- Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, United States.
DOI:10.25259/SNI_421_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Epstein NE. Ghost Surgery, Including Neurosurgery and Other Surgical Subspecialties. Surg Neurol Int 09-Aug-2019;10:157
How to cite this URL: Epstein NE. Ghost Surgery, Including Neurosurgery and Other Surgical Subspecialties. Surg Neurol Int 09-Aug-2019;10:157. Available from: http://surgicalneurologyint.com/surgicalint-articles/9573/
INTRODUCTION
“Ghost Surgery” is best defined by when a surgeon substitutes their partners and/or other surgeons (e.g., residents, physicians’ assistants or any other healthcare or other individual) to perform the actual operation. Here we reviewed several medicolegal neurosurgical and other surgical subspecialty cases that illustrated how “Ghost Surgery” is being performed.
Definition of “Ghost Surgery”
“Ghost Surgery” occurs when the original surgeon substitutes someone else to perform the actual operation. Dunn (2015) defined ghost surgery as: “…when a physician assistant, a surgical assistant, an RN first assistant, a resident, or another surgeon assists on or performs an operative or other invasive procedure without the patient’s knowledge, regardless of whether the surgeon who obtained the consent was scrubbed in or not.”[
Gray v. Grunnagle (1966): “Ghost Neurosurgery”[ 3 ]
The patient, Charles B. Gray, saw an orthopedist, and was admitted to the hospital.[
Holmes’ Article on Ghost Surgery in 1980[ 4 ]
Substitute Surgeons Implanting Medical Devices
In 1980, Holmes discussed “Ghost Surgery”, and estimated that 50-85% of the operations performed in teaching hospitals by 1980 were done by residents, often without an attending present.[
Industry Representative Implanting A Medical Device[ 4 ]
Holmes also defined “Ghost Surgery” as occurring when a representative from industry performed the actual implantation of a medical device. [
Perna v Pirozzi (1982): “Ghost Urological Surgery”[ 8 ]
The plaintiff Thomas Perna saw Dr. Michael Pirozzi, a urological surgeon, and was told he needed surgery for kidney stones (right pyelolithotomy); Dr. Pirozzi obtained the patient’s informed consent.[
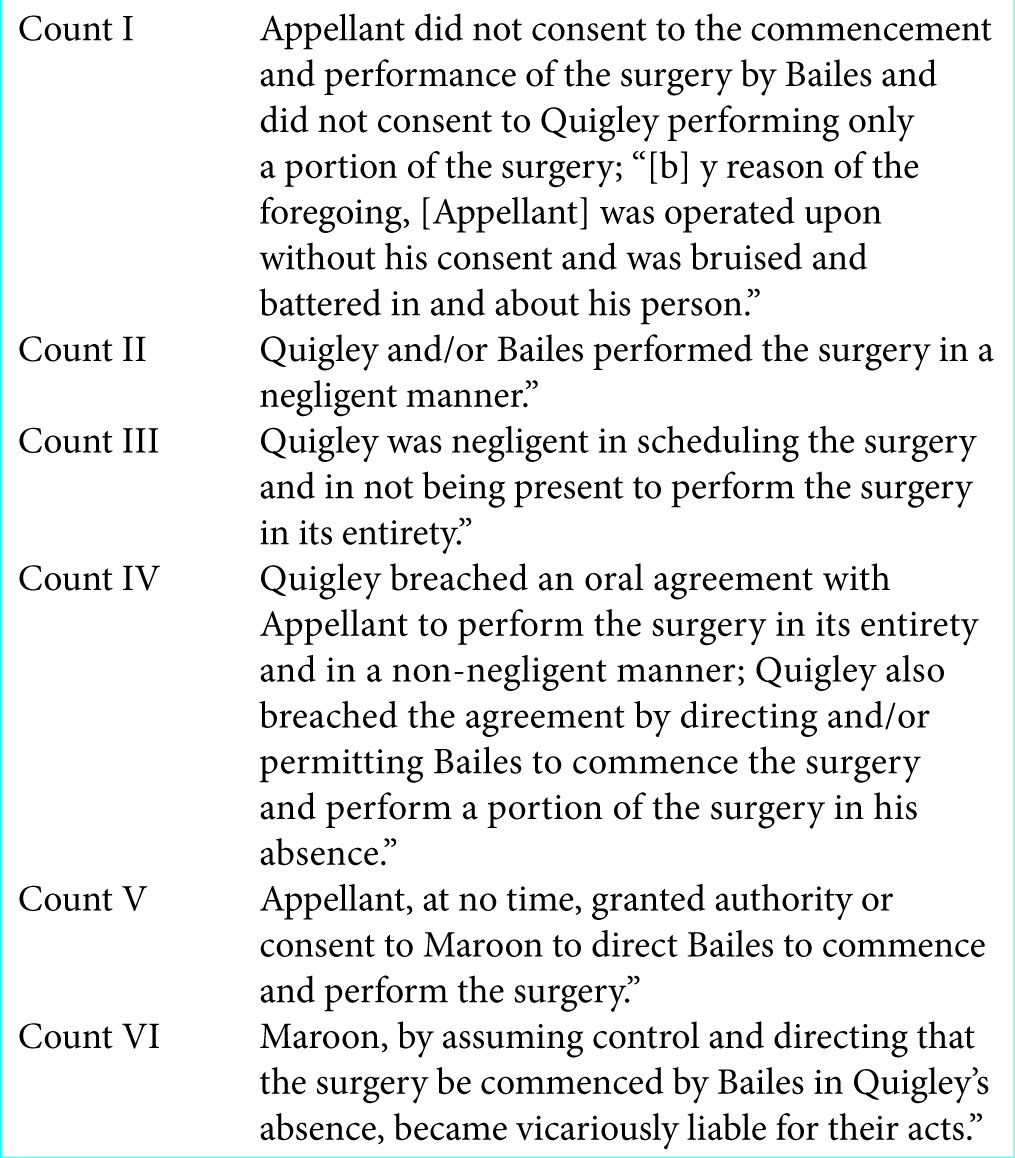
Grabowski v Quigley (1996): “Ghost Neurosurgery”[ 2 ]
In Grabowski vs. Quigley et al. (1996), Grabowski scheduled spinal neurosurgery with Dr. Quigley on April 18, 1989.[
Mr. Grabowski later filed a suit after finding out that Dr. Quigley was not in the operating room for most of the case; the patient had consented for Dr. Quigley alone to perform the surgery. Here, the New Jersey Supreme Court quoted from the Perna v. Pirozzi case regarding the lack of informed consent.[
