- Departments of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico,
- Department of Internal Medicine, Instituto Mexicano del Seguro Social, León, Mexico.
- Departments of Neuroinfectology, National Institute of Neurology and Neurosurgery, Mexico,
Correspondence Address:
Marcos Vinicius Sangrador-Deitos
Departments of Neuroinfectology, National Institute of Neurology and Neurosurgery, Mexico,
DOI:10.25259/SNI_506_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marcos Vinicius Sangrador-Deitos, Jimena Alejandra González Olvera, Heidy Adames Espinal, Graciela Cárdenas Hernández, Verónica Angeles Morales, José Luis Soto Hernandez. Fungal mycotic aneurysm in a patient with Aspergillus terreus chronic meningoencephalitis. 06-Jun-2020;11:139
How to cite this URL: Marcos Vinicius Sangrador-Deitos, Jimena Alejandra González Olvera, Heidy Adames Espinal, Graciela Cárdenas Hernández, Verónica Angeles Morales, José Luis Soto Hernandez. Fungal mycotic aneurysm in a patient with Aspergillus terreus chronic meningoencephalitis. 06-Jun-2020;11:139. Available from: https://surgicalneurologyint.com/surgicalint-articles/10067/
Abstract
Background: Central nervous system involvement due to aspergillosis is an extremely serious entity, particularly in patients with severe neutropenia, hematological diseases, or post-transplant cases. Immunocompetent patients can be infected by intense exposure, particularly iatrogenic after invasive procedures.
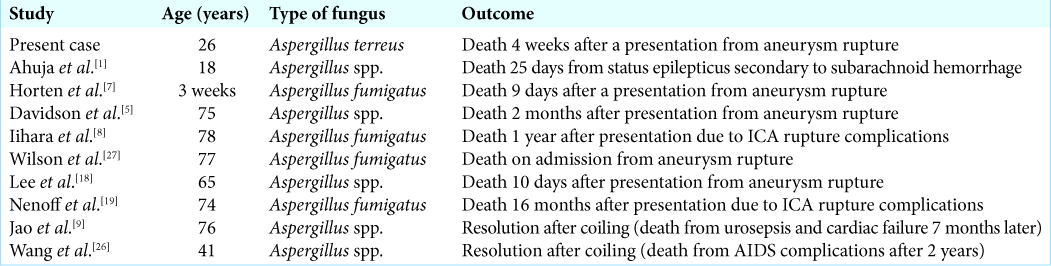
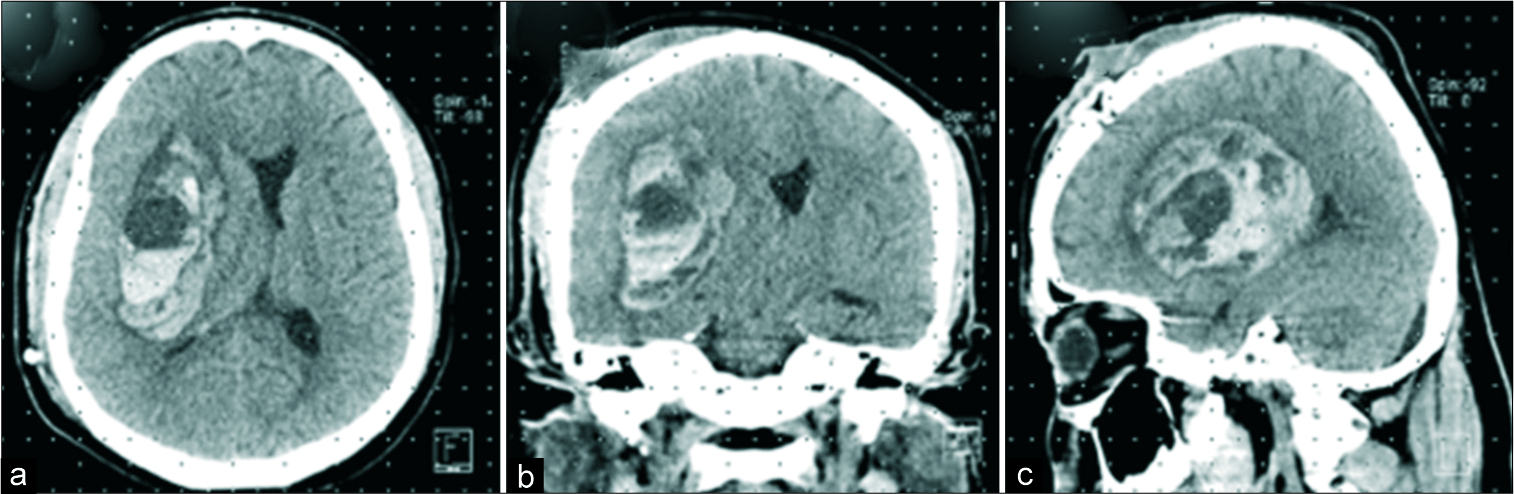
Case Description: We present the case of a 26-year-old male with a 1 year appendectomy background, which required epidural anesthesia. After that surgery, insidious headache presented, requiring mild analgesics for adequate control. In the following weeks, headaches increased and tomographic imaging revealed hydrocephalus. A ventriculoperitoneal shunt was placed, and empirical treatment for neurocysticercosis was established, but diagnosis was never confirmed. Sequentially, shunt dysfunction occurred twice, for which shunt replacement was performed. Cerebrospinal fluid and shunt’s catheter were cultured. Some days later, a filamentous fungus was isolated and finally identified as Aspergillus sp. Intravenous amphotericin B and fluconazole at therapeutic dosage were administered; however, a torpid clinical evolution was observed. After a 2-week antifungal scheme, the fungus was identified as Aspergillus terreus. The patient developed sudden rostrocaudal deterioration. Computed tomography imaging was done, revealing a 70 cc hematoma in the right operculoinsular region, midline shift, and a 9 mm saccular aneurysm at the bifurcation of the middle cerebral artery.
