- Department of Neurosurgery, All India Institute of Medical Sciences, Patna, Bihar, India.
- Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India.
Correspondence Address:
Saraj Kumar Singh, Department of Neurosurgery, All India Institute of Medical Sciences, Patna, Bihar, India.
DOI:10.25259/SNI_650_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anand Kumar Das1, Saraj Kumar Singh1, Subhash Kumar2. Filar arteriovenous fistula mimicking upper motor neuron palsy: A case report with review of the literature. 26-Aug-2022;13:385
How to cite this URL: Anand Kumar Das1, Saraj Kumar Singh1, Subhash Kumar2. Filar arteriovenous fistula mimicking upper motor neuron palsy: A case report with review of the literature. 26-Aug-2022;13:385. Available from: https://surgicalneurologyint.com/surgicalint-articles/11826/
Abstract
Background: Filar A-V fistula is a rare entity. It requires a high degree of suspicion to diagnose. Magnetic resonance imaging (MRI) findings are often nonspecific and spinal angiogram is required to diagnose it.
Case Description: A 63-year-old male patient presented with Grade 4 spastic paraplegia and significant sensory disturbance below D8 level along with severe vesicorectal dysfunction. On imaging flow voids were present at lower dorsal and lumbar level in MRI (T2 sequence). Patient underwent spinal digital substraction angiography (DSA) which was suggestive of filar fistula at L4-L5 level. Patient underwent surgical exploration with L4-5 laminectomy. Feeding artery was identified using indigocyanine green (ICG) dye and excised along with filum and dilated vessels. Patient recovered symptomatically in postoperative period.
Conclusion: Filar fistula is a rare lesion and it presents with long standing progressive congestive myelopathy. It requires a high degree of suspicion to diagnose it. DSA is the gold standard for diagnosis and management planning. Surgical approach utilizing the ICG dye is best treatment options in such cases.
Keywords: Filar arteriovenous fistula, Myelopathy, Spinal angiogram, Venous hypertension
INTRODUCTION
Filar arteriovenous (A-V) fistula is a rare type of A-V shunt. It is a direct communication of artery of filum terminale and a single draining vein. These types of fistulas are 3 times more common in males than females.[
CASE REPORT
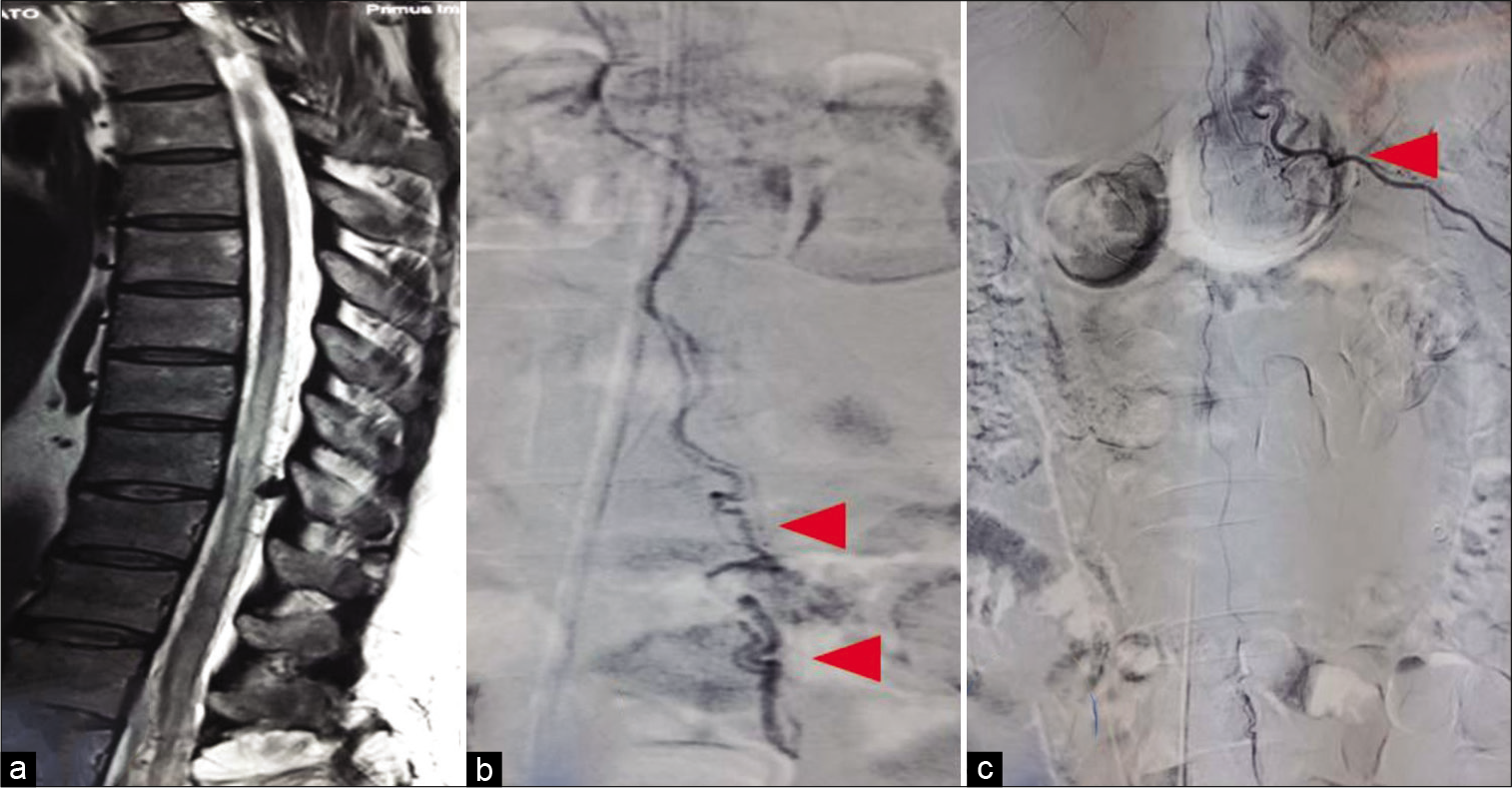
