- Department of Anaesthesia and Intensive Care, , Postgraduate Institute of Medical Education and Research, Chandigarh, India.
- Department of Neurosurgery, , Postgraduate Institute of Medical Education and Research, Chandigarh, India.
- Department of Radiology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Correspondence Address:
Hemant Bhagat
Department of Anaesthesia and Intensive Care, , Postgraduate Institute of Medical Education and Research, Chandigarh, India.
DOI:10.25259/SNI_522_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sanket Agrawal1, Pravin Salunke2, Shailesh Gupta1, Amlan Swain1, Kiran Jangra1, Nidhi Panda1, Seelora Sahu1, Vivek Gupta3, Summit Bloria1, Ketan Karsandas Kataria1, Hemant Bhagat1. Fiberoptic bronchoscopy versus video laryngoscopy guided intubation in patients with craniovertebral junction instability: A cinefluroscopic comparison. 08-Mar-2021;12:92
How to cite this URL: Sanket Agrawal1, Pravin Salunke2, Shailesh Gupta1, Amlan Swain1, Kiran Jangra1, Nidhi Panda1, Seelora Sahu1, Vivek Gupta3, Summit Bloria1, Ketan Karsandas Kataria1, Hemant Bhagat1. Fiberoptic bronchoscopy versus video laryngoscopy guided intubation in patients with craniovertebral junction instability: A cinefluroscopic comparison. 08-Mar-2021;12:92. Available from: https://surgicalneurologyint.com/surgicalint-articles/10631/
Abstract
Background: Manipulation during endotracheal intubation in patients with craniovertebral junction (CVJ) anomalies may cause neurological deterioration due to underlying instability. Fiberoptic-bronchoscopy (FOB) is better than video laryngoscope (VL) for minimizing cervical spine movement during intubation. However, evidence suggesting superiority of FOB in patients with CVJ instability is lacking. We prospectively compared dynamic movements of the upper cervical spine during intubation using FOB with VL in patients with CVJ anomalies.
Methods: A prospective, randomized, and clinical trial was conducted in 62 patients of American Society of Anaesthesiologist Grade I-II aged between 12 and 65 years with CVJ anomalies. Patients were randomized for intubation under general anesthesia with either VL or FOB. The intubation process was done with application of skeletal traction and recorded cinefluroscopically. The dynamic interrelationship of bony landmarks (horizontal, vertical, and diagonal distances between fixed points on posterior C1 and C2) was analyzed to indirectly calculate alteration of the upper cervical spinal canal diameter (at CVJ). Atlanto-dental interval (ADI) was calculated wherever possible.
Results: The alteration in canal diameter (using bony landmarks) at CVJ during intubation was not significant with the use of either VL or FOB (P > 0.05). In 41 patients, where ADI could be measured, ADI was reduced (increased spinal canal diameter) in a greater number of patients in VL group when compared to FOB group (P
Conclusion: Using rigid skull traction, intubation under general anesthesia with VL offers similar advantage as FOB in terms of the spinal kinematics in patients with CVJ anomalies/instability. Nevertheless, greater number of patients intubated with VL may have an advantage of increased cervical spinal canal diameter when compared to FOB.
Keywords: Atlanto-axial dislocation, Cervical spine movement, Craniovertebral junction, Fiberoptic bronchoscopy, Video laryngoscopy
INTRODUCTION
Endotracheal intubation is associated with significant movement of cervical spine.[
The objective of our prospective randomized clinical study was to record and to analyze the dynamic interrelationship of bony landmarks of the upper cervical spine at CVJ (using novel indices) during intubation with FOB and compare it with intubation with VL in patients with CVJ instability on rigid skull traction. Comparison of the groups for difference in the horizontal distance between two bony landmarks was the primary outcome measure of the study. The differences in the change of vertical distance, diagonal distance, and ADI between the groups were the secondary outcomes of the study.
MATERIALS AND METHODS
The study is a prospective randomized control trial conducted from January 2017 to June 2018. After obtaining approval from the institution ethics committee, the trial was registered with the Clinical Trial Registry of India (CTRI/2017/08/009433). Written informed consent was obtained from all the participants. The patients aged 12–65 years of either gender belonging to American Society of Anaesthesiologist Physical Status (ASA PS) 1 and 2 were enrolled in the study. The patients who were scheduled for posterior C1-C2 reduction and fusion for CVJ anomalies AAD under general anesthesia were included in the study. Patients with anticipated difficult intubation, need for emergency intubation, patients at increased risk of pulmonary aspiration and those requiring more than three attempts for intubation were excluded from the study. A computer-generated random number table achieved group allocation of patients to either one of the intubation modalities. Before induction of anesthesia, a sealed opaque envelope containing a computer-generated random assignment was opened, assigning patients to either Macintosh VL (VBM, India) or FOB (Pentax, Japan) guided intubation.
Anesthesia protocol
The patient’s epidemiological and anthropometric data were recorded. As an institutional protocol, the rigid skull traction was applied 1 day before surgery under local anesthesia. On the day of the surgery, the patient was placed on a radiolucent, rigid table with skull traction equivalent to one seventh of the body weight using Crutchfield tongs in neutral position. All patients were subjected to Standard ASA monitoring protocols. The intubation was carried out in both the groups under general anesthesia. Anesthesia was induced with intravenous fentanyl 2 mcg/kg, propofol 2 mg/kg, vecuronium 0.1 mg/kg, and maintained with propofol 100–200 mcg/kg till the completion of intubation sequence.
