has several widespread variants. However, these procedures are associated with complications such as temporalis muscle atrophy, facial nerve frontal branch damage, and masticatory difficulties. The postoperative cranial aesthetic is, nonetheless, the main setback according to patients. This review aims to map different pterional approaches focusing on final aesthetics.
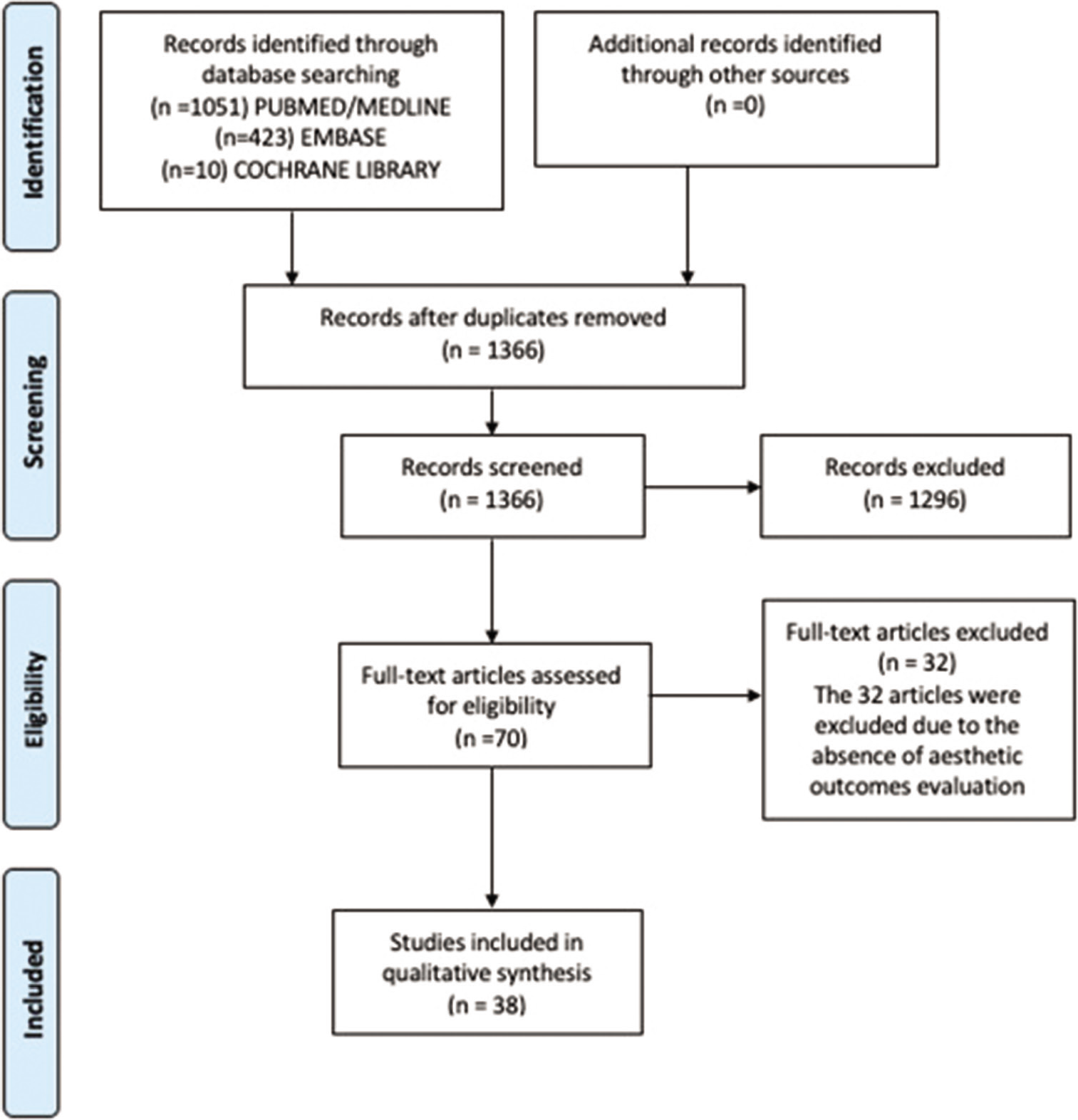
Methods: This review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. Studies were classified through the Oxford method. We searched PubMed/MEDLINE, EMBASE, and Cochrane Library from January 1969 to February 2021 for cohorts and randomized clinical trials that met our inclusion criteria.
