- Department of Surgery, US Naval Hospital Okinawa, Okinawa, United States.
- Department of Neurosurgery, Walter Reed National Military Medical Center, Bethesda, Maryland, United States.
- Department of Neurosurgery, Naval Medical Center San Diego, San Diego, California, United States.
Correspondence Address:
Daniel Satoshi Ikeda
Department of Neurosurgery, Naval Medical Center San Diego, San Diego, California, United States.
DOI:10.25259/SNI_762_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniel Satoshi Ikeda1, Charles A. Miller2, Vijay M. Ravindra3. Fusion for subaxial bow hunter’s syndrome results in remote osseous remodeling of the hyperostotic growth responsible for vertebral artery compression. 17-Mar-2021;12:104
How to cite this URL: Daniel Satoshi Ikeda1, Charles A. Miller2, Vijay M. Ravindra3. Fusion for subaxial bow hunter’s syndrome results in remote osseous remodeling of the hyperostotic growth responsible for vertebral artery compression. 17-Mar-2021;12:104. Available from: https://surgicalneurologyint.com/surgicalint-articles/10647/
Abstract
Background: The authors present a previously unreported case of a patient with diffuse idiopathic skeletal hyperostosis (DISH) who developed bow hunter’s syndrome (BHS) or positional vertebrobasilar insufficiency. In addition, the authors demonstrate angiographic evidence of remote osseous remodeling after segmental fusion without direct decompression of the offending bony growth. BHS is a rare, yet well established, cause of posterior circulation ischemia and ischemic stroke. Several etiologies such as segmental instability and spondylosis have been described as causes, however, DISH has not been associated with BHS before this publication.
Case Description: A 77-year-old man who presented with BHS was found to have cervical spine changes consistent with DISH, and angiography confirmed right vertebral artery (VA) stenosis at C4–5 from a large pathological elongation of the right C5 lateral mass. Head rotation resulted in occlusion of the VA. The patient underwent an anterior cervical discectomy and fusion and reported complete resolution of his symptoms. A delayed angiogram and CT of the cervical spine demonstrated complete resolution of the baseline stenosis, no dynamic compression, and remote osseous remodeling of the growth, respectively.
Conclusion: This case represents the first publication in the literature of DISH as a causative etiology of BHS and of angiographic data demonstrating resolution of a compressive osseous pathology without direct decompression in BHS.
Keywords: Bow hunter’s syndrome, Cervical fusion, Diffuse idiopathic skeletal hyperostosis, Digital subtraction angiography, osseous remodeling, Positional vertebrobasilar insufficiency
INTRODUCTION
Bow hunter’s syndrome (BHS), or positional vertebrobasilar insufficiency, is a rare, yet well-established etiology of posterior circulation ischemia and stroke.[
To the best of our knowledge, this is the first report of BHS in association with DISH. In addition, the authors present angiographic data that have not been previously reported, where the offending osseous growth remodels after fusion without direct decompression.
CASE REPORT
History and examination
This 77-year-old man with a medical history including coronary artery disease and dysrhythmia presented to the neurosurgery clinic after months of evaluations for repeated episodes of presyncope and at least four syncopal events, where the patient was found unconscious or had awoken on the ground after presumably losing consciousness. The patient reported these symptoms and events were preceded by turning his head to the right. In some instances, the patient reported double vision in conjunction with the presyncopal symptoms.