Intubation protocol
After induction of anesthesia and achievement of adequate neuromuscular blockade (TOF count 0), sleep FOB was conducted in patients randomized to the FOB group. We used a bite block in all the cases of FOB group so as to facilitate the introduction of FOB. Ancillary measures to open the airway such as jaw thrust was used in a case to case basis to facilitate adequate visualization of the vocal cords and a record of use of jaw thrust was maintained. The FOB was advanced through the vocal cords till carina and subsequently an appropriately sized PVC endotracheal tube were placed at the correct position. In patients randomized to VL group, laryngoscopy was performed till vocal cords were visualized and an appropriate sized PVC endotracheal tube was placed in the trachea.
Fluoroscopy was performed from the time of insertion of VL as well as FOB until its removal, taking care to exert minimal force necessary to achieve intubation. All intubations were performed by anesthesiologists (SA and HB) proficient in the use of both the devices (more than 50 intubations with each device). Three attempts were permitted for each technique. An attempt was aborted when the patient desaturated below 92%. In between two attempts, the patient’s lungs were ventilated. The frames which recorded the greatest range of motion were used for final analysis.
Cinefluoroscopy protocol
Cinefluoroscopy was performed with the c-spine in the neutral position, the occiput and shoulders resting directly on the firm horizontal surface of the table. The head was kept in the anatomical position with the skeletal traction. The cinefluoroscopy was adjusted to include the base of the cranium (C0) and the second cervical vertebra (C2) in the lateral view. Once the positioning was deemed appropriate, the table and the fluoroscopy camera were kept static. Radiation protective device was placed from shoulder to knee to protect patient from radiation and only neck portion was exposed to minimize radiation. O-C1-C2 dynamics were recorded with continuous fluoroscopy (Philips, Allura Xper FD20/10; Philips Medical Systems, the Netherland) during laryngoscopy and intubation with either VL or FOB. The patients or their relatives were informed regarding the radiation exposure during surgery. However, they were clearly explained as to the additional radiation they would be exposure to if they chose to participate in the study.
The imaging for intubation was divided into four stages for comparison between the two techniques. The first stage was the “baseline,” a neutral image of the c-spine immediately before the introduction of the intubating device into the oropharynx. The second stage was “introduction,” which included the insertion of the intubating device until the visualization of the glottic aperture in the VL group and the carina in the FOB group. The third stage, “intubation” recorded the endotracheal tube placement in the trachea. The fourth stage, “removal” recorded the withdrawal of the intubating device from the patient.
The previous studies measuring the cervical spine kinetics vis a vis various intubation modality have mostly measured the angles between the cervical vertebra and presented their findings accordingly. In the realm of cervical spine kinetics during intubation, it is pertinent to note that very few studies have been done in patients with diseased cervical spine.
Acquisition and analysis of radiologic data
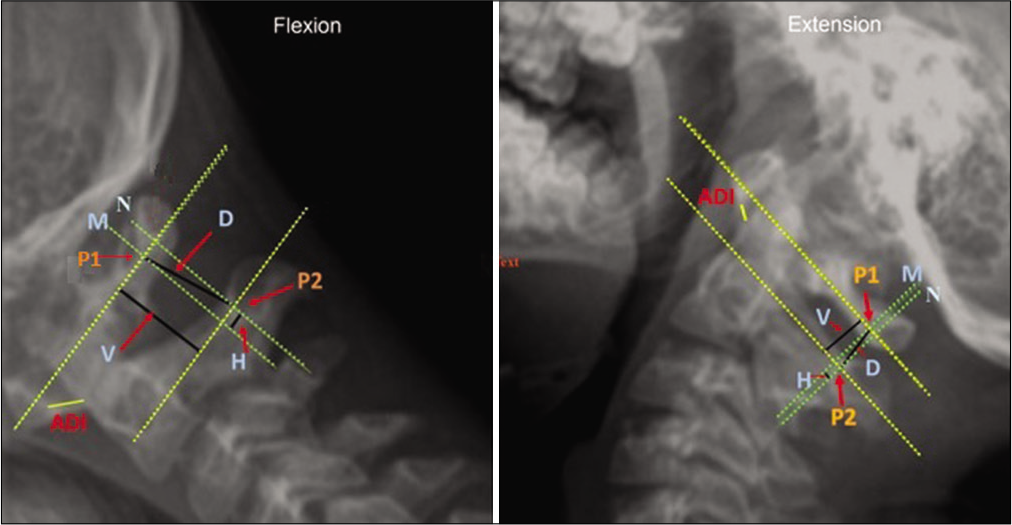
Digital cinefluroscopic recordings of intubation were analyzed offline using software “Horos.” Film for all the stages of intubation was systematically reviewed frame-by-frame and compared with “baseline reference image,” to determine maximum vertical as well as horizontal motion between C1 and C2. The frame capturing maximum cervical spine movement was used for analysis. The determination of the motion between C1 and C2 was impeded by the fact that due to the anomaly in CV junction, the C1 arch and dens were not clearly delineated on fluoroscopy due to its invagination, hence making it nearly impossible to measure ADI. The anatomical landmarks which could be appreciated in all patients were the inferior-posterior point of C1 post arch along spinolaminar junction (P1) and superior-anterior point at C2 spinolaminar junction (P2) [
Figure 1:
Dynamic flexion extension lateral radiograph of cervical spine with calculation of vertical, horizontal, and diagonal distance. P1-infero-posterior point on posterior arch of atlas, P2-supero-anterior point at axis spinolaminar junction. M-A line perpendicular to axial plane along C1 passing through point P1, N – a second-line passing through point P2 parallel to the M (first line).