A 63-year-old male patient presented with insidious onset gradually progressive difficulty in walking, decreased sensation below chest, and bladder bowel dysfunction for the past 11 years. The patient was operated for lumbar spondylolisthesis 11 years back. Multiple MRIs (whole spine) were done at different hospitals but no definite diagnosis was reached. His neurological deficit continued to worsen and he became paraplegic. On examination, he was found to have spastic paraplegia (power – 0/5 in both lower limb, tone – spasticity, and bulk reduced in both lower limbs). There was significant sensory disturbance below D8 level along with severe vesicorectal dysfunction. Deep tendon reflexes were absent in the lower limb but normal in the upper limb. Plantars were extensor on both sides. Cerebral MRI was normal. MRI spine revealed multiple flow voids at lumbosacral level in T2 with cord signal changes at dorsolumbar level [
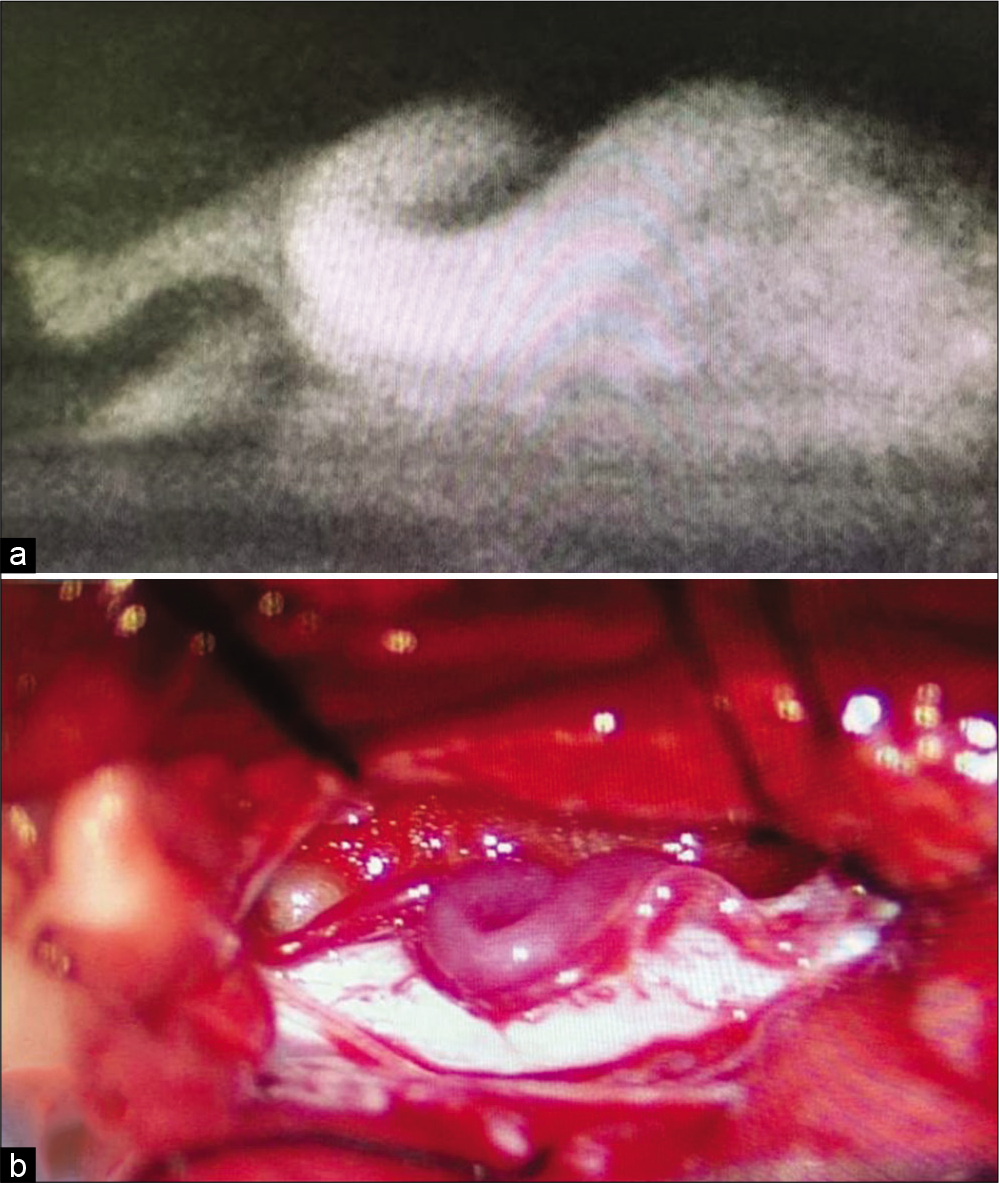
Patient underwent surgery with L4-5 laminectomy. Thecal sac was opened over virgin area at L4 level. On opening dura, dilated veins were visualized posterior to the filum. Indigocyanine green (ICG) was injected to identify feeding and draining vessels [
DISCUSSION
Filum terminale AV fistula (AVF) is a rare variety of spinal AV shunt.[
Patients usually present with dysesthesias, nondermatomal sensory loss, walking difficulty, wasting, and weakness of lower limbs, buttock pain, and sphincter dysfunction. Due to nonspecific clinical manifestations and rarity, this condition is usually misdiagnosed as polyneuropathy, polyradiculopathy, or intramedullary tumor.[
MRI is first diagnostic step for such patients of progressive myelopathy. Prominent vascular flow voids and vascular enhancement around conus and lower dorsal spinal cord are common diagnostic findings in MRI T2 sequence. However, to differentiate between perimedullary fistula and filar fistula, spinal angiogram is necessary. DSA is must for characterization of the angioarchitecture of the lesion. It identifies all arterial feeders, draining vein, and fistulous connection. It also detects any additional associated spinal vascular malformations. On DSA, filar fistula is typically characterized by a focal, single fistula located well below the conus in the lower lumbar spine. The fistulous point is usually defined by the transition from the smaller artery to the larger proximal draining vein.[
Main therapeutic target is complete obliteration of fistula with preservation of spinal cord circulation. Surgical intervention is the most favored treatment for filar fistula in expert hands.
Surgery is advocated when filar fistula has a single feeder with long distance to the AVF and is safer than endovascular treatment. The overall success rate is close to 100%, and complication rates are low (<5%).[