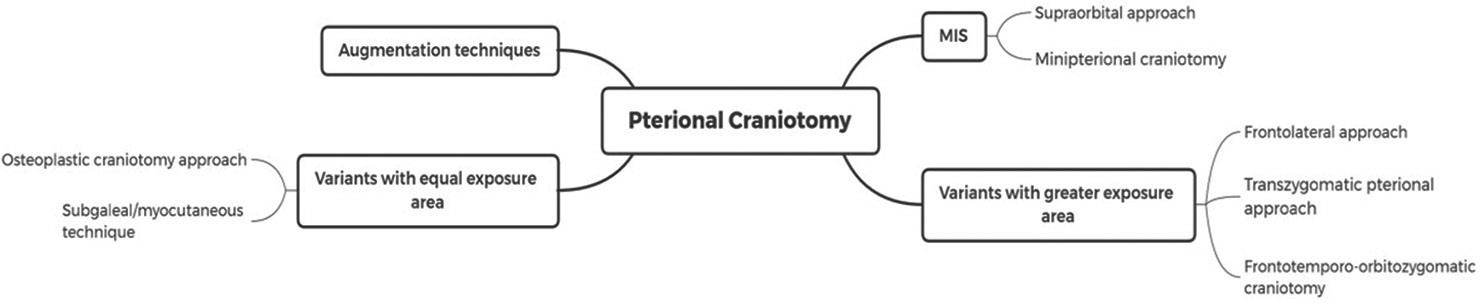
Results: 1484 articles were initially retrieved from the databases. 1328 articles did not fit the inclusion criteria. 118 duplicates were found. 38 studies were found eligible for the established criteria. 27 (71.05%) were retrospective cohorts, with low evidence level. Only 5 (13.15%) clinical trials were found eligible to the criteria. The majority of the studies (36/38) had the 2B OXFORD evidence level. A limited number of studies addressed cosmetic outcomes and patient satisfaction. The temporal muscle atrophy or temporal hollowing seems to be the patient’s main complaint. Only 17 (44.73%) studies addressed patient satisfaction regarding the aesthetics, and only 10 (26.31%) of the studies reported the cosmetic outcome as a primary outcome. Nevertheless, minimally invasive approaches appear to overcome most cosmetic complaints and should be performed whenever possible.
Conclusion: There are several variants of the classic PC. The esthetic outcomes are poorly evaluated. The majority of the studies were low evidence articles.
Keywords: Esthetic outcomes, Patient reported outcomes, Pterional craniotomy
INTRODUCTION
Pterional craniotomy (PC) is a classic approach for all anterior circulation aneurysms, suprasellar tumors (i.e., pituitary adenomas and craniopharyngiomas), and neurosurgeries where the opening of the Sylvian fissure is a crucial step.[
MATERIALS AND METHODS
Search strategy
This scoping review was made using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement extension for scoping reviews.[
Study selection
This study intended to gather randomized clinical trials and cohort studies that compared different types of PC from the esthetics point of view. Inclusion criteria were: (a) studies that evaluated PC and its variants, in terms of aesthetics outcomes, (b) randomized clinical trial and cohort studies, and (c) articles written in English, Spanish, and Portuguese. Conversely, we excluded review articles, editorials, letters, comments, and articles that had no related theme to this study, case/series reports, or studies that evaluated the reconstructive surgeries for esthetic repair.
Data extraction
Two researchers (D.B.G and M.I.A.S) selected the studies. Divergences among the article selection as well as to the quality assessment were evaluated by the senior author. The following data were extracted from the studies: (1) general details on the study (author, year of publication, country, study type, time of follow-up, number of patients); (2) type of pterional approach; (3) baseline disease; (4) esthetic outcomes; and (5) complications.
