- Departments of Neurosurgery, University of Louisville, Louisville, Kentucky, Iraq
- Departments of Neurosurgery Teaching Hospital, Baghdad, Iraq.
Correspondence Address:
Zaid Aljuboori
Departments of Neurosurgery, University of Louisville, Louisville, Kentucky, Iraq
DOI:10.25259/SNI_49_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zaid Aljuboori, Samer Hoz, Maxwell Boakye. Failure of C2-3 anterior arthrodesis for the treatment of atypical Hangman’s fractures: A three case series. 21-Mar-2020;11:52
How to cite this URL: Zaid Aljuboori, Samer Hoz, Maxwell Boakye. Failure of C2-3 anterior arthrodesis for the treatment of atypical Hangman’s fractures: A three case series. 21-Mar-2020;11:52. Available from: https://surgicalneurologyint.com/surgicalint-articles/9917/
Abstract
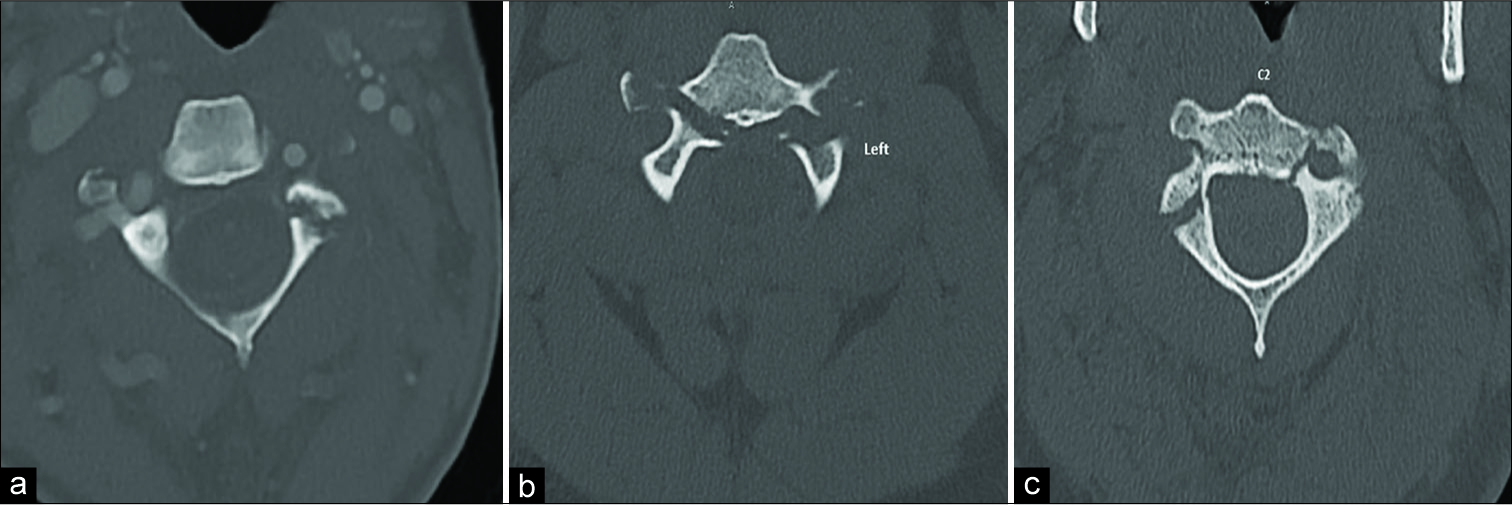
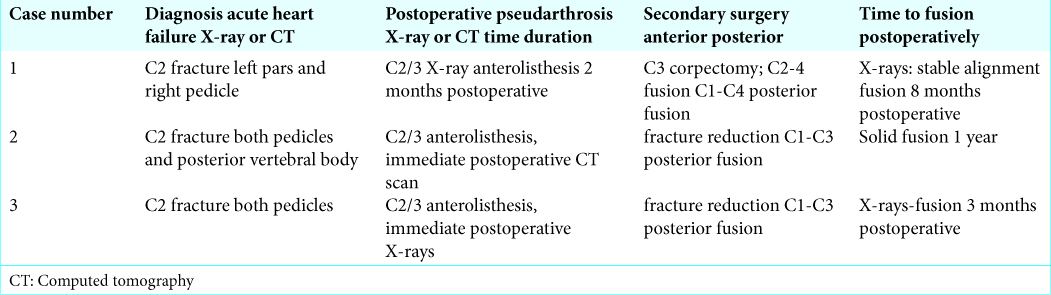
Background: Hangman’s fractures (HF) are defined by bilateral fractures of pars interarticularis of the axis. Most can be treated with a collar. However, the treatment strategies for atypical HF (AHF) involve the pedicles, are unstable, and require fusion. Here, we present three cases of AHF that failed anterior arthrodesis warranting repeat anterior (one case), and posterior fusions (three cases).