Endovascular procedure and embolization requires selection of microcatheter for arterial feeder and navigation at the most distal part of the artery, just proximal to the fistula. Risk of anterior spinal artery (ASA) dissection, thrombosis, or vasospasm is very high while manipulation. High flow fistulae can cause dilatation of ASA making manipulation with microcatheter safer. However, still surgical management is recommended due to low morbidity and high occlusion rate.[
CONCLUSION
Filar fistula is a rare lesion and it presents with long standing progressive congestive myelopathy. DSA is the gold standard for diagnosis and management planning. Surgical approach utilizing the ICG dye is best treatment options in such cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Fischer S, Perez MA, Bassiouni H, Hopf N, Bäzner H, Henkes H. Arteriovenous fistula of the filum terminale: Diagnosis, treatment, and literature review. Clin Neuroradiol. 2013. 23: 309-14
2. Flores B, Klinger D, White J, Batjer H. Spinal vascular malformations: Treatment strategies and outcome. Neurosurg Rev. 2016. 40: 15-28
3. Giordan E, Brinjikji W, Ciceri E, Lanzino G. Arteriovenous fistulae of the filum terminale. J Neurointerv Surg. 2017. 10: 191-7
4. Jellema K, Tijssen CC, van Gijn J. Spinal dural arteriovenous fistulas: A congestive myelopathy that initially mimics a peripheral nerve disorder. Brain. 2006. 129: 3150-64
5. Kumar A, Deopujari CE, Mhatre M. Misdiagnosis in a case of non-compressive myelopathy due to a lumbar spinal intradural fistula supplied by the artery of adamkiewicz. Surg Neurol Int. 2011. 2: 12
6. Trinh VT, Duckworth EA. Surgical excision of filum terminale arteriovenous fistulae after lumbar fusion: Value of indocyanine green and theory on origins (a technical note and report of two cases). Surg Neurol Int. 2011. 2: 63
7. Wajima D, Nakagawa I, Park HS, Haku T, Wada T, Kichikawa K. A case of filum terminale arterial venous fistula needed a long arterial access for trans-arterial shunt obliteration. Interv Neuroradiol. 2017. 23: 221-7
8. Witek A, Cerejo R, Elgabaly M, Bain M. Diagnosis and microsurgical ligation of an intradural ventral (Type IV) arteriovenous fistula of the filum terminale: 3-dimensional operative video. Oper Neurosurg. 2018. 15: 475-6
9. Witiw CD, Fallah A, Radovanovic I, Wallace MC. Sacral intradural arteriovenous fistula treated indirectly by transection of the filum terminale: Technical case report. Neurosurgery. 2011. 69: E780-4