Statistical analysis
The sample size of our prospective study was based on the pilot study conducted in ten patients. Taking the difference in means of H distance between two groups as 1.09 (1.20 in FOB group and 0.11 in VL group), with a standard deviation of 1.47 and a power of study of 80% and a confidence interval of 95% the sample size estimated was 29 subjects per group. We decided to have 31 subjects per group after accounting for possible attrition. Data analysis was performed with the aid of Statistical Package for the Social Sciences (SPSS) software (version 22, SPSS, Chicago, IL). Continuous data were presented as mean and standard deviation or median and interquartile range. The normality of data was tested with the Kolmogorov–Smirnov tests. For normally distributed data, t-test was carried out for statistical analysis of two groups. Group comparisons of values of skewed data were made with the Mann–Whitney test for two groups (Gender). Categorical variables were reported as counts and percentages. Group comparisons were made with the Chi-square test or Fisher’s exact test. Statistical significance was defined at P < 0.05.
RESULTS
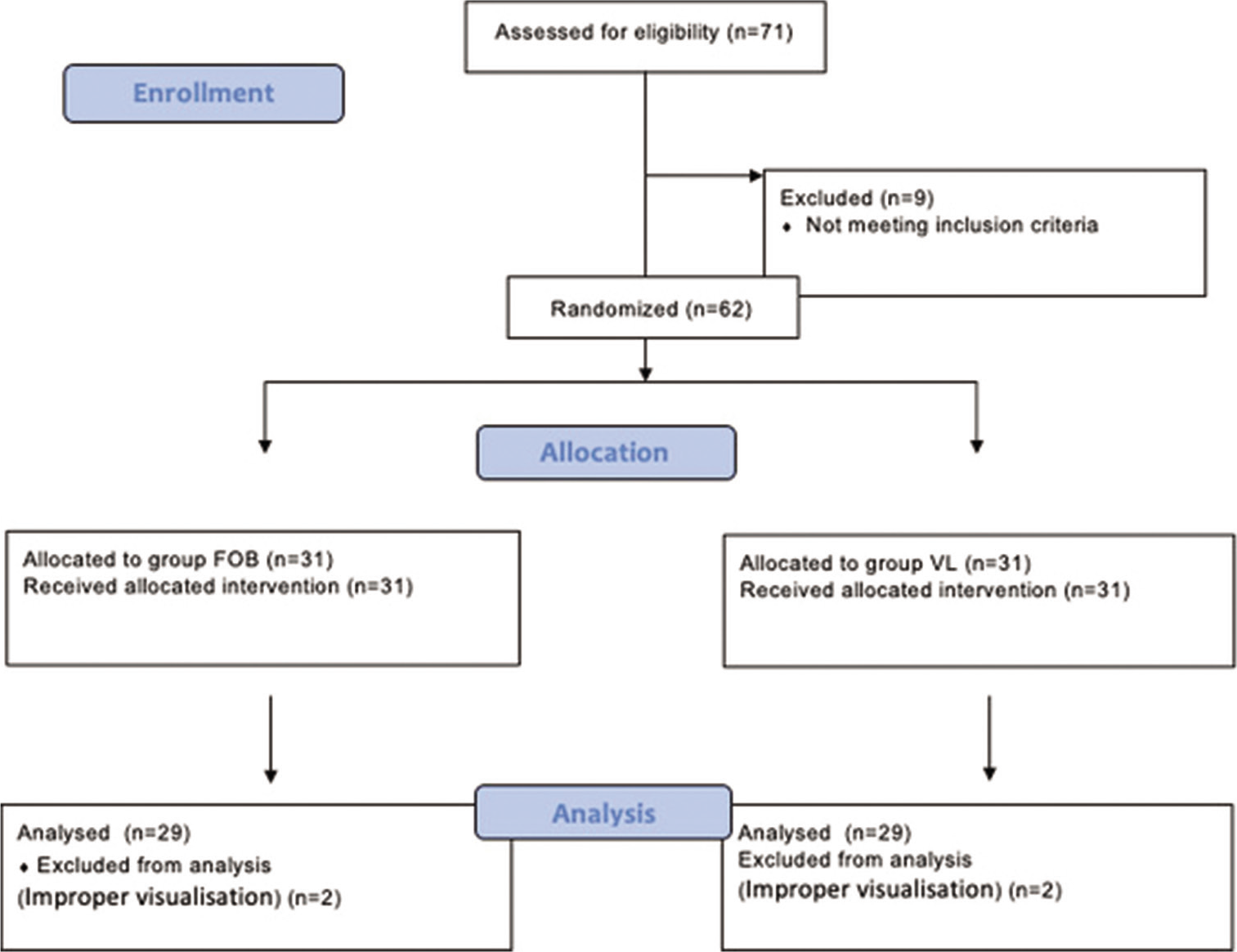
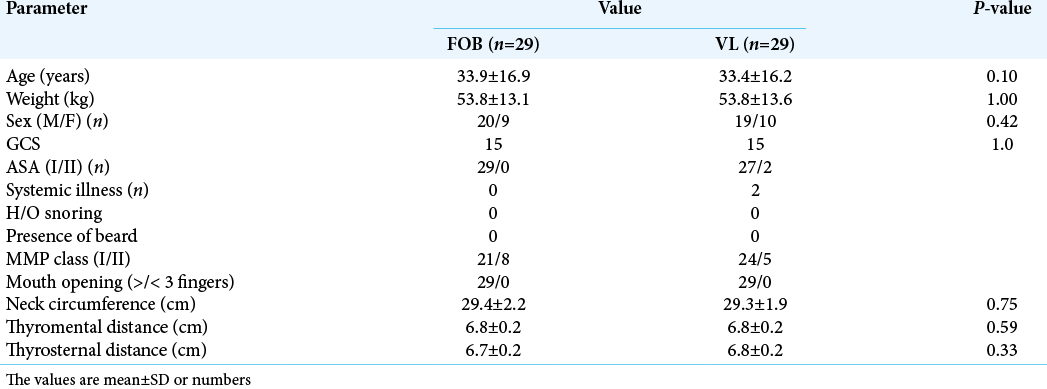
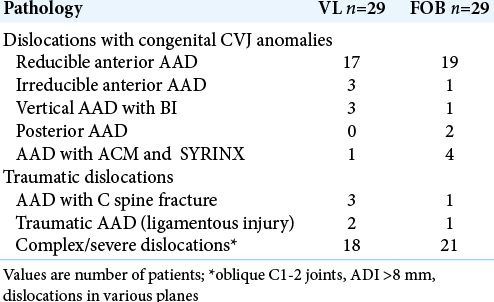
Sixty-two patients were enrolled for the study and the data were analyzed for 58 patients [
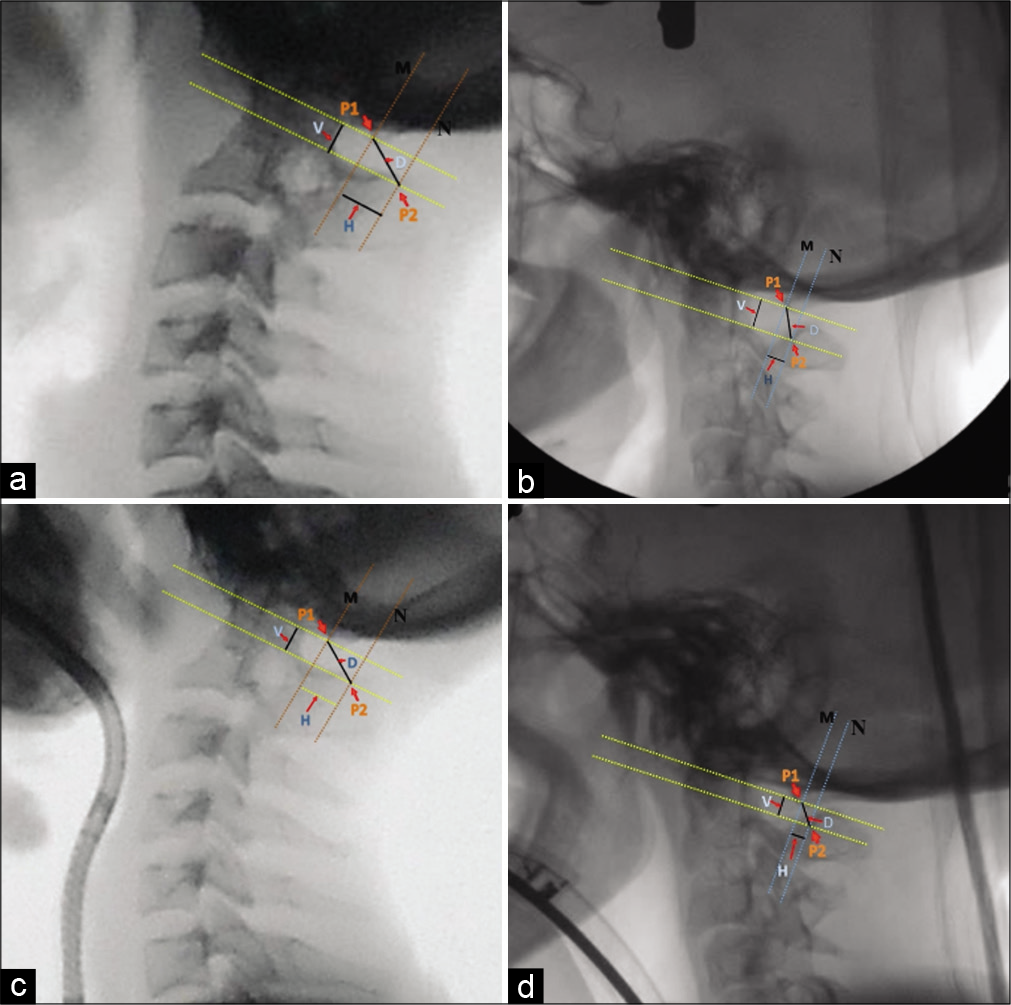
Figure 3:
Dynamic lateral radiograph of cervical spine with calculation of vertical, horizontal, and diagonal distances. (a and b) calculation of vertical, horizontal, and diagonal distances in neutral position. (c) Calculation of vertical, H, and diagonal distances during FOB and (d) calculation of vertical, H, and diagonal distances during VL.
