- Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, United States.
- Department of Radiology, Icahn School of Medicine, New York, United States.
- Department of Pathology, Mount Sinai Health System, New York, United States.
Correspondence Address:
Remi A. Kessler
Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, United States.
DOI:10.25259/SNI_898_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Remi A. Kessler1, Mia Saade1, Emily K. Chapman1, Rui Feng1, Thomas P. Naidich2, Mary E. Fowkes3, Joshua B. Bederson1, Peter F. Morgenstern1. Giant chondrosarcoma of the falx in an adolescent: A case report. 08-Apr-2021;12:137
How to cite this URL: Remi A. Kessler1, Mia Saade1, Emily K. Chapman1, Rui Feng1, Thomas P. Naidich2, Mary E. Fowkes3, Joshua B. Bederson1, Peter F. Morgenstern1. Giant chondrosarcoma of the falx in an adolescent: A case report. 08-Apr-2021;12:137. Available from: https://surgicalneurologyint.com/surgicalint-articles/10706/
Abstract
Background: Intracranial chondrosarcomas are slowly growing malignant cartilaginous tumors that are especially rare in adolescents.
Case Description: A 19-year-old woman with no medical history presented with symptoms of intermittent facial twitching and progressive generalized weakness for 6 months. The patient’s physical examination was unremarkable. Imaging revealed a large bifrontal mass arising from the falx cerebri, with significant compression of both cerebral hemispheres and downward displacement of the corpus callosum. The patient underwent a bifrontal craniotomy for gross total resection of tumor. Neuropathologic examination revealed a bland cartilaginous lesion most consistent with low-grade chondrosarcoma. Her postoperative course was uneventful, and she was discharged to home on postoperative day 3.
Conclusion: This is an unusual case of an extra-axial, non-skull base, low-grade chondrosarcoma presenting as facial spasm in an adolescent patient.
Keywords: Adolescent, Chondrosarcoma, Falx cerebri, Intracranial, Pediatric
INTRODUCTION
Intracranial chondrosarcomas are rare, slowly growing, malignant cartilaginous tumors first described in 1899. They are thought to originate from embryonal cartilage or meningeal fibroblasts,[
