- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq
- Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq
- Department of Neurosurgery, University of Al-Nahrain, College of Medicine, Baghdad, Iraq
- Department of Neurosurgery, University of Alameed, College of Medicine, Karbala, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
DOI:10.25259/SNI_948_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hayder R. Salih1, Huda Jaafer2, Mustafa Ismail2, Ali Kareem Khallaf1, Ali Jassim Mohammed1, Mohammad Sadeq M. J. Al-Mosawy3, Hawraa Sadiq Naser4, Ziyad Talal Maulood1, Anwar N. Hafedh1, Samer S. Hoz5. Extensive tension pneumocephalus presented in the setting of a challenging etiology. 09-Dec-2022;13:570
How to cite this URL: Hayder R. Salih1, Huda Jaafer2, Mustafa Ismail2, Ali Kareem Khallaf1, Ali Jassim Mohammed1, Mohammad Sadeq M. J. Al-Mosawy3, Hawraa Sadiq Naser4, Ziyad Talal Maulood1, Anwar N. Hafedh1, Samer S. Hoz5. Extensive tension pneumocephalus presented in the setting of a challenging etiology. 09-Dec-2022;13:570. Available from: https://surgicalneurologyint.com/surgicalint-articles/12056/
Abstract
Background: Pneumocephalus (PNC) is a well-described consequence in postoperative settings and skull fractures that is usually self-limiting. It can get complicated into tension PNC on some rare occasions, leading to an intracranial mass effect. PNC was also reported after unintentional dural puncture throughout the epidural anesthesia process. However, tension PNC resulting from epidural anesthesia procedures is an extremely rare outcome that implies urgent intervention to relieve the tension within the brain. Here, we report a case of an extensive tension intraventricular PNC 2 days following an epidural anesthesia procedure for a femur fixation surgery.
Case Description: A 23-year-old male presented to the emergency department with basal skull fractures and a femur fracture due to a motorcycle accident. His skull base fracture was managed conservatively then he underwent a femur fixation procedure under epidural anesthesia. Two days after, he developed a severe headache with a disturbed level of consciousness. Computed tomography of the brain revealed an extensive PNC that involved all the subarachnoid spaces down to the cervical region and compressing the cerebellum, which was not found in the initial imaging. The patient’s status improved after the twist-drill burr-hole evacuation of air under the water seal.
Conclusion: Extensive tension PNC can occur after traumatic brain injury, especially after epidural anesthesia. Such cases should gain high focus because they may differ from simple PNC regarding diagnosis, treatment, and follow-up.
Keywords: Epidural anesthesia, Intraventricular aerocele, Pneumocephalus, Traumatic brain injury, Tension pneumocephalus
INTRODUCTION
Pneumocephalus (PNC) is defined as the asymptomatic existence of air inside the cranium, including any of the epidural, subdural, subarachnoid, intracerebral, or intraventricular compartments.[
Here, we report a case of an extensive tension intraventricular PNC 2 days following an epidural anesthesia procedure for a femur fixation surgery.
CASE DESCRIPTION
A 23-year-old male presented to the emergency department after encountering a motor vehicle accident that resulted in a skull base fracture and fracture in the right femur. The patient received conservative care at the neurosurgical unit and was discharged in good condition. Afterward, the patient was referred to the orthopedic unit, where he underwent a femur fixation procedure using epidural anesthesia. The procedure was completed without any remarkable events.