Conclusion: Cerebral aspergillosis is a serious disease with high mortality in patients, particularly those without identifiable risk factors. The iatrogenic forms are serious, due to the delay of clinical diagnosis. It is important to have a high index of suspicion in patients with a history of invasive procedures such as epidural anesthesia or surgery, and who develop a persistent chronic headache or chronic meningitis.
Keywords: Aneurysm, Aspergillus terreus, Mycotic
INTRODUCTION
In 1885, William Osler was the first to describe an aortic aneurysm secondary to infectious endocarditis.[
CASE DESCRIPTION
We present the case of a 26-year-old non-HIV male with a 1-year background appendectomy, which required epidural anesthesia. After surgery, he presented an insidious headache, requiring mild analgesics for adequate control. In the following weeks, headaches increased and tomographic imaging revealed hydrocephalus. A ventriculoperitoneal shunt was installed for suspicion of neurocysticercosis. Even though treatment was initiated, there was no clinical improvement. Sequentially, during hospital stay, shunt dysfunction occurred twice, for which shunt replacement was performed. Cerebrospinal fluid (CSF) and shunt’s catheter were cultured, identifying a filamentous fungus. CSF and serum galactomannan tests were positive for Aspergillus spp.: 9.4 ng/dl and 5.8 ng/dL, respectively. Intravenous amphotericin B and fluconazole were administered; however, a torpid clinical evolution was observed. The filamentous fungus was finally sequenced as Aspergillus terreus. After a 2-week antifungal scheme, sudden rostrocaudal deterioration appeared. Computed tomography imaging was done, revealing a 70 cc hematoma in the right operculoinsular region, midline shift [
DISCUSSION
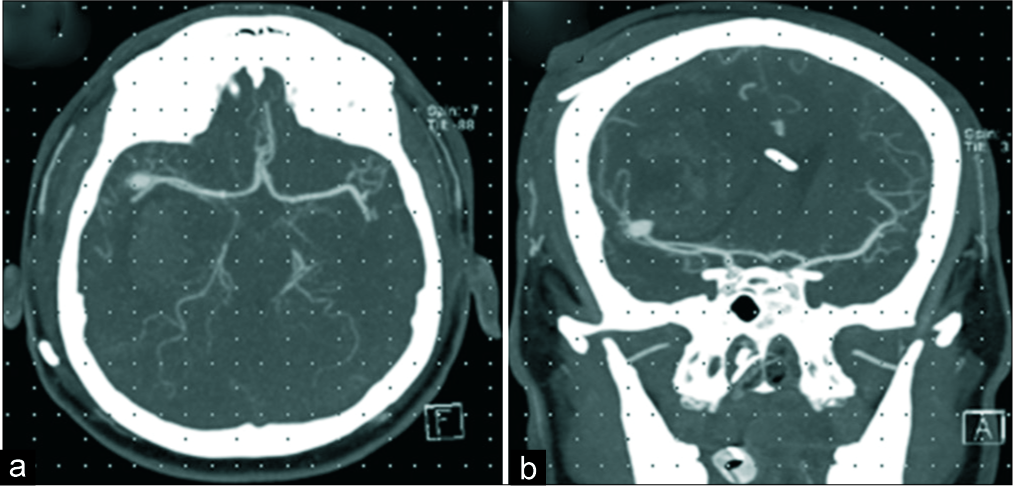
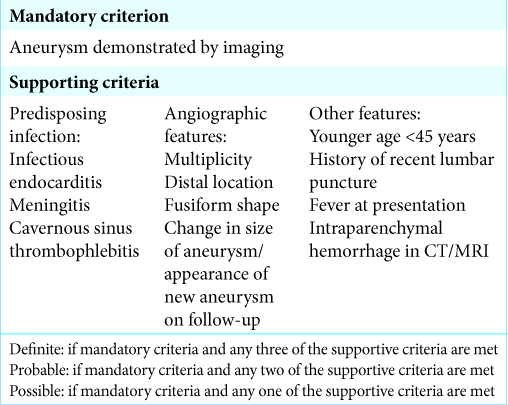
Fungal cerebral MAs are most commonly seen in patients with immunocompromised states, such as AIDS or complicated diabetes mellitus.[
Iatrogenic fungal infections of the central nervous system must be suspected in patients with meningitis and a background of epidural invasive procedures such as anesthesia or any drug administration.[
CONCLUSION