CASE DESCRIPTION
History and physical examination
A 19-year-old female with no medical history presented to the emergency department complaining of intermittent facial twitching and progressive generalized weakness for 6 months. She noted that each episode of facial twitching lasted several minutes and would self-resolve. She described her weakness as “heaviness” in all extremities such that occasionally she was unable to lift her arms above her shoulders. She endorsed bilateral frontal headache alleviated by ibuprofen, and “fullness” in both ears, more severe on the right. She denied visual symptoms, dizziness, tingling in the extremities, pain, or difficulty with ambulation. The initial physical examination was unremarkable; the patient was neurologically intact.
Imaging
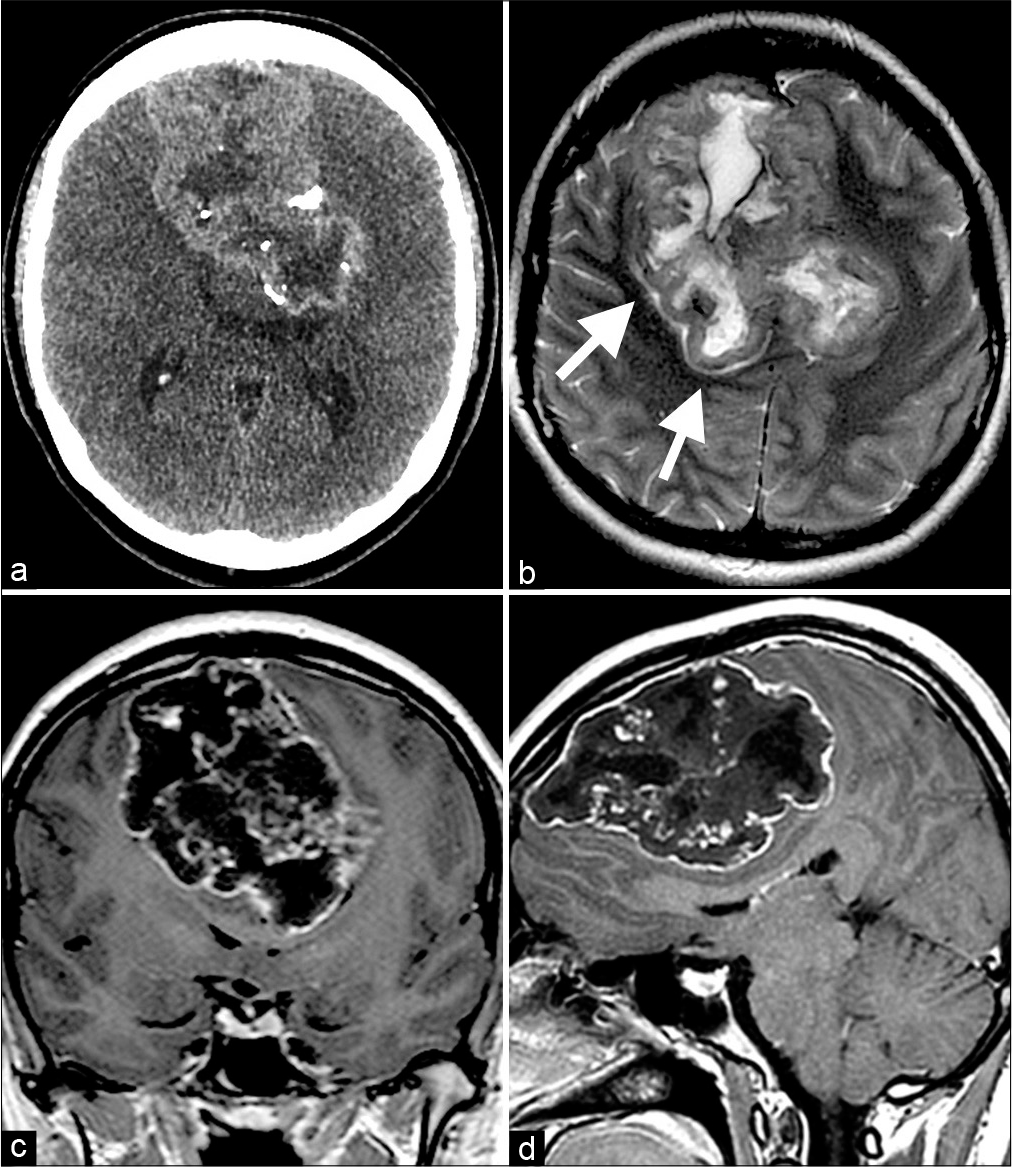
The initial non-contrast computed tomogram of the head showed a large, bifrontal, coarsely calcified extra-axial mass that scalloped the inner table of the skull and displaced the cerebral hemispheres circumferentially [
Figure 1:
(a) Non-contrast axial CT section demonstrates a large, well-defined, partially calcified midline mass that displaces each cerebral hemisphere laterally and displaces lateral ventricles posteriorly. There is no evidence of cerebral edema. (b) Non-contrast axial T2-weighted MRI displays heterogeneous internal texture of the mass. Myelinated cerebral white matter shows normal signal intensity with no evidence of cerebral edema. Clear, cerebral spinal fluid-containing cleavage plane (arrows) between medial surface of the right hemisphere and central mass confirms that the mass is extra-axial. (c and d) Contrast-enhanced T1-weighted MRI in coronal (c) and sagittal (d) planes shows heterogeneous enhancement along the surface and within the interstices of the tumor. There is marked compression of corpus callosum and lateral ventricles and a central vector of mass that displaces the brain downward through tentorial incisura and displaces cerebellar tonsils downward through foramen magnum. The nearly linear contour of the left side of mass and of the medial border of the left cerebral hemisphere again suggests that the mass arises from midline falx.