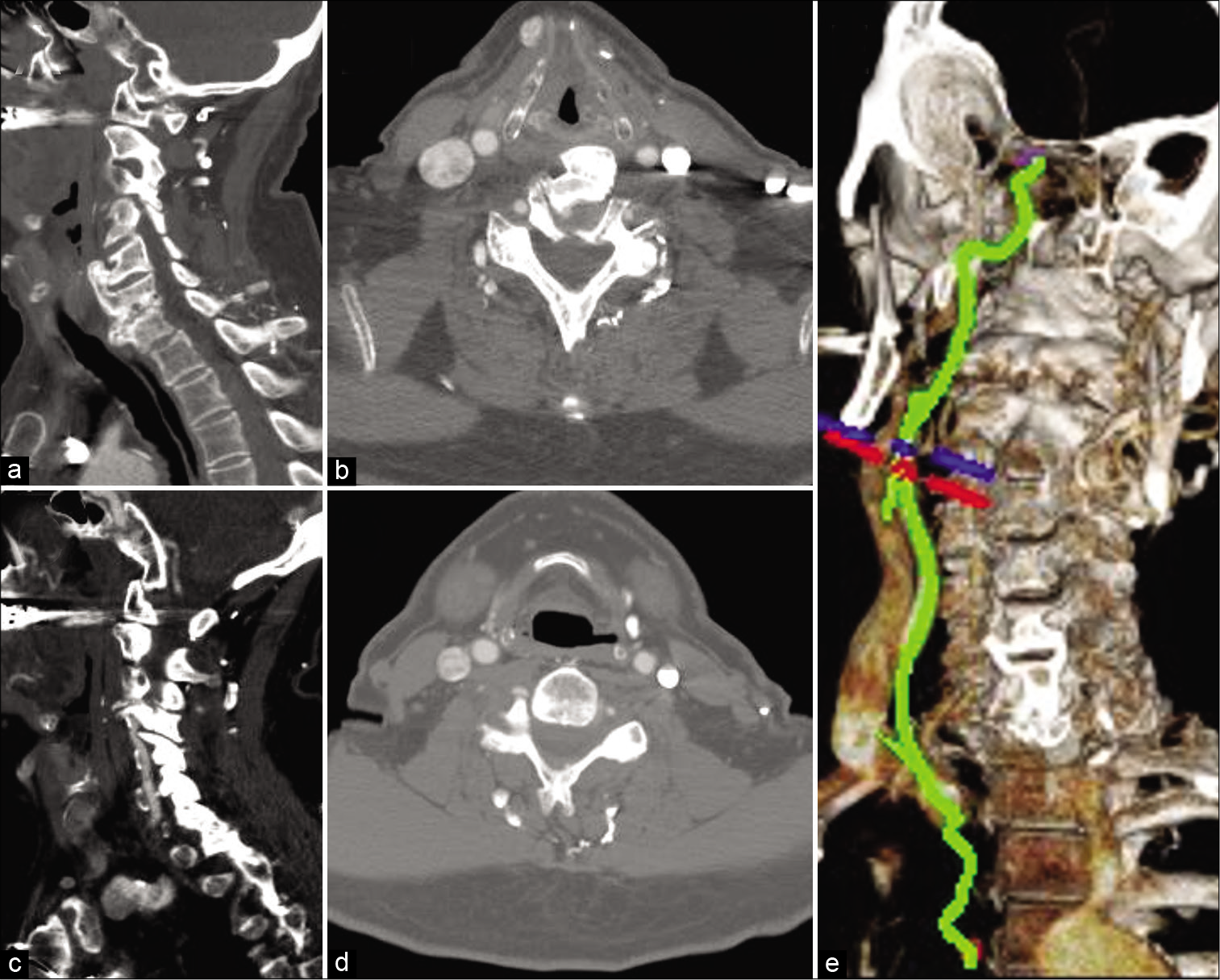
On physical examination, the patient was neurologically intact. He was able to reproduce the symptoms with head rotation of approximately 45° to the right. As a matter of safety, these assessments were performed in short intervals as to not elicit a full syncopal event. Diplopia was not detected. A CT angiogram (CTa) of the head and neck demonstrated osseous changes consistent with cervical DISH as well as a “fang”-like osseous elongation of the right C5 lateral mass, which protruded into the vertebral foramen and compressed the VA [
Figure 1
: Preoperative CTa sagittal (a and c) reconstructions demonstrate the changes associated with diffuse idiopathic skeletal hyperostosis and the “fang”-like elongation of the C5 lateral mass (black circle) with mass effect on the vertebral artery. Axial (b and d) reconstructions demonstrate ventral osteophytes (white arrow) which displace the esophagus (white arrowheads) and display the osseous growth (black arrow). A 3D reconstruction (e) further details the precise anatomical location of the stenosis at C4–5.
