- Clinic of Neurosurgery, St. Ivan Rilski Hospital, Sofia, Bulgaria.
DOI:10.25259/SNI_733_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dilyan Ferdinandov, Dimo Yankov, Assen Bussarsky. Grisel’s syndrome in adults: A case report. 13-Jan-2021;12:15
How to cite this URL: Dilyan Ferdinandov, Dimo Yankov, Assen Bussarsky. Grisel’s syndrome in adults: A case report. 13-Jan-2021;12:15. Available from: https://surgicalneurologyint.com/surgicalint-articles/10524/
Abstract
Background: The non traumatic, post inflammatory atlantoaxial rotatory instability, also known as Grisel’s syndrome is a relatively rare condition usually affecting children. Adult cases are rare and even less frequently reported with separate case reports describing a single patient. Although antibiotic treatment and close neurological monitoring seem to be the gold standard of care, there is no general consensus on the optimal timing and extent of the surgical treatment.
Case Description: We present a case of C1-C2 spondylitis, secondary to retropharyngeal abscess, without atlantoaxial instability on initial evaluation that progressed to C1-C2 subluxation with rapidly developing myelopathy 3 months after optimal antibiotic therapy and complete clinical and biochemical remission.
Conclusion: Grisel’s syndrome is a rare condition in adults with secondary instability in spite of successful antibacterial treatment, which requires decompression and delayed surgical fixation in our case.
Keywords: Atlantoaxial rotatory instability, Atlantoaxial subluxation, Grisel’s syndrome, Surgical treatment
INTRODUCTION
Post inflammatory C1-C2 subluxation was described in the first half of the 19th century by Charles Bell it was later named after Grisel who published a paper on two patients with retropharyngeal inflammatory involvement of the C1 anterior arch, C2 dens, and ligamentous complex.[
CASE DESCRIPTION
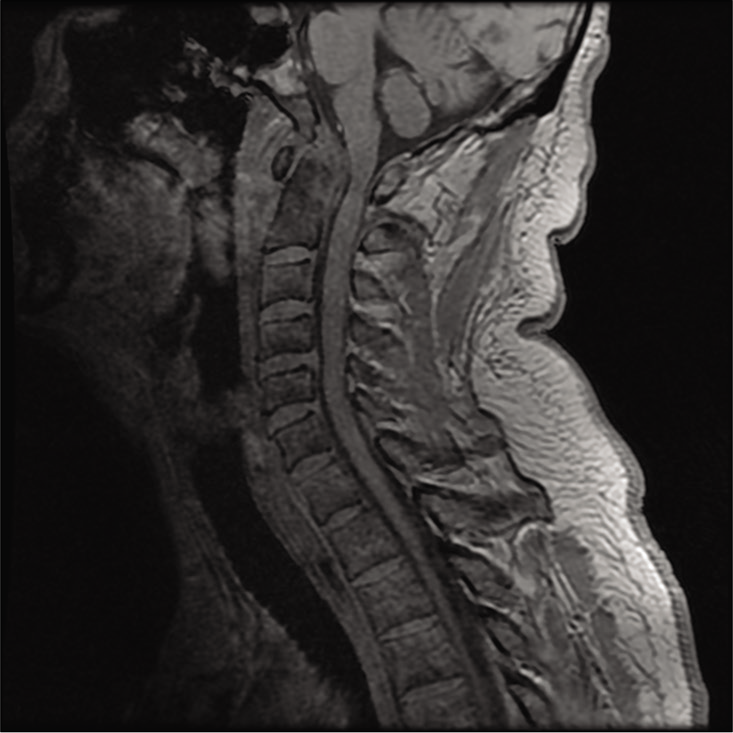
A 48-year-old male was treated at our institution between April and September 2018, no history of intravenous drug use or HIV infection was noted. He was referred to the department of neurosurgery with a 1 month history of the upper cervical region pain radiating toward the shoulders and proximal brachia, tenderness, and increased rigidity of the neck musculature. The patient reported a history of oropharyngeal bacterial infection that was interpreted as strep throat by the general practitioner, for which the patient received a 10-day course of antibiotic. Although local inflammation was resolved the patient continued to feel under the weather, complaining of night sweats general lack of energy and later on – neck pain and tenderness that was previously described. After a cervical magnetic resonance imaging (MRI) was performed [