Surgical treatment
Surgery was recommended to alleviate the mass effect and obtain a tissue diagnosis. Given the size of the tumor and the possible pathologies considered, initial biopsy was not performed, and maximal safe resection was planned. The patient underwent bifrontal craniotomy for resection of tumor. The lesion was extremely firm and not amenable to ultrasonic aspiration or typical cautery and suction techniques. Monopolar loop cautery was utilized to progressively debulk the lesion piecemeal so that the capsule could be defined from the surrounding compressed brain. Calcifications were removed en bloc, as they could not be divided sharply or with cautery. There was no brain invasion, and the tumor was removed completely.
Pathology
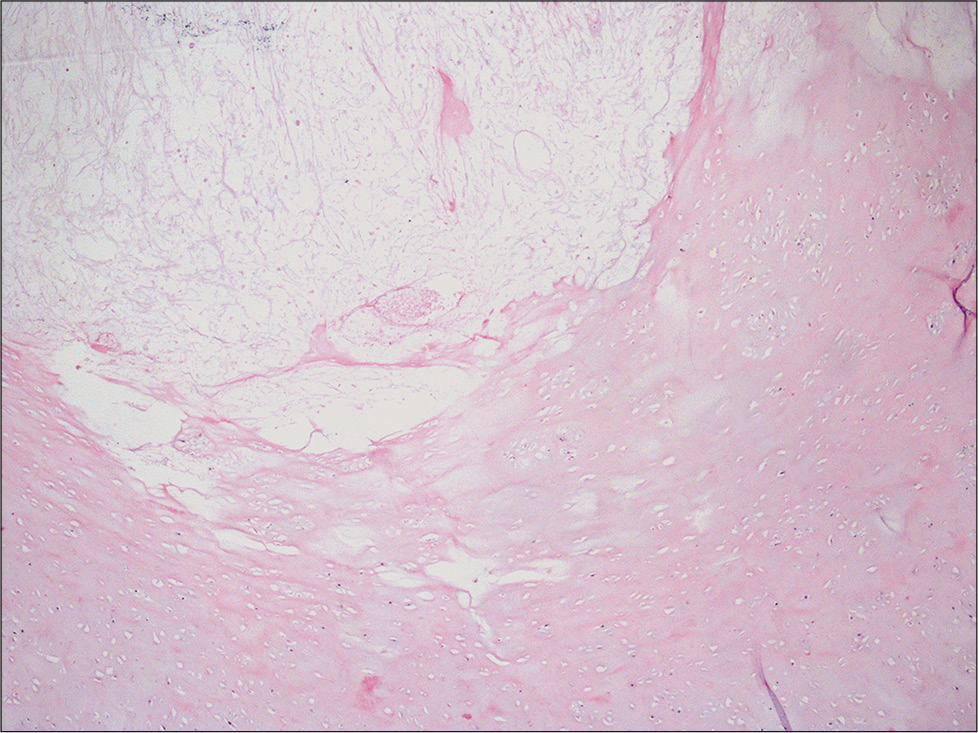
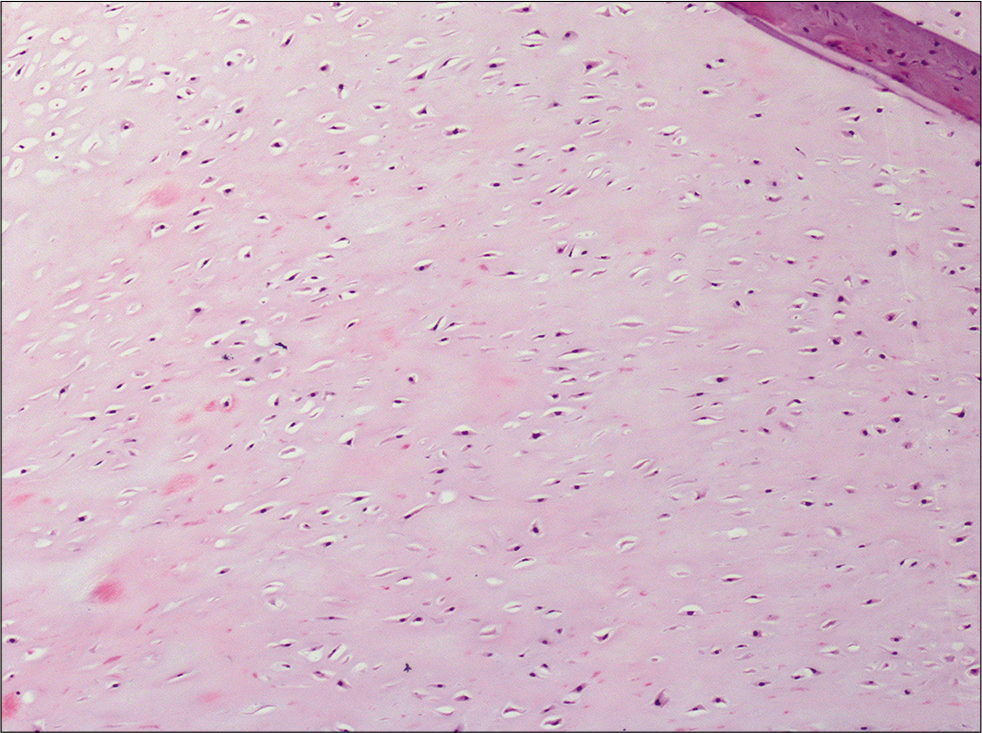
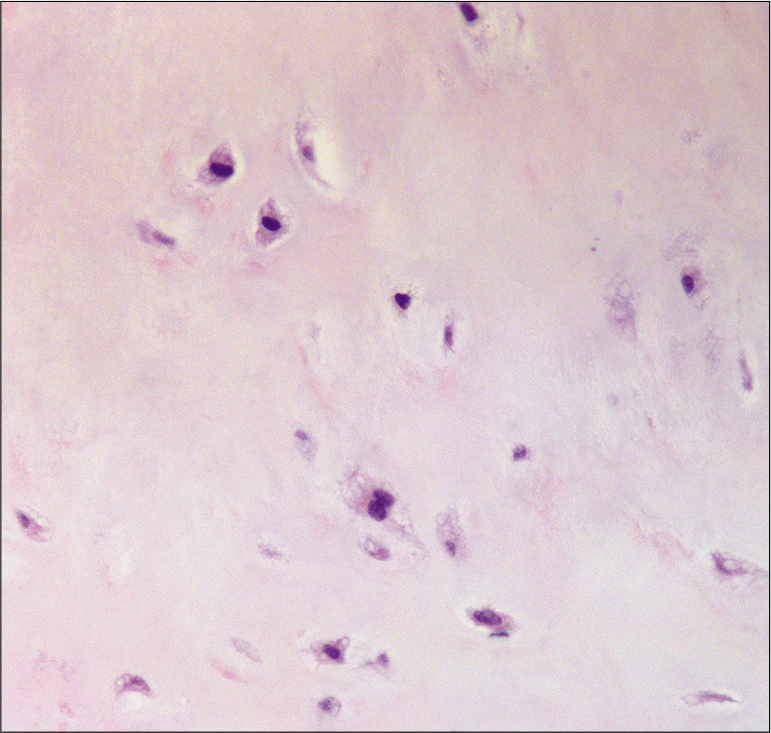
Pathologic examination revealed a low-grade cartilaginous neoplasm. The lesion was composed of an encapsulated bland chondroid tumor with a thin fibrous capsule with minimal nuclear atypia, no perceived increase in nuclei within the lacunar spaces, and no identifiable mitotic figures.