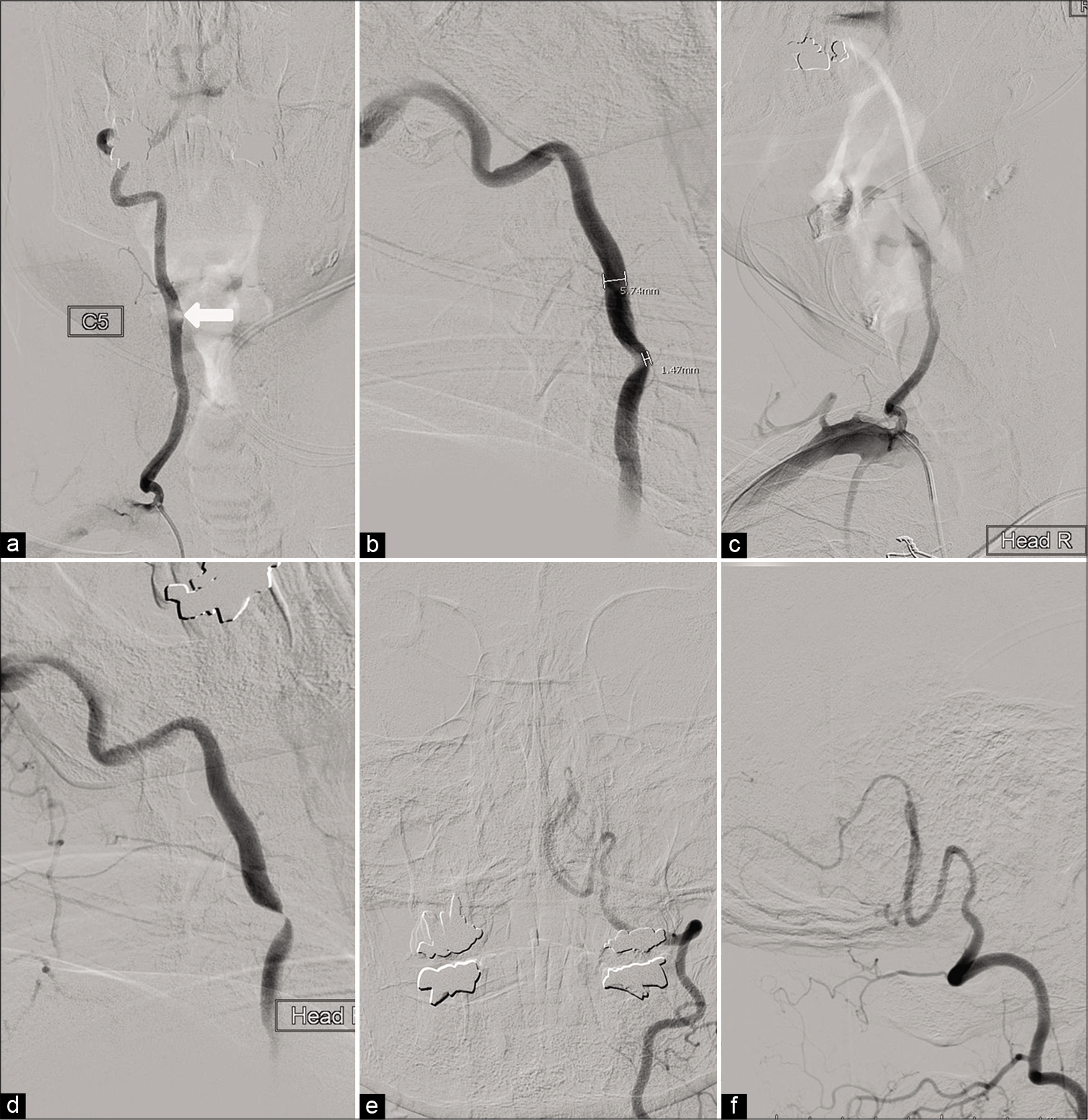
Figure 2:
AP (a) and lateral (b) cervical right vertebral artery (VA) digital subtraction angiography demonstrates the compression in neutral (white arrow) and occlusion with head rotation (c and d). AP (e) and lateral (f) left VA angiography demonstrates the artery ends in the left posterior inferior cerebellar artery and does not join the right VA.
Operation
A C4–5 anterior cervical discectomy and fusion (ACDF) was performed under general endotracheal anesthesia. The traditional Smith-Robinson approach to the cervical spine was employed and special care was taken not to injure the esophagus, which had been displaced to the right of the cervical spine by large hyperostotic osteophytes. In addition to the C4–5 discectomy, partial osteophyte removal was required at C5 to allow for the plating system to lay flat. A structural allograft and low-profile titanium plating system was used to complete the surgery.