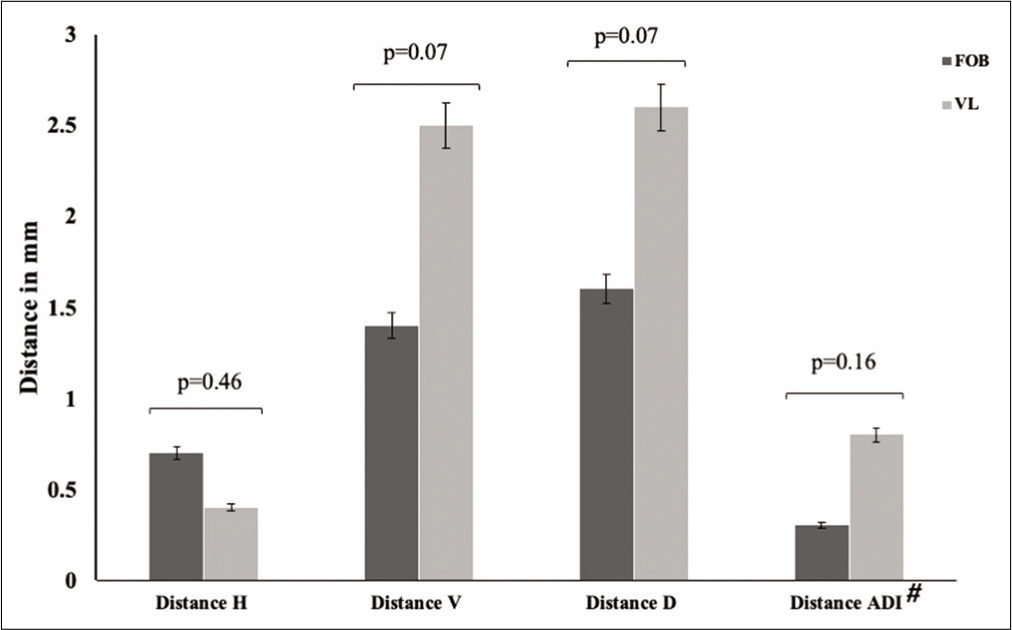
There was no difference between the two groups with respect to change of distances H, V, D, and ADI at maximum movement during intubation from baseline (P > 0.05) [
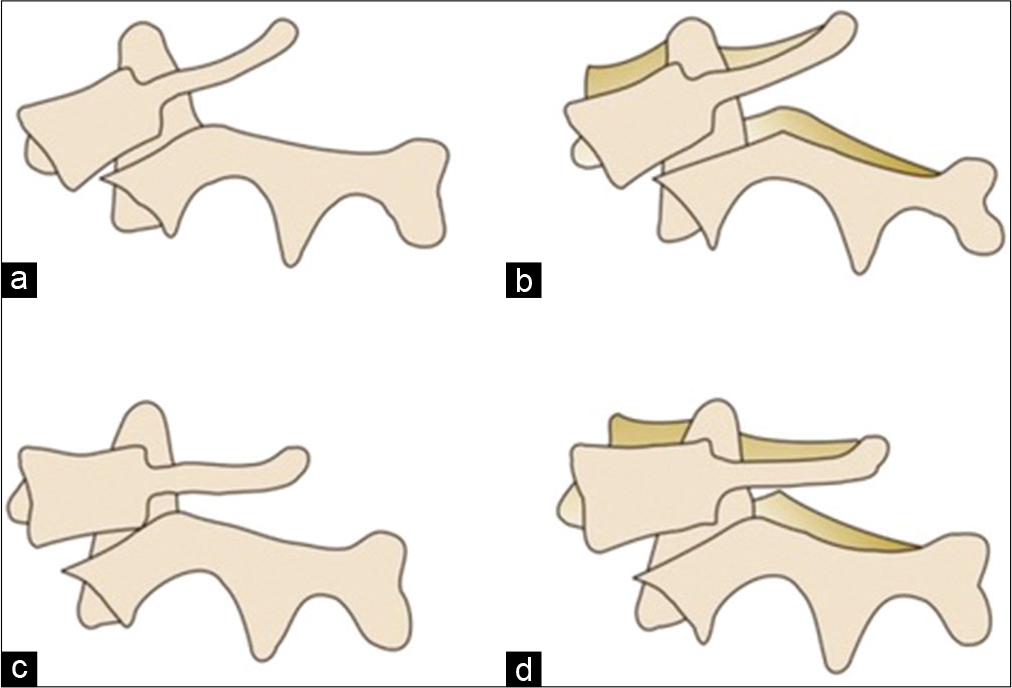
Figure 4:
Schematic diagram showing atlanto-axial instability. A (2-Dimention) and B (3-Dimension) show dislocation on flexion. C (2- Dimension) and D (3-Dimention) shows that the dislocation does not reduce on extension. However, the canal diameter does increase on extension. On extension the C1 lateral mass levers on the C2 lateral mass bringing the dens down. Note the reduction in vertical, horizontal and diagonal distance between C1 posterior arch and C2 spino-laminar junction on extension.