Quality assessment
Studies were classified according to the Oxford method. The quality of the only randomized clinical trial that met the final criteria was assessed trough the JADAD score.[
RESULTS
One thousand four hundred and eighty-four articles were retrieved. 38 studies were found eligible for the established criteria (27 retrospective cohort studies, one outcome research, four prospective cohorts, one case–control, and five clinical trials).[
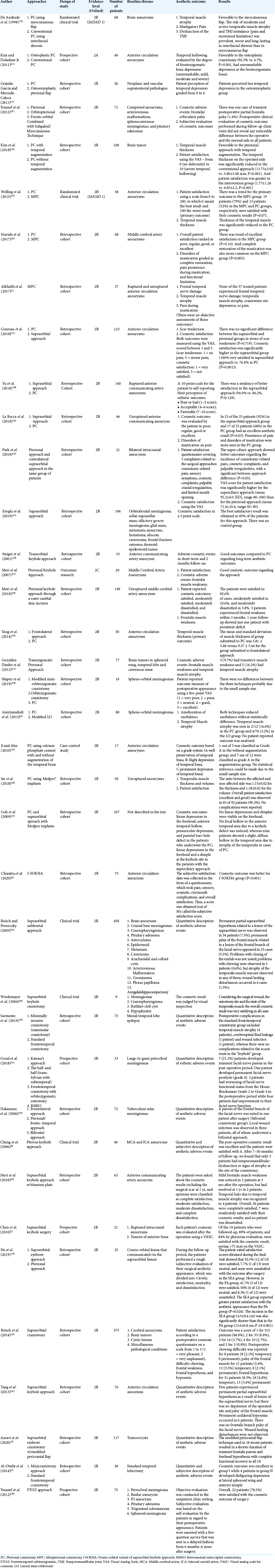
Among the cohorts, four were prospective studies. Most of the articles studied the cosmetic/aesthetic outcomes in intracranial brain aneurysms (27/38). The primary outcomes analyzed were the temporal muscle atrophy (TMA) and frontal nerve palsy, evaluated quantitatively or qualitatively (through patients or health professionals reported outcomes). Over 50% of the studies (31/38) considered aesthetic as a secondary outcome. All main information from each included study are summarized in [
We have identified five studies that compare PC and minimally invasive surgery (MIS) understood as minipterional craniotomy (MPC) and supraorbital variants approach. [
DISCUSSION
At present, PC is still the most widely used craniotomy to approach vascular and neoplastic diseases in neurosurgical practice.[
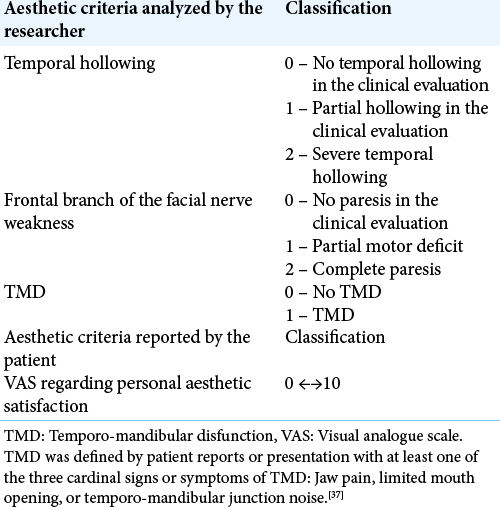
Due to the heterogeneity of the esthetic evaluations carried out among the studies analyzed, we identified that for the purposes of evaluating of aesthetic outcomes, it is important that the evaluation is standardized and that it considers the patient’s evaluation. We identified that the most important aspects to be assessed by the researcher are: temporal hollowing, paresis of the frontal branch of the facial nerve, temporo-mandibular dysfunction, and patient’s visual analogue scale proposed in [
TMA
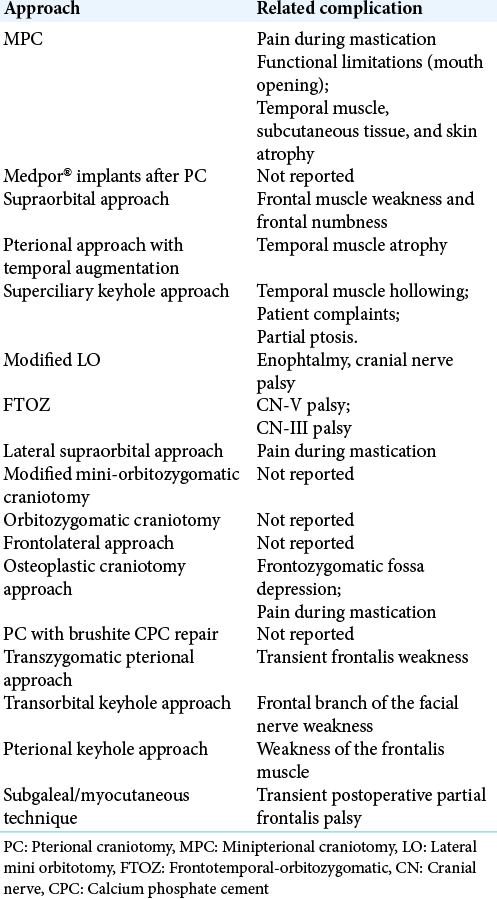
The TMA or temporal hollowing seems to be the chief complaint of the patients regarding the esthetics issue. Temporal hollowing can cause significant craniomaxillofacial asymmetry, esthetic deformity, and serious cosmetic concern in patients, even when there is an excellent postoperative functional outcome [