Postoperative course
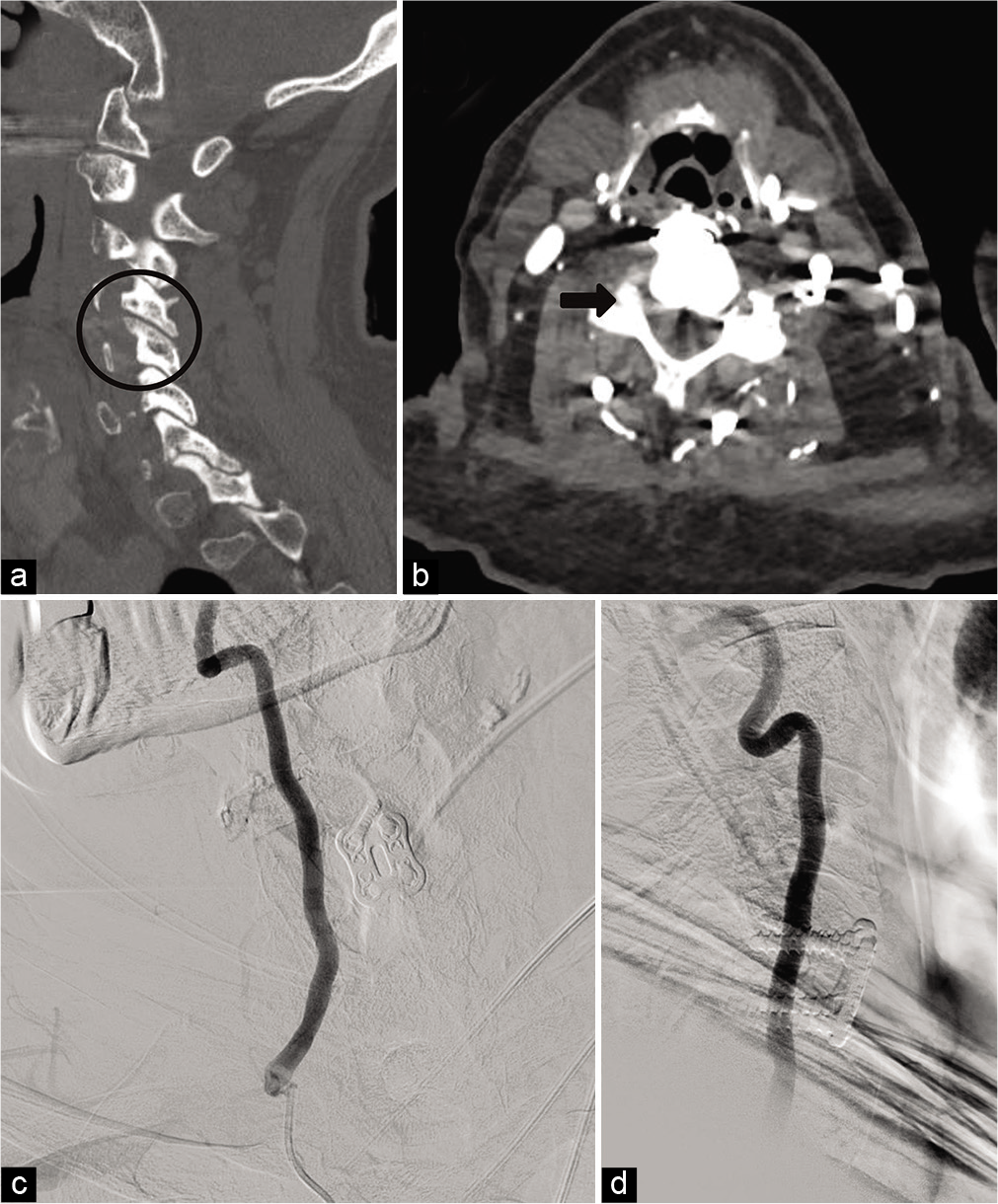
The patient tolerated surgery well and was discharged on postoperative day 1. He had an uneventful recovery and reported complete resolution of his symptoms with head rotation. Approximately 9 months after surgery, the patient underwent a repeat CTa and DSA as part of an evaluation for cardiac dysrhythmia. The CTa demonstrated blunting of the osseous growth at C5, and the DSA showed no evidence of VA compression in the neutral or dynamic positions [
Figure 3:
A postoperative CTa sagittal (a) and axial (b) reconstructions demonstrate osseous remodeling of the “fang”-like elongation with blunting of the growth (black circle and black arrow). A postoperative digital subtraction angiography (c and d) 9 months after surgery demonstrates resolution of the compression in neutral and with head rotation.