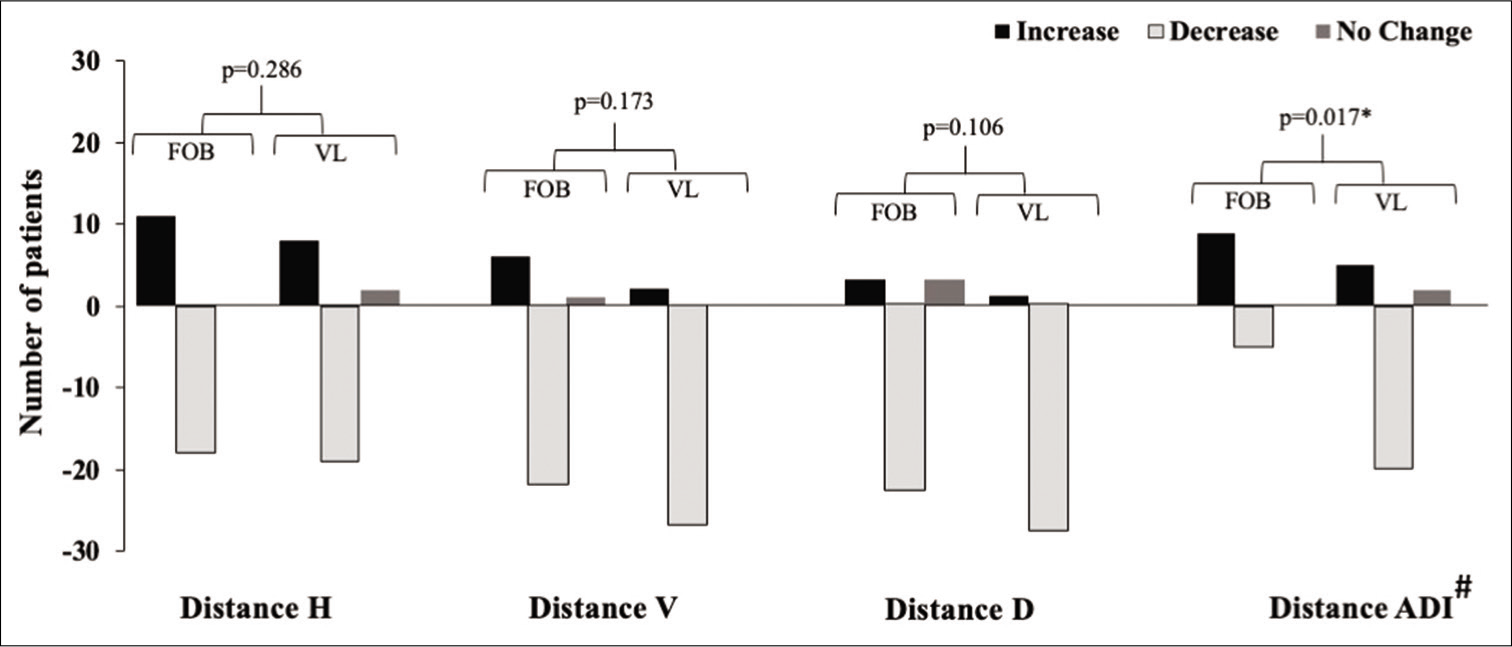
The incidence of change in ADI between two groups was found to be statistically significant (P = 0.017) [
DISCUSSION
Tracheal intubation in patients with AAD can be associated with neurological deterioration.[
Corroboration of data and its interpretation
We observed no significant changes in the mean H, V, and D distances between posterior elements of C1-C2 and ADI during intubation with FOB or VL. However, the number of patients who had reduction of ADI using VL was significantly more than those intubated using FOB. The observations of our study suggest that a decrease in ADI represents more potential space being available for the spinal cord. It can be inferred that there is no increase in cord compression during FOB or VL at CVJ. A possible explanation for the observed similarity in the two intubation techniques could be the presence of skeletal traction during the procedure. Cervical spine stabilization maneuvers such as traction and cervical collars are routinely used to prevent further insult to cervical cord.[
From previous studies, it was evident that the primary movement at the cervical spine during laryngoscopy is extension occurring at O-C1-C2 complex.[
Amongst patients in the FOB group 20 patients required the application of jaw thrust to facilitate better glottis visualization. It is possible, the application of jaw thrust caused movements at CVJ in this group of patients. These results were similar to the previous studies who demonstrated that pre-intubation maneuvers such as chin lift and jaw thrust resulted in cervical motion similar to some of the intubation techniques.[
Motor power was noted in preoperative period and compared postoperatively at 6-h. In VL group, motor power was comparable preoperatively and at 6-h postoperatively. In FOB group, only one patient had reduction in motor power from 5/5 in preoperative period to 4/5 in the left upper and lower limb in postoperative period. In this patient, the deficit was attributed to intraoperative surgical manipulations.
Challenges in measurement of canal space at CVJ and need for newer indices
CVJ is an extremely mobile segment and houses vital neurological structures. The AAD may occur in more than one plane, anteror-posterior, vertical, as well as in the lateral plane.[
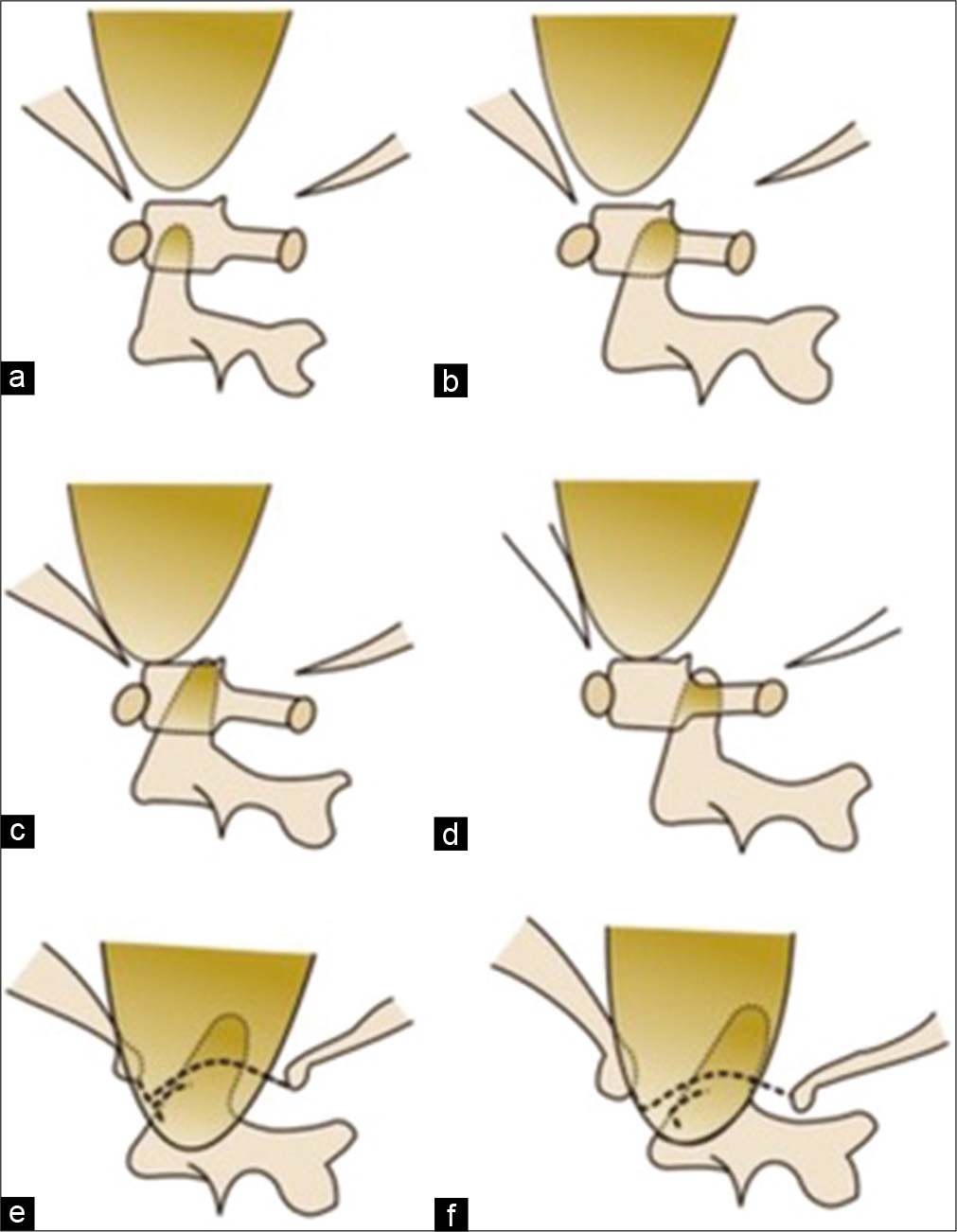
Figure 6:
(Mastoid overlapping sketch): Schematic diagram comparing C1-2 dislocation/basilar invagination in normal C1 to assimilated C1. (a and b) Well formed C1 and C2 with anterior-posterior dislocation. (c and d) Well formed C1 and C2 with anterior-posterior dislocation and basilar invagination (vertical dislocation). (e and f) Assimilated arch of atlas with anterior-posterior dislocation and basilar invagination. Note the mastoid obscures both the anterior arch and the dens in cases with assimilation on the lateral view. Therefore, ADI as well as PDI cannot be measured in such cases. The indices described here VH, HH, and DH can be measured in such cases.
Figure 7:
(CVJ flexion extension sketch): Schematic diagram showing atlanto-axial instability. (a - 2 dimensional) and (b - 3 dimensional) Dislocation on flexion. (c - 2 dimensional) and (d - 3 dimensional) shows that the dislocation does not reduce on extension. However, the canal diameter does increase on extension. On extension the C1 lateral mass levers on the C2 lateral mass bringing the dens down. Note the reduction in vertical, H, and diagonal distance between C1 posterior arch and C2 spino-laminar junction on extension.
Limitations
The major limitation of this study is that all the patients underwent intubation under general anesthesia. The protocol did not have a study arm evaluating the awake fiberoptic intubation. Consequently, the significance of an awake fiberoptic intubation on the CVJ kinematics could not be determined in this group of patients. Because of limitation of availability, intraoperative neuromonitoring could not be performed during the intubation in both groups. The dimensions measured in our study were those related to the upper cervical bony canal. There is a possibility of soft-tissue bulging into the spinal canal during intubation. It was not possible to measure the effect of soft-tissue while intubation. We have measured distances between the bony landmarks and extrapolated these distances to cervical spinal canal diameter. Measurement of cervical spinal canal could have been possible with the computed tomography (CT) imaging which was not feasible due to ethical and logistic issues. Application of jaw thrust was required in 20 cases of FOB group which contributed to significant movement. Finally, measurement of ADI was possible in only 14 out of 29 patients in FOB group and 27 out of 29 patients in VL group. In rest of the cases, ADI could not be assessed due to occipitalization of anterior arch of atlas and mastoid overlap.