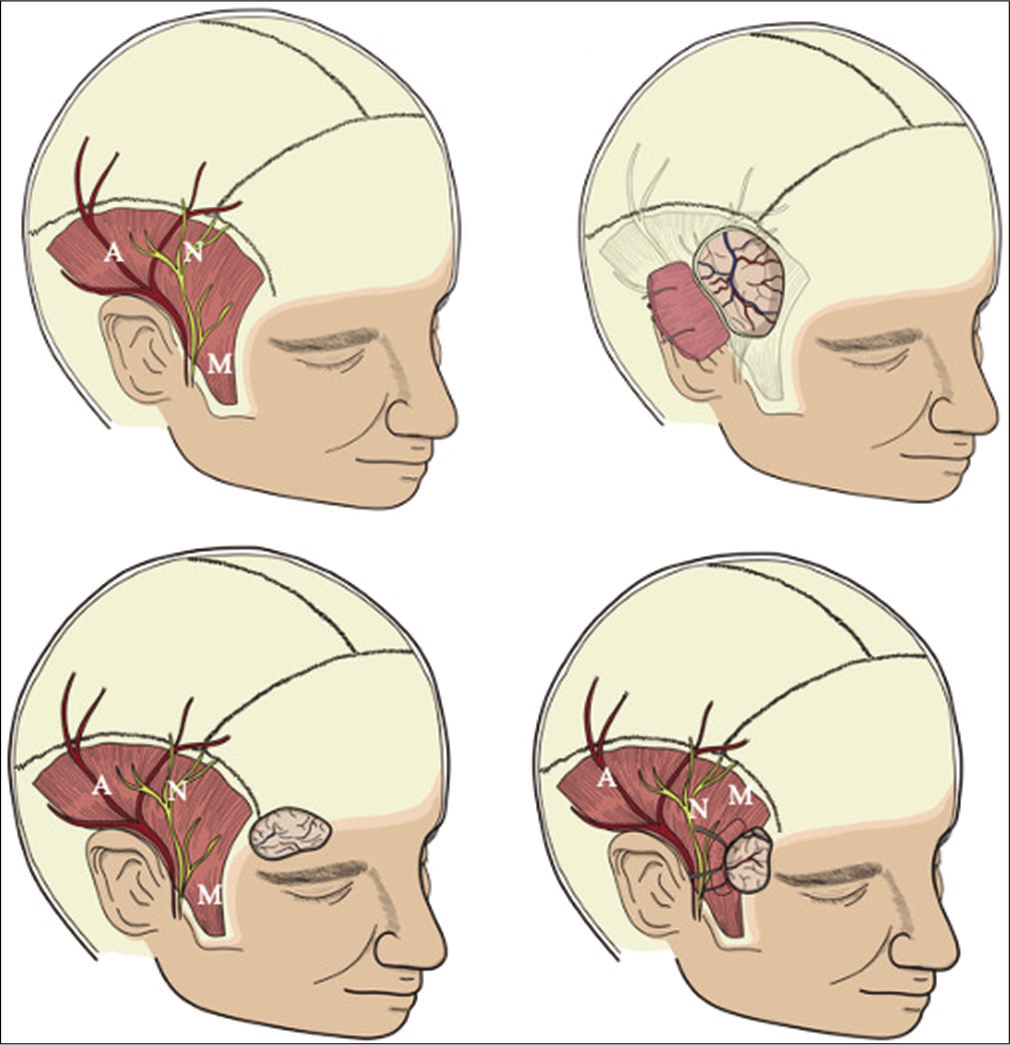
Figure 3:
Schematic representation of the minimally invasive approaches compared with standard pterional craniotomy. A – Superficial Temporal Artery; N – Frontal Branch of Facial Nerve; M – Superficial Temporal Muscle. (a) Preoperative illustration of the main affected structures potentially damaged in surgery. (b) Schematic illustration of the standard pterional craniotomy and structures potentially damaged in surgery. (c) Schematic illustration of the supraorbital craniotomy. Note that due to the location of the approach, the main complaints are frontal muscle weakness and frontal numbness. (d) Schematic illustration of the minipterional craniotomy and structures potentially damaged in surgery. This technique aims to minimize temporal hollowing and adverse effects related to the superficial temporal artery and the frontal branch of facial nerve.
Moreover, there was no control group. The “myocutaneous flap,” the “osteoplastic craniotomy” and the “osteomyoplastic craniotomy” are similar techniques that preserve the temporal muscle attached to the bone flap. There was just one randomized control trial and 2 observational studies showing significant differences regarding TMA compared to the conventional PC. However, the operative time may be a drawback of these techniques, which was just explored in one study and favored the conventional PC.[
With the increasing concept of minimally invasive surgeries, techniques such as mini PC, supraorbital, and frontolateral approaches emerged. It seems logical to think that no or less temporal muscle handling, lesser would be the temporal hollowing. The MPC seems to be an excellent option for unruptured anterior circulation aneurysms,[
Temporomandibular dysfunction (TMD)
TMD is one the most described adverse aesthetic event among the studies. However, no adequate quantification of the event was made by the authors. Costa et al.[
Skin incision