Kocher 2002: “Ghost Orthopedic Surgery”[ 6 ]
In 2002, Kocher introduced 3 cases in which ghost surgeons performed the surgery: shoulder arthroscopy, knee arthroscopy, and Carpal Tunnel release.[
In the first case, a patient required additional hospitalization following shoulder arthroscopy; the patient sued when he found out that the surgeon’s partner did the surgery. In the second case, a patient developed a complication following an arthroscopic partial meniscectomy performed by a resident rather by his surgeon. The patient sued when he found out that his surgeon left the room to operate “simultaneously” in another operating room. In the third case, a carpal tunnel release was performed by a resident, who injured the median nerve, under the supervision of the attending orthopedist.
Kweon 2016: “Ghost Plastic Surgery”[ 7 ]
In 2016, Kweon discussed how The Korean Association of Plastic Surgeons (KAPS) reviewed a plastic procedure performed by a “Ghost Surgeon” at an out-patient Plastic Surgical Clinic; the high school student died of cerebral hypoxia.[
Hong et al. 2018: “Ghost General Surgery”[ 5 ]
Hong et al. (2018) observed that “Ghost Surgery” was not new, and added that it; “…happens in university-affiliated hospitals as well as private hospitals”.[
CONClUSION
“Ghost Surgery” is seen in neurosurgery and other surgical subspecialties. It occurs when the surgeon of record, who obtained the informed consent, does not perform the operation; rather it is performed by another individual (partner surgeon, another surgeon, resident, other).[
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management.
References
1. Dunn DA. Ghost Surgery: A Frank Look at the Issue and How to Address It. ORN J. 2015. 102: 603-13
2. .editorsp.
3. .editorsp.
4. Holmes MK, Ghost Surgery. Bull N Y Acad Med. 1980. 56: 412-419
5. Hong SE, Hong MK, Park BY, Woo KJ, Kang SR. Is the “ghost surgery” the subject of legal punishment in Korea?. Ann Surg Treat Res. 2018. 94: 167-173
6. Kocher MS.editors. Ghost surgery: the ethical and legal implications of who does the operation. J Bone Joint Surg Am. 2002. 84: 148-50
7. Kweon YD. Ghost Surgeries Must Be Eradicated. Korean Association of Plastic surgeons Public Information & Public Affairs Committee Chairman, Former Korean Society of Plastic and Reconstructive Surgeons Ethics Committee Chairman Arch Plast Surg. 2016. 43: 309-10
8. .editorsp.






ADRIAN SANTANA
Posted April 6, 2023, 1:57 pm
As Always Prof.Eipstein exellent Item