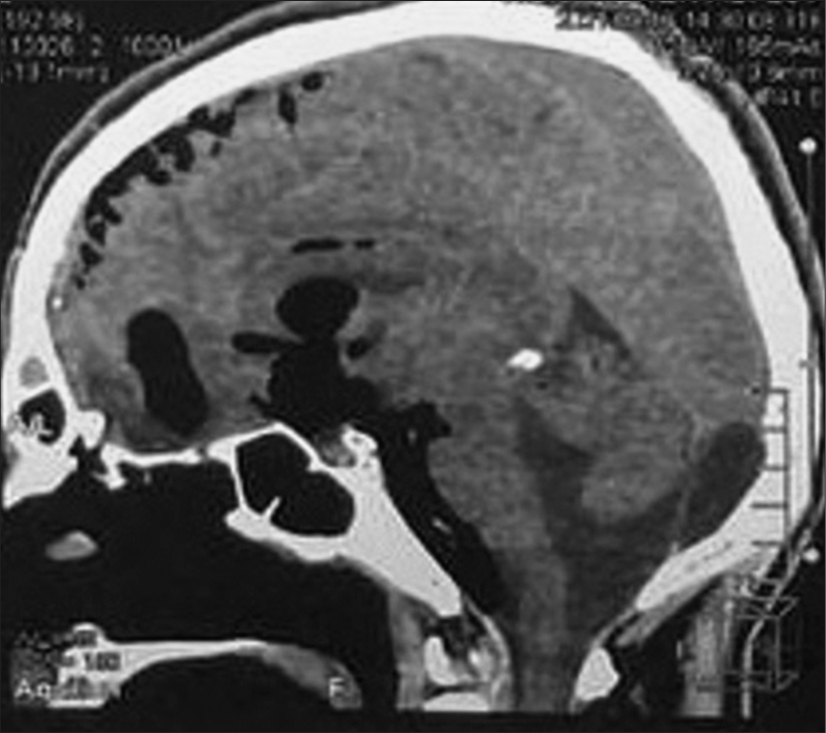
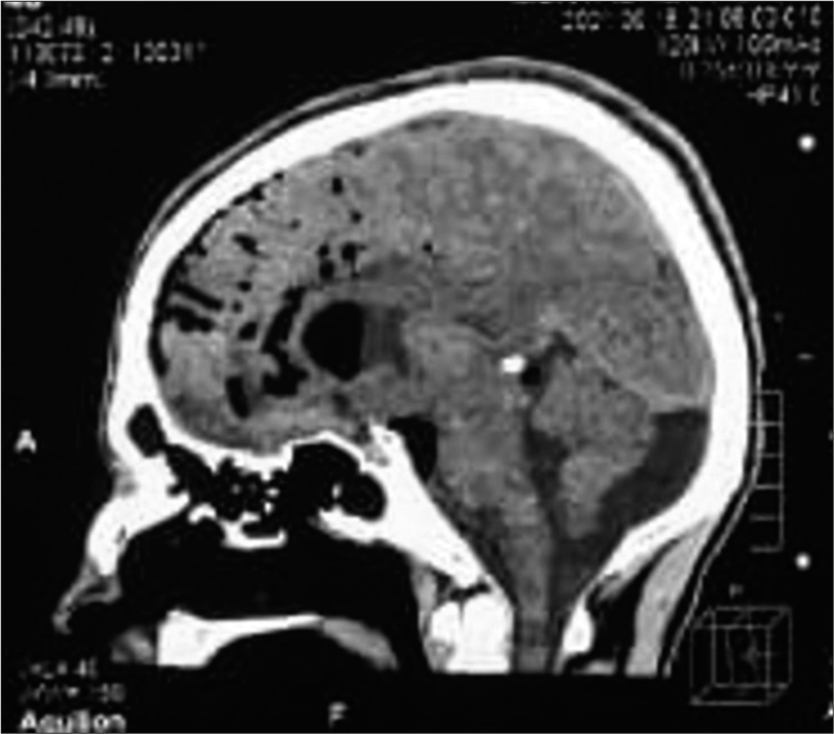
Two days after, the patient developed a severe headache and disturbed level of consciousness; Glasgow Coma Scale (GCS) scored 11/15 (E3, V4, M4), with vomiting and irritability. Computed tomography (CT) of the cranium revealed a huge intracranial aerocele, including lateral, third, and fourth ventricles extending to the cervical subarachnoid spaces [
The patient’s symptoms improved eventually as the follow-up CT scans confirmed the gradual resolution of the PNC, and the headache was relieved, while GCS scored 15.
DISCUSSION
The most frequent cause of PNC is trauma, mainly basal skull fractures. Other causes include tumors, infections such as meningitis and abscess, CSF fistula, nitrous oxide anesthesia, and open brain surgeries. Meanwhile, the causes of PNC originating from the spine include trauma, tumor, and spine infection, and rarely, spinal surgeries and dural tears induced by spinal operations such as lumbar puncture and epidural injections are among the causes.[
Epidural anesthesia is generally considered a safe and easy-to-perform procedure with a low prevalence of complications. The method is similar to a lumbar puncture, except that the needle is fixed before the dura is punctured.[
Possible complications of the LORA technique are dural puncture which could be with or without postdural puncture headache, PNC, spinal cord and nerve root compression, subcutaneous emphysema, and air embolism.[
There were multiple cases in the literature reporting PNC after epidural procedures in different parts of the brain, including the ventricles.[
Two theories describe air’s pathophysiology within the skull.[
We assume that our case falls within the second theory. The ball valve mechanism was noted during the LORA procedure since neither CSF leakage nor CSF flashback. A previous paper suggested that in the absence of visible evidence of dural taps, such as no CSF flashback, the air enters the head either through an unidentified dural puncture or a dural defect in the lumbar area and subsequent arachnoid tear.[
In summary, this case report describes a rare yet severe complication of PNC, possibly due to epidural anesthesia or a basal skull fracture. An immediate procedure was done to evacuate the air from the brain since it had a compressive effect on the cerebellum and caused neurological deterioration. Cases of tension PNC in the literature are scarce; only a few have been reported after epidural anesthesia, and fewer were of this extensive size.