Other incisions, such as those to perform the modified miniorbitomy or the pterional keyhole approach, generate concerns since the incision is out of the hairline. However, the patients submitted to the later were overall satisfied with the final esthetic result. As the patients submitted to the miniorbitomy had orbital meningiomas, the central concern was exophthalmos. This study did not evaluate scars.[
Patient-reported outcomes (PRO)
PRO are highly relevant. This tool is a regularly used indicator for measuring health care quality.[
Among the 38 articles gathered in this study, 27 (71.05%) were retrospective cohorts, with low evidence levels. Only 5 (13.15%) clinical trials met the criteria with a JADAD score of 1 in 2 studies. The remaining three clinical trials had the JADAD score of 0.4 (10.52%) prospective cohorts were included in the study. These articles had a poor description of the methods used to assess cosmetic outcomes, jeopardizing our analysis. More studies should be performed to properly evaluate PRO and the impacts of the different types of craniotomy in patients’ overall satisfaction.
An important limitation observed in practically all studies is that the analysis of aesthetic aspects in the postoperative period of brain surgery is superficial. This results mainly from the severity of the diseases treated, presenting life-threatening, and risk to functional neurological sequelae. However, components that involve the patient’s quality of life have progressively gained relevance more recently. The use of non-surgical treatments with radiosurgery and embolization of aneurysms requires an improvement in PC techniques.[
CONCLUSION
This review showed that the prime esthetic outcomes were TMA, frontal branch weakness, and scar. Several alternative techniques to the PC can be adopted to minimize the drawbacks mentioned above, which appear to be successfully overcome by minimally invasive approaches. The use of one procedure over another must consider the baseline disease, area of exposure, and surgeon expertise. Furthermore, temporozygomatic region primary augmentation with bone or other materials safely prevents temporal hollowing. Finally, an adequate evaluation of the various pterional surgeries is still lacking due to the limited prospective high-quality researches.