DISCUSSION
Since Sorenson initially described the patient who presented with VA dissection after head rotation during archery practice, several additional causative etiologies of BHS have been described.[
In addition to a condition such a cervical spondylosis or rheumatoid arthritis, patients often have a vascular variant that predisposes them to have symptoms with positional occlusion of a single VA.[
Both surgical options of an ACDF or a posterior cervical lateral mass resection of C5 and lateral mass fixation and fusion were presented to our patient. With his lack of symptoms in the neutral position, advanced age, and premorbid cardiac risk factors, we felt that an ACDF would be as efficacious as a direct decompression of the VA, pose less perioperative risk, and produce an easier postoperative recovery.
In addition to the novel contributing etiology, this case is unique in that it angiographically demonstrates osseous remodeling. While we were expecting the ACDF to prevent dynamic occlusion of the VA, we did not anticipate such a dramatic osseous change that returned the lumen of the VA to its natural caliber. We suspect that arterial pulsations were responsible for remodeling the adjacent osseous growth. Arterial pulsations have been postulated to “direct” the formation of DISH osteophytes,[
CONCLUSION
This case reaffirms the distinctive nature of BHS, which motion is required for symptomatology, and treatment strategies should be tailored to the patient and specific etiology. That is, a compressive structure of the VA may be safely treated with segmental fusion, rather than direct decompression, if the patient is asymptomatic in the neutral position.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ajiboye RM, Zoller SD, Ashana AA, Sharma A, Sheppard W, Holly LT. Regression of disc-osteophyte complexes following laminoplasty versus laminectomy with fusion for cervical spondylotic myelopathy. Int J Spine Surg. 2017. 11: 17
2. Bakker JT, Kuperus JS, Kuijf HJ, Oner FC, de Jong PA, Verlaan JJ. Morphological characteristics of diffuse idiopathic skeletal hyperostosis in the cervical spine. PLoS One. 2017. 12: e0188414
3. Buch VP, Madsen PJ, Vaughan KA, Koch PF, Kung DK, Ozturk AK. Rotational vertebrobasilar insufficiency due to compression of a persistent first intersegmental vertebral artery variant: Case report. J Neurosurg Spine. 2017. 26: 199-202
4. Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950. 9: 321-30
5. Ikeda DS, Villelli N, Shaw A, Powers C. Bow hunter’s syndrome unmasked after contralateral vertebral artery sacrifice for aneurysmal subarachnoid hemorrhage. J Clin Neurosci. 2014. 21: 1044-6
6. Jost GF, Dailey AT. Bow hunter’s syndrome revisited: 2 New cases and literature review of 124 cases. Neurosurg Focus. 2015. 38: E7
7. Mazières B. Diffuse idiopathic skeletal hyperostosis (Forestierrotes-Querol disease): What’s new?. Joint Bone Spine. 2013. 80: 466-70
8. Schuette AJ, Barrow DL. Rotational vertebral artery syndrome. World Neurosurg. 2012. 79: 680-1
9. Schunemann V, Kim J, Dornbos D, Nimjee SM. C2-C3 anterior cervical arthrodesis in the treatment of bow hunter’s syndrome: Case report and review of the literature. World Neurosurg. 2018. 118: 284-9
10. Sorensen BF. Bow hunter’s stroke. Neurosurgery. 1978. 2: 259-61
11. Vates GE, Wang KC, Bonovich D, Dowd CF, Lawton MT. Bow hunter stroke caused by cervical disc herniation. Case report. J Neurosurg. 2002. 96: 90-3
12. Verlaan JJ, Boswijk PF, de Ru JA, Dhert WJ, Oner FC. Diffuse idiopathic skeletal hyperostosis of the cervical spine: An underestimated cause of dysphagia and airway obstruction. Spine J. 2011. 11: 1058-67