However, because cartilaginous tumors of the falx cerebri are very rare and the distinction between chondroma and low-grade chondrosarcoma is challenging, an outside pathologist was consulted for a second opinion. This pathologist noted that although the diagnosis was difficult in this case, due to the presence of moderate cellularity, chondrocyte crowding, mild nuclear atypia, frequent binucleation, patchy necrosis, and myxoid change, a diagnosis of low-grade chondrosarcoma was most likely [
Postsurgical course
The patient’s postoperative course was uncomplicated. Postoperative MRI confirmed a gross total resection with no significant ischemia or edema. She was discharged home on postoperative day 3 with home physical therapy. On the first day at home, she experienced a 3-minute episode of facial spasm. Her dose of levetiracetam was increased from 2000 mg/day to 3000 mg/day. Since this change, she has done well with no complaints. At the patient’s 2-month postoperative follow-up, her only complaints were mild headaches, difficulty sleeping, and some fatigue. At 4-month follow-up, she was completely asymptomatic, and she is currently in the process of attempting to wean off levetiracetam. On-going surveillance imaging for recurrence is planned.
DISCUSSION
In older children and adolescents with a new meningeal neoplasm, the leading diagnostic consideration is meningioma. Differential diagnoses that are more common in pediatric than adult patients include teratoma, other congenital dysplastic tumors, hemangiopericytoma, and, rarely, massively exophytic oligodendroglioma.[
Comprehensive literature search revealed eleven distinct cases of intracranial chondrosarcoma arising from the falx in patients under 25 years old; six of which cases were pediatric or adolescent patients (<18 years old).[
Intracranial chondrosarcoma is difficult to distinguish from other meningeal neoplasms on the basis of clinical presentation and preoperative imaging. In one case, contrast-enhanced MRI demonstrated a heterogeneous lesion with perifocal edema presumed to be a meningioma or hemangiopericytoma preoperatively.[
Chondrosarcomas show a distinct pathology that is subclassified as mesenchymal or myxoid. The majority of falcine and parasagittal chondrosarcomas are mesenchymal.[
Gross total surgical resection is the ideal treatment of intracranial chondrosarcomas. Postoperative radiotherapy is controversial, as some researchers express concern that radiation may increase the risk for malignant transformation. [
CONCLUSION
The present report describes a pathologically confirmed intracranial, extra-axial low-grade chondrosarcoma projecting from the falx cerebri in an adolescent patient presenting as facial spasm ultimately thought to be due to substantial tumor mass effect. To the best of our knowledge, this is the first reported case of chondrosarcoma in an adolescent with these specific presenting symptoms. Her prognosis is deemed overall favorable given that the pathology was low grade. Close surveillance with serial imaging over the next several years is warranted.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Gerszten PC, Pollack IF, Hamilton RL. Primary parafalcine chondrosarcoma in a child. Acta Neuropathol. 1998. 95: 111-4
2. Güneş M, Günaldi O, Tuğcu B, Tanriverdi O, Güler AK, Cöllüoğlu B. Intracranial chondrosarcoma: A case report and review of the literature. Minim Invasive Neurosurg. 2009. 52: 238-41
3. Lin HS, Tsai CC, Chang CK, Chen SJ. Giant intracranial mesenchymal chondrosarcoma with uncal herniation. Formos J Surg. 2012. 45: 93-6
4. Nagata S, Sawada K, Kitamura K. Chondrosarcoma arising from the falx cerebri. Surg Neurol. 1986. 25: 505-9
5. Omezine S, Bouali S, Taallah M, Zehani A, Kallel J, Jemel H. Distinguishing falcine chondrosarcomas from their mimics and management. World Neurosurg. 2018. 118: 279-83
6. Park JH, Kim MJ, Kim CJ, Kim JH. Intracranial extraskeletal myxoid chondrosarcoma: Case report and literature review. J Korean Neurosurg Soc. 2012. 52: 246-9
7. Perry A, Dehner LP. Meningeal tumors of childhood and infancy. An update and literature review. Brain Pathol. 2003. 13: 386-408
8. Sadashiva N, Sharma A, Shukla D, Rajalakshmi P, Mahadevan A, Devi BI. Intracranial extraskeletal mesenchymal chondrosarcoma. World Neurosurg. 2016. 95: 618.e1-6
9. Safaee M, Clark AJ, Tihan T, Parsa AT, Bloch O. Falcine and parasagittal chondrosarcomas. J Clin Neurosci. 2013. 20: 1232-6