Study limitations
This article is not a systematic review; therefore it was not submitted in the PROSPERO database. Furthermore, the studies included did not provide a uniform and systemic method to evaluate the aesthetic outcomes when comparing different approaches. This applies also to a viable quantitative analysis since most articles had no specific quantification of the aesthetic adverse events.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Study limitations
This article is not a systematic review; therefore it was not submitted in the PROSPERO database. Furthermore, the studies included did not provide a uniform and systemic method to evaluate the aesthetic outcomes when comparing different approaches. This applies also to a viable quantitative analysis since most articles had no specific quantification of the aesthetic adverse events.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alkhalili KA, Hannallah JR, Alshyal GH, Nageeb MM, Abdel Aziz KM. The minipterional approach for ruptured and unruptured anterior circulation aneurysms: Our initial experience. Asian J Neurosurg. 2017. 12: 466-74
2. Almeida da Silva S, Yamaki VN, Fontoura Solla DJ, de Andrade AF, Teixeira MJ, Spetzler RF. Pterional, pretemporal, and orbitozygomatic approaches: Anatomic and comparative study. World Neurosurg. 2018. 121: e398-403
3. Al-Otaibi F, Albloushi M, Baeesa S. Minicraniotomy for standard temporal lobectomy: A minimally invasive surgical approach. ISRN Neurol. 2014. 2014: 532523
4. Amirjamshidi A, Abbasioun K, Amiri RS, Ardalan A, Hashemi SM. Lateral orbitotomy approach for removing hyperostosing en plaque sphenoid wing meningiomas. Description of surgical strategy and analysis of findings in a series of 88 patients with long-term follow up. Surg Neurol Int. 2015. 6: 79
5. Ansari SF, Eisenberg A, Rodriguez A, Barkhoudarian G, Kelly DF. The supraorbital eyebrow craniotomy for intra-and extra-axial brain tumors: A single-center series and technique modification. Oper Neurosurg (Hagerstown). 2020. 19: 667-77
6. Chandra PS, Tej M, Sawarkar D, Agarwal M, Doddamani RS. Fronto-orbital variant of supraorbital keyhole approach for clipping ruptured anterior circulation aneurysms (f-sokha). Neurol India. 2020. 68: 1019-27
7. Chen HC, Tzaan WC. Microsurgical supraorbital keyhole approach to the anterior cranial base. J Clin Neurosci. 2010. 17: 1510-4
8. Cheng WY, Lee HT, Sun MH, Shen CC. A pterion keyhole approach for the treatment of anterior circulation aneurysms. Minim Invasive Neurosurg. 2006. 49: 257-62
9. Costa AL, Yasuda CL, França M, de Freitas CF, Tedeschi H, de Oliveira E. Temporomandibular dysfunction post-craniotomy: Evaluation between pre-and post-operative status. J Craniomaxillofac Surg. 2014. 42: 1475-9
10. de Andrade FC, de Andrade FC, de Araujo Filho CM, Filho JC. Dysfunction of the temporalis muscle after pterional craniotomy for intracranial aneurysms. Comparative prospective and randomized study of one flap versus two flaps dieresis. Arq Neuropsiquiatr. 1998. 56: 200-5
11. Eroglu U, Shah K, Bozkurt M, Kahilogullari G, Yakar F, Dogan İ. Supraorbital keyhole approach: Lessons learned from 106 operative cases. World Neurosurg. 2019. S1878-8750: 30060-9
12. Genesan P, Haspani MS, Noor SR. A comparative study between supraorbital keyhole and pterional approaches on anterior circulation aneurysms. Malays J Med Sci. 2018. 25: 59-67
13. Goh DH, Kim GJ, Park J. Medpor craniotomy gap wedge designed to fill small bone defects along cranial bone flap. J Korean Neurosurg Soc. 2009. 46: 195-8
14. Gonzalez LF, Crawford NR, Horgan MA, Deshmukh P, Zabramski JM, Spetzler RF. Working area and angle of attack in three cranial base approaches: Pterional, orbitozygomatic, and maxillary extension of the orbitozygomatic approach. Neurosurgery. 2002. 50: 550-5
15. González-Darder JM, Quilis-Quesada V, Botella-Maciá L. Abordaje pterional transcigomático Parte 2 Experiencia quirúrgica en la patología de base de cráneo [Transzygomatic pterional approach. Part 2: Surgical experience in the management of skull base pathology]. Neurocirugia (Astur). 2012. 23: 96-103
16. Gosal JS, Behari S, Joseph J, Jaiswal AK, Sardhara JC, Iqbal M. Surgical excision of large-to-giant petroclival meningiomas focusing on the middle fossa approaches: The lessons learnt. Neurol India. 2018. 66: 1434-46
17. Grajeda-García FM, Mercado-Caloca F. El colgajo osteomioplástico, una contribución al arte de la neurocirugía [The osteomyoplastic flap, a contribution to neurosurgery]. Rev Med Inst Mex Seguro Soc. 2011. 49: 649-54
18. Hakuba A, Liu S, Nishimura S. The orbitozygomatic infratemporal approach: A new surgical technique. Surg Neurol. 1986. 26: 271-6
19. He H, Li W, Cai M, Luo L, Li M, Ling C. Outcomes after pterional and supraorbital eyebrow approach for cranio-orbital lesions communicated via the supraorbital fissure-a retrospective comparison. World Neurosurg. 2019. 129: e279-85
20. Im SH, Song J, Park SK, Rha EY, Han YM. Cosmetic reconstruction of frontotemporal depression using polyethylene implant after pterional craniotomy. Biomed Res Int. 2018. 2018: 1982726
21. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary?. Control Clin Trials. 1996. 17: 1-12
22. Ji C, Ahn JG. Clinical experience of the brushite calcium phosphate cement for the repair and augmentation of surgically induced cranial defects following the pterional craniotomy. J Korean Neurosurg Soc. 2010. 47: 180-4
23. Kim E, Delashaw JB. Osteoplastic pterional craniotomy revisited. Neurosurgery. 2011. 68: 125-9
24. Kim JH, Lee R, Shin CH, Kim HK, Han YS. Temporal augmentation with calvarial onlay graft during pterional craniotomy for prevention of temporal hollowing. Arch Craniofac Surg. 2018. 19: 94-101
25. Ku D, Koo DH, Bae DS. A prospective randomized control study comparing the effects of dermal staples and intradermal sutures on postoperative scarring after thyroidectomy. J Surg Res. 2020. 256: 413-21
26. La Rocca G, Pepa GM, Sturiale CL, Sabatino G, Auricchio AM, Puca A. Lateral supraorbital versus pterional approach: Analysis of surgical, functional, and patient-oriented outcomes. World Neurosurg. 2018. 119: e192-9
27. Mori K, Osada H, Yamamoto T, Nakao Y, Maeda M. Pterional keyhole approach to middle cerebral artery aneurysms through an outer canthal skin incision. Minim Invasive Neurosurg. 2007. 50: 195-201
28. Mori K, Wada K, Otani N, Tomiyama A, Toyooka T, Takeuchi S. Keyhole strategy aiming at minimizing hospital stay for surgical clipping of unruptured middle cerebral artery aneurysms. J Neurosurg. 2018. 1: 1-8
29. Mori K, Wada K, Otani N, Tomiyama A, Toyooka T, Tomura S. Long-term neurological and radiological results of consecutive 63 unruptured anterior communicating artery aneurysms clipped via lateral supraorbital keyhole minicraniotomy. Oper Neurosurg (Hagerstown). 2018. 14: 95-103
30. Nakamura M, Roser F, Struck M, Vorkapic P, Samii M. Tuberculum sellae meningiomas: Clinical outcome considering different surgical approaches. Neurosurgery. 2006. 59: 1019-28
31. Nassiri F, Price B, Shehab A, Au K, Cusimano MD, Jenkinson MD. life after surgical resection of a meningioma: A prospective cross-sectional study evaluating health-related quality of life. Neuro Oncol. 2019. 21: i32-43