CONCLUSION
Extensive tension PNC can occur after traumatic brain injury, particularly after epidural anesthesia. These cases should gain high focus because they may have different management strategies from simple PNC cases.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aida S, Taga K, Yamakura T, Endoh H, Shimoji K. Headache after attempted epidural block: The role of intrathecal air. Anesthesiology. 1998. 88: 76-81
2. Almubarak AO, Fakhroo F, Alhuthayl MR, Kanaan I, Aldahash H. Tension pneumoventricle secondary to cutaneous-ventricular fistula: Case report and literature review. World Neurosurg. 2020. 142: 155-8
3. Armocida D, Pesce A, Frati A, Miscusi M, Paglia F, Raco A. Pneumoventricle of unknown origin: A personal experience and literature review of a clinical enigma. World Neurosurg. 2019. 122: 661-4
4. Cowan CM, Moore EW. A survey of epidural technique and accidental dural puncture rates among obstetric anaesthetists. Int J Obstet Anesth. 2001. 10: 11-6
5. Dabdoub CB, Salas G, Silveira ED, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int. 2015. 6: 155
6. Dahlgren N, Törnebrandt K. Neurological complications after anaesthesia. A follow-up of 18,000 spinal and epidural anaesthetics performed over three years. Acta Anaesthesiol Scand. 1995. 39: 872-80
7. Figueira H, Guimaraes J, Sousa AL, Regalado AM. Pneumocephalus following unidentified dural puncture: A case report with an unusual neurological presentation. Pain Physician. 2017. 20: E329-34
8. Gonçalves MB, Nunes CF, Melo JO, Guimarães RD, Klescoski J, Landeiro JA. Tension pneumoventricle after resection of a fourth ventricle choroid plexus papilloma: An unusual postoperative complication. Surg Neurol Int. 2012. 3: 116
9. Gorissen Z, Hakvoort K, van den Boogaart M, Klinkenberg S, Schijns O. Pneumocephalus: A rare and life-threatening, but reversible, complication after penetrating lumbar injury. Acta Neurochir (Wien). 2019. 161: 361-5
10. Hsieh XX, Hsieh SW, Lu CH, Wu ZF, Ju DT, Huh B. A rare case of pneumocephalus and pneumorrhachis after epidural anesthesia. Acta Anaesthesiol Taiwan. 2015. 53: 47-9
11. Krishnan SS, Manuel A, Vasudevan MC. Delayed pneumoventricle following endonasal cerebrospinal fluid rhinorrhea repair with thecoperitoneal shunt. Asian J Neurosurg. 2019. 14: 325-8
12. Lee SH, Koh JS, Bang JS, Kim MC. Extensive tension pneumocephalus caused by spinal tapping in a patient with basal skull fracture and pneumothorax. J Korean Neurosurg Soc. 2009. 45: 318-21
13. Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien). 1967. 16: 1-78
14. McMurtrie R, Jan R. Subarachnoid pneumocephalus: A rare complication of epidural catheter placement. J Clin Anesth. 2002. 14: 539-42
15. Nafiu OO, Urquhart JC. Pneumocephalus with headache complicating labour epidural analgesia: Should we still be using air?. Int J Obstet Anesth. 2006. 15: 237-9
16. Tsai JC, Cheng KY, Tsai ST, Tsai MJ. Tension pneumoventricle and cerebrospinal fluid rhinorrhea. QJM. 2017. 110: 39-40
17. Tuğcu B, Tanriverdi O, Günaldi Ö, Baydin S, Postalci LŞ Akdemir H. Delayed intraventricular tension pneumocephalus due to scalp-ventricle fistula: A very rare complication of shunt surgery. Turk Neurosurg. 2009. 19: 276-80
18. Wantman A, Hancox N, Howell PR. Techniques for identifying the epidural space: A survey of practice amongst anaesthetists in the UK. Anaesthesia. 2006. 61: 370-5
19. Young M, Putty M, Schaible K. Spontaneous intraventricular tension pneumocephalus: Case report and review of the literature. World Neurosurg. 2018. 114: 317-22
20. Yun JH, Kim YJ, Yoo DS, Ko JH. Diffuse pneumocephalus: A rare complication of spinal surgery. J Korean Neurosurg Soc. 2010. 48: 288-90