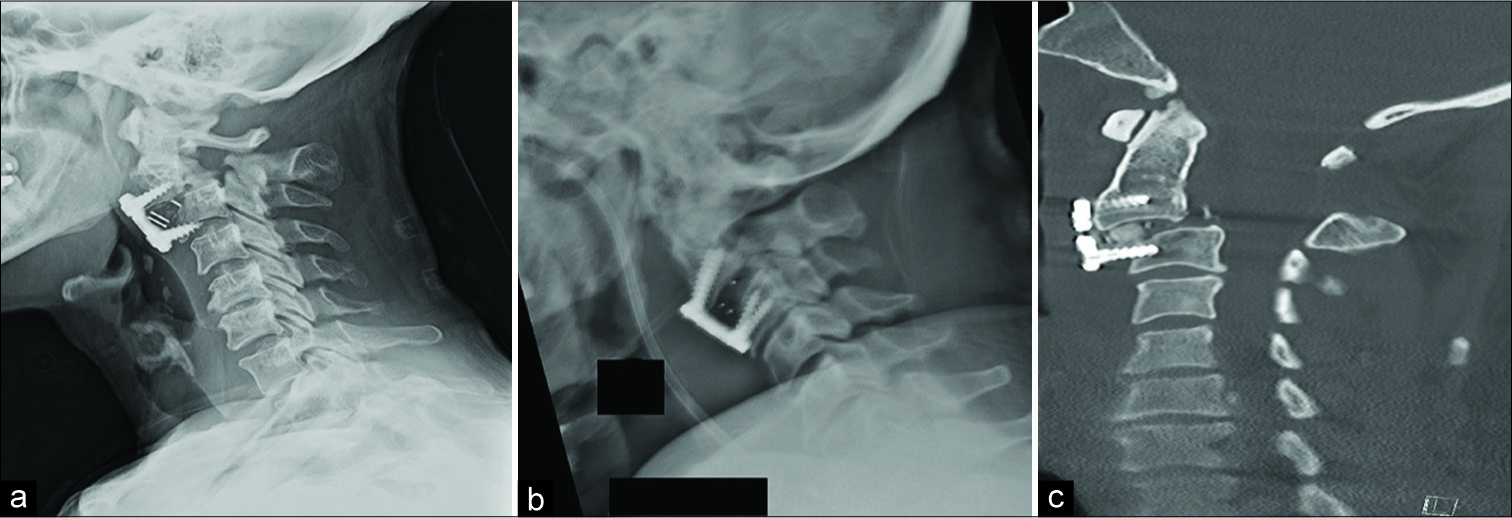
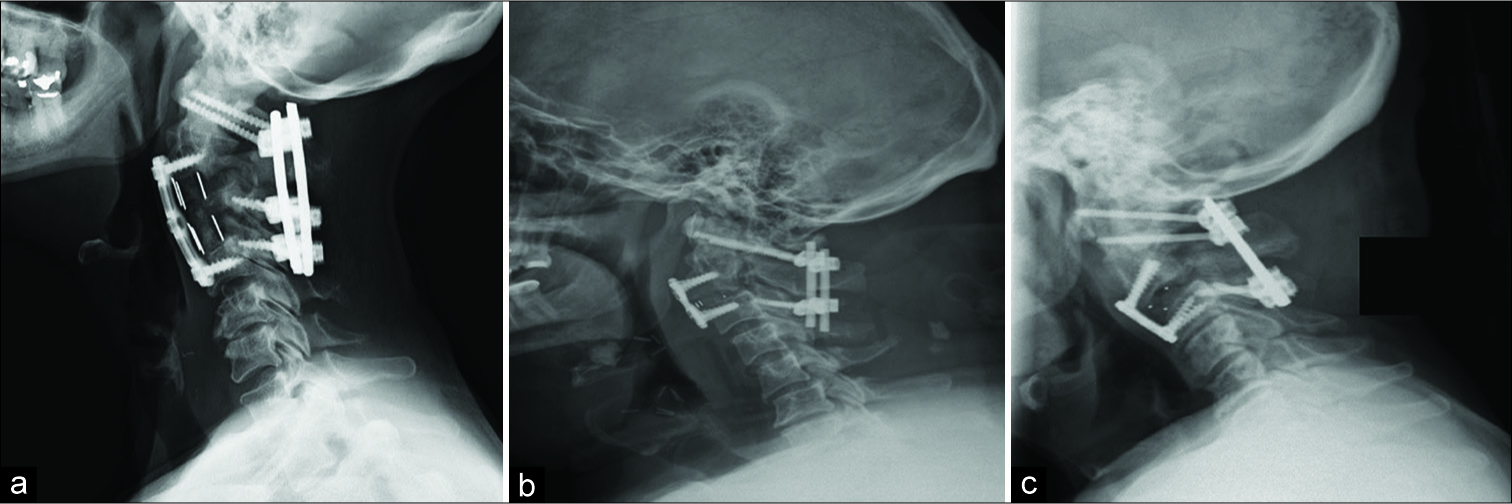
Case Description: One female and two males, ranging from 48 to 69 years of age, presented with AHF. All three were originally treated with C2-3 anterior cervical discectomy/fusion, and all three failed (e.g., resulted in pseudarthrosis/ anterolisthesis/instability). The first patient required a secondary C3 corpectomy/C2-4 arthrodesis, with C1-C4 posterior instrumentation. The latter two patients required secondary C1-C3 posterior fusions. For all three patients, 3–12 months follow-up X-rays confirmed the excellent alignment of the instrumentation and bony fusion.
Conclusion: Anterior arthrodesis can be utilized to treat AHF, but often fail when addressing AHF. All AHF warranted secondary posterior fusions (e.g., C1-C3 two cases; and C1-C4 one case) and a subset may additionally require more extensive anterior fusions (e.g., C2-C4 with corpectomy of C3).
Keywords: Anterolisthesis, Arthrodesis, Atypical, Hangman’s fracture, Instrumentation, Spine, Trauma
INTRODUCTION
Traumatic spondylolisthesis of the axis hangman’s fractures (HF) involves fracture of the pars interarticularis bilaterally. These are the second most common type of axis fractures.[
Most patients with typical HF are neurologically intact; only 6.5% present with neurological injury.[
CASE PRESENTATIONS
Three patients presented with AHF; these included one female and two males, ranging in age from 48 to 69 years of age[
DISCUSSION
Here, we analyzed three cases of AHF that failed following C2-C3 ACDF variously all attributed to: (1) involvement of the C2 pedicle/posterior vertebral body (one case), and disc disruption (two cases). All patients were treated with C2-3 ACDF shortly after injury and received rigid cervical orthoses.
Failure recognition
The failure of the anterior arthrodesis was evident in the initial postoperative imaging in two cases and on the 2 months follow-up exam for the third patient [
Literature review
Al-Mahfoudh et al. reported a study of 41 patients with HF; 68.2% were atypical.[
CONCLUSION
Anterior arthrodesis offers a >90% fusion rate for typical HF, but not for AHF. We suggest that AHF, especially with pedicle(s) involvement, be treated occasionally with anterior reoperations (e.g., if needed due to instrumentation displacement), but uniformly with secondary posterior stabilization.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Mahfoudh R, Beagrie C, Woolley E, Zakaria R, Radon M, Clark S. Management of typical and atypical hangman’s fractures. Global Spine J. 2016. 6: 248-56
2. Hakało J, Wroński J. Operative treatment of hangman’s fractures of C2. Posterior direct pars screw repair or anterior plate-cage stabilization? Neurol Neurochir Pol. 2008. 42: 28-36
3. Han K, Cui SB, Wang L, Wei FX, Liu SY. Traumatic bilateral atlantoaxial rotatory subluxation with hangman fracture in an adult. Neurol India. 2016. 64: 811-4
4. Karthigeyan M, Rangan V, Salunke P. A case of traumatic C2-3 listhesis without pars fracture: Insights from this possible variant of hangman’s fracture. Neurol India. 2017. 65: 209-11
5. Li G, Zhong D, Wang Q. A novel classification for atypical hangman fractures and its application: A retrospective observational study. Medicine (Baltimore). 2017. 96: e7492-
6. Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of hangman’s fractures. Eur Spine J. 2006. 15: 257-69
7. Murphy H, Schroeder GD, Shi WJ, Kepler CK, Kurd MF, Fleischman AN. Management of hangman’s fractures: A systematic review. J Orthop Trauma. 2017. 31: S90-5
8. Salunke P, Karthigeyan M, Sahoo SK, Prasad PK. Multiplanar realignment for unstable hangman’s fracture with posterior C2-3 fusion: A prospective series. Clin Neurol Neurosurg. 2018. 169: 133-8