32. Park J, Son W, Kwak Y, Ohk B. Pterional versus superciliary keyhole approach: Direct comparison of approach-related complaints and satisfaction in the same patient. J Neurosurg. 2018. 130: 220-6
33. Reisch R, Marcus HJ, Hugelshofer M, Koechlin NO, Stadie A, Kockro RA. Patients’ cosmetic satisfaction, pain, and functional outcomes after supraorbital craniotomy through an eyebrow incision. J Neurosurg. 2014. 121: 730-4
34. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005. 57: 242-55
35. Romani R, Laakso A, Kangasniemi M, Lehecka M, Hernesniemi J. Lateral supraorbital approach applied to anterior clinoidal meningiomas: Experience with 73 consecutive patients. Neurosurgery. 2011. 68: 1632-47
36. Sarmento SA, Rabelo NN, Figueiredo EG. Minimally invasive technique (nummular craniotomy) for mesial temporal lobe epilepsy: A comparison of 2 approaches. World Neurosurg. 2020. 134: e636-41
37. Schiffman EL, Truelove EL, Ohrbach R, Anderson GC, John MT, List T. The research diagnostic criteria for temporomandibular disorders. I: Overview and methodology for assessment of validity. J Orofac Pain. 2010. 24: 7-24
38. Shapey J, Jung J, Barkas K, Gullan R, Barazi S, Bentley R. A single centre’s experience of managing spheno-orbital meningiomas: Lessons for recurrent tumour surgery. Acta Neurochir (Wien). 2019. 161: 1657-67
39. Steiger HJ, Schmid-Elsaesser R, Stummer W, Uhl E. Transorbital keyhole approach to anterior communicating artery aneurysms. Neurosurgery. 2001. 48: 347-52
40. Sturiale CL, La Rocca G, Puca A, Fernandez E, Visocchi M, Marchese E. Minipterional craniotomy for treatment of unruptured middle cerebral artery aneurysms. A single-center comparative analysis with standard pterional approach as regard to safety and efficacy of aneurysm clipping and the advantages of reconstruction. Acta Neurochir Suppl. 2017. 124: 93-100
41. Tang C, Sun J, Xue H, Yu Y, Xu F. Supraorbital keyhole approach for anterior circulation aneurysms. Turk Neurosurg. 2013. 23: 434-8
42. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018. 169: 467-73
43. Welling LC, Figueiredo EG, Wen HT, Gomes MQ, Bor-SengShu E, Casarolli C, Guirado VM. Prospective randomized study comparing clinical, functional, and aesthetic results of minipterional and classic pterional craniotomies. J Neurosurg. 2015. 122: 1012-9
44. Wiedemayer H, Sandalcioglu IE, Wiedemayer H, Stolke D. The supraorbital keyhole approach via an eyebrow incision for resection of tumors around the sella and the anterior skull base. Minim Invasive Neurosurg. 2004. 47: 221-5
45. Yang J, Oh CW, Kwon OK, Hwang G, Kim T, Moon JU. The usefulness of the frontolateral approach as a minimally invasive corridor for clipping of anterior circulation aneurysm. J Cerebrovasc Endovasc Neurosurg. 2014. 16: 235-40
46. Yasargil MG, Antic J, Laciga R, Jain KK, Hodosh RM, Smith RD. Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg Neurol. 1976. 6: 83-91
47. Youssef AS, Ahmadian A, Ramos E, Vale F, van Loveren HR. Combined subgaleal/myocutaneous technique for temporalis muscle dissection. J Neurol Surg B Skull Base. 2012. 73: 387-93
48. Youssef AS, Willard L, Downes A, Olivera R, Hall K, Agazzi S. The frontotemporal-orbitozygomatic approach: Reconstructive technique and outcome. Acta Neurochir (Wien). 2012. 154: 1275-83
49. Yu LB, Huang Z, Ren ZG, Shao JS, Zhang Y, Wang R. Supraorbital keyhole versus pterional craniotomies for ruptured anterior communicating artery aneurysms: A propensity score-matched analysis. Neurosurg Rev. 2018. 43: 547-54