CONCLUSION
The study evaluated the craniocervical kinetics during intubation in patients with CVJ anomalies in the presence of rigid skeletal traction. The results demonstrate that use of VL and FOB for intubation in the presence of cervical spine is comparable in terms of CVJ dynamics. An in-depth perusal of results on the basis of ADI may be advantageous in terms of greater widening of cervical spine diameter during intubation with VL when compared to FOB at CVJ.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Donaldson WF, Heil BV, Donaldson VP, Silvaggio VJ. The effect of airway maneuvers on the unstable C1-C2 segment. A cadaver study. Spine (Phila Pa 1976). 1997. 22: 1215-8
2. Donaldson WF, Towers JD, Doctor A, Brand A, Donaldson VP. A methodology to evaluate motion of the unstable spine during intubation techniques. Spine (Phila Pa 1976). 1993. 18: 2020-3
3. Dutta K, Sriganesh K, Chakrabarti D, Pruthi N, Reddy M. Cervical spine movement during awake orotracheal intubation with fiberoptic scope and McGrath videolaryngoscope in patients undergoing surgery for cervical spine instability: A randomized control trial. J Neurosurg Anesthesiol. 2020. 32: 249-55
4. Farmer J, Vaccaro A, Albert TJ, Malone S, Balderston RA, Cotler JM. Neurologic deterioration after cervical spinal cord injury. J Spinal Disord. 1998. 11: 192-6
5. Fielding JW, Hawkins RJ, Ratzan SA. Spine fusion for atlanto-axial instability. J Bone Joint Surg Am. 1976. 58: 400-7
6. Goel A, Shah A, Rajan S. Vertical mobile and reducible atlantoaxial dislocation. Clinical article. J Neurosurg Spine. 2009. 11: 9-14
7. Goel A. Goel’s classification of atlantoaxial “facetal” dislocation. J Craniovertebr Junction Spine. 2014. 5: 3-8
8. Greenberg AD. Atlanto-axial dislocations. Brain. 1968. 91: 655-84
9. Hastings RH, Kelley SD. Neurologic deterioration associated with airway management in a cervical spine-injured patient. Anesthesiology. 1993. 78: 580-3
10. Heidegger T, Gerig HJ, Ulrich B, Schnider TW. Structure and process quality illustrated by fibreoptic intubation: Analysis of 1612 cases. Anaesthesia. 2003. 58: 734-9
11. Hindman BJ, From RP, Fontes RB, Traynelis VC, Todd MM, Zimmerman MB. Intubation biomechanics: Laryngoscope force and cervical spine motion during intubation in cadaverscadavers versus patients, the effect of repeated intubations, and the effect of Type II odontoid fracture on C1-C2 motion. Anesthesiology. 2015. 123: 1042-58
12. Hirabayashi Y, Fujita A, Seo N, Sugimoto H. A comparison of cervical spine movement during laryngoscopy using the Airtraq or Macintosh laryngoscopes. Anaesthesia. 2008. 63: 635-40
13. Jain VK, Behari S. Management of congenital atlanto-axial dislocation: Some lessons learnt. Neurol India. 2002. 50: 386-97
14. Jain VK. Atlantoaxial dislocation. Neurol India. 2012. 60: 9-17
15. Maruyama K, Yamada T, Kawakami R, Hara K. Randomized cross-over comparison of cervical-spine motion with the AirWay Scope or Macintosh laryngoscope with in-line stabilization: A video-fluoroscopic study. Br J Anaesth. 2008. 101: 563-7
16. Muckart DJ, Bhagwanjee S, van der Merwe R. Spinal cord injury as a result of endotracheal intubation in patients with undiagnosed cervical spine fractures. Anesthesiology. 1997. 87: 418-20
17. Passias PG, Wang S, Kozanek M, Wang S, Wang C. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech. 2013. 26: 15-21
18. Powell RM, Heath KJ. Quadraplegia in a patient with an undiagnosed odontoid peg fracture. The importance of cervical spine immobilisation in patients with head injuries. J R Army Med Corps. 1996. 142: 79-81
19. Redl G. Massive pyramidal tract signs after endotracheal intubation: A case report of spondyloepiphyseal dysplasia congenita. Anesthesiology. 1998. 89: 1262-4
20. Robitaille A, Williams SR, Tremblay MH, Guilbert F, Thériault M, Drolet P. Cervical spine motion during tracheal intubation with manual in-line stabilization: Direct laryngoscopy versus GlideScope videolaryngoscopy. Anesth Analg. 2008. 106: 935-41
21. Salunke P, Sahoo SK, Deepak AN, Khandelwal NK. Redefining congenital atlantoaxial dislocation: Objective assessment in each plane before and after operation. World Neurosurg. 2016. 95: 156-64
22. Shetty A, Kumar A, Chacko A, Guthe S, Kini AR. Reduction techniques in the management of atlantoaxial subluxation. Indian J Orthop. 2013. 47: 333-9
23. Simmons ST, Schleich AR. Airway regional anesthesia for awake fiberoptic intubation. Reg Anesth Pain Med. 2002. 27: 180-92
24. Swain A, Bhagat H, Gupta V, Salunke P, Panda NB, Sahu S. Intubating laryngeal mask airway-assisted flexible bronchoscopic intubation is associated with reduced cervical spine motion when compared with C-MAC video laryngoscopy-guided intubation: A prospective randomized cross over trial. J Neurosurg Anesthesiol. 2020. 32: 242-8
25. Swarbrick C, Turner M. Awake nasal intubation: From darkness into light, or a leap into the unknown?. Anaesthesia. 2015. 70: 881-2
26. Takenaka I, Aoyama K, Iwagaki T, Ishimura H, Takenaka Y, Kadoya T. Approach combining the airway scope and the bougie for minimizing movement of the cervical spine during endotracheal intubation. Anesthesiology. 2009. 110: 1335-40
27. Tokunaga D, Hase H, Mikami Y, Hojo T, Ikoma K, Hatta Y. Atlantoaxial subluxation in different intraoperative head positions in patients with rheumatoid arthritis. Anesthesiology. 2006. 104: 675-9
28. Turkstra TP, Pelz DM, Jones PM. Cervical spine motion: A fluoroscopic comparison of the AirTraq laryngoscope versus the Macintosh laryngoscope. Anesthesiology. 2009. 111: 97-101
29. Wong DM, Prabhu A, Chakraborty S, Tan G, Massicotte EM, Cooper R. Cervical spine motion during flexible bronchoscopy compared with the Lo-Pro GlideScope. Br J Anaesth. 2009. 102: 424-30
30. Yan K, Diggan MF. A case of central cord syndrome caused by intubation: A case report. J Spinal Cord Med. 1997. 20: 230-2
31. Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014. 4: 197-210