We present the first case report of a fungal MA of the middle cerebral artery bifurcation caused by A. terreus, a fungus found worldwide in soil. It has been reported to cause pathologic states in immunocompromised patients; however, our patient showed no evidence of immunocompromise whatsoever. Intrathecal inoculation following epidural anesthesia represents the form of transmission, which should be always taken into account with patients presenting this background history. The lethal outcome observed, depicts the intrinsic resistance this pathogen presents for amphotericin, which has been administered to the patient. Even though the wide range of diagnostic studies and treatment strategies, fungal central nervous system infections remain a diagnosis challenge which requires high suspicion and continues to be have one of the highest mortality rates among neurological diseases.
Declaration of patient consent
Patient’s consent is not required as identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahuja G, Jain N, Vijayaraghavan M, Roy S. Cerebral mycotic aneurysm of fungal origin. Case report. J Neurosurg. 1978. 49: 107-10
2. Akhaddar A, Diabira S, Turgut M, Challa S, Akhaddar A.editors. Intracranial fungal aneurysms. Fungal Infections of the Central Nervous System. Cham, Switzerland: Springer International Publishing; 2019. p. 327-34
3. Allen LM, Fowler AM, Walker C, Derdeyn CP, Nguyen BV, Hasso AN. Retrospective review of cerebral mycotic aneurysms in 26 patients: Focus on treatment in strongly immunocompromised patients with a brief literature review. AJNR Am J Neuroradiol. 2013. 34: 823-7
4. Azar MM, Assi R, Patel N, Malinis MF. Fungal mycotic aneurysm of the internal carotid artery associated with sphenoid sinusitis in an immunocompromised patient: A case report and review of the literature. Mycopathologia. 2016. 181: 425-33
5. Davidson P, Robertson D. A true mycotic (Aspergillus) aneurysm leading to fatal subarachnoid hemorrhage in a patient with hereditary hemorrhagic telangiectasia. Case report. J Neurosurg. 1971. 35: 71-6
6. Gunaratne PS, Wijeyaratne CN, Chandrasiri P, Sivakumaran S, Sellahewa K, Perera P. An outbreak of Aspergillus meningitis following spinal anaesthesia for caesarean section in Sri Lanka: A post-tsunami effect?. Ceylon Med J. 2006. 51: 137-42
7. Horten B, Abbott G, Porro R. Fungal aneurysms of intracranial vessels. Arch Neurol. 1976. 33: 577-9
8. Iihara K, Makita Y, Nabeshima S, Tei T, Keyaki A, Nioka H. Aspergillosis of the central nervous system causing subarachnoid hemorrhage from mycotic aneurysm of the basilar artery--case report. Neurol Med Chir (Tokyo). 1990. 30: 618-23
9. Jao SY, Weng HH, Wong HF, Wang WH, Tsai YH. Successful endovascular treatment of intractable epistaxis due to ruptured internal carotid artery pseudoaneurysm secondary to invasive fungal sinusitis. Head Neck. 2011. 33: 437-40
10. Johnson M, Perfect J. Use of antifungal combination therapy: Agents, order, and timing. Curr Fungal Infect Rep. 2010. 4: 87-95
11. Kainer MA, Reagan DR, Nguyen DB, Wiese AD, Wise ME, Ward J. Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012. 367: 2194-203
12. Kannoth S, Iyer R, Thomas SV, Furtado SV, Rajesh BJ, Kesavadas C. Intracranial infectious aneurysm: Presentation, management and outcome. J Neurol Sci. 2007. 256: 3-9
13. Kannoth S, Thomas S. Intracranial microbial aneurysm (infectious aneurysm): Current options for diagnosis and management. Neurocrit Care. 2009. 11: 120-9
14. Kannoth S, Thomas SV, Nair S, Sarma PS. Proposed diagnostic criteria for intracranial infectious aneurysms. J Neurol Neurosurg Psychiatry. 2008. 79: 943-6
15. Kauffman C, Pappas P, Patterson T. Fungal infections associated with contaminated methylprednisolone injections. N Engl J Med. 2013. 368: 2495-500
16. Klont R, Mennink-Kersten M, Verweij P. Utility of Aspergillus antigen detection in specimens other than serum specimens. Clin Infect Dis. 2004. 39: 1467-74
17. Lahoti S, Berger J. Iatrogenic fungal infections of the central nervous system. Curr Neurol Neurosci Rep. 2013. 13: 399-
18. Lee DH, Yoon TM, Lee JK, Joo JE, Park KH, Lim SC. Invasive fungal sinusitis of the sphenoid sinus. Clin Exp Otorhinolaryngol. 2014. 7: 181-7
19. Nenoff P, Kellermann S, Horn LC, Keiner S, Bootz F, Schneider S. Case report. Mycotic arteritis due to Aspergillus fumigatus in a diabetic with retrobulbar aspergillosis and mycotic meningitis. Mycoses. 2001. 44: 407-14
20. Oppe W. Zur kentniss der schimmelmymykosen beim menschen. Z Allg Path. 1897. 8: 301-6
21. Osler W. The Gulstonian lectures, on malignant endocarditis. Br Med J. 1885. 1: 467-70
22. Roach M, Drake C. Ruptured cerebral aneurysms caused by micro-organisms. N Engl J Med. 1965. 273: 240-4
23. Rodrigo N, Perera KN, Ranwala R, Jayasinghe S, Warnakulasuriya A, Hapuarachchi S. Aspergillus meningitis following spinal anaesthesia for caesarean section in Colombo, Sri Lanka. Int J Osbtet Anesth. 2007. 16: 256-60
24. Suwanwela C, Suwanwela N, Charuchinda S, Hongsaprabhas C. Intracranial mycotic aneurysms of extravascular origin. J Neurosurg. 1972. 36: 552-9
25. Venkatesh SK, Phadke RV, Kalode RR, Kumar S, Jain VK. Intracranial infective aneurysms presenting with haemorrhage: An analysis of angiographic findings, management and outcome. Clin Radiol. 2000. 55: 946-53
26. Wang H, Rammos S, Fraser K, Elwood P. Successful endovascular treatment of a ruptured mycotic intracavernous carotid artery aneurysm in an AIDS patient. Neurocrit Care. 2007. 7: 156-9
27. Wilson WR, Hawrych A, Olan W. Rapid development of bilateral internal carotid artery aneurysm from sphenoid sinus aspergillosis. Skull Base Surg. 1998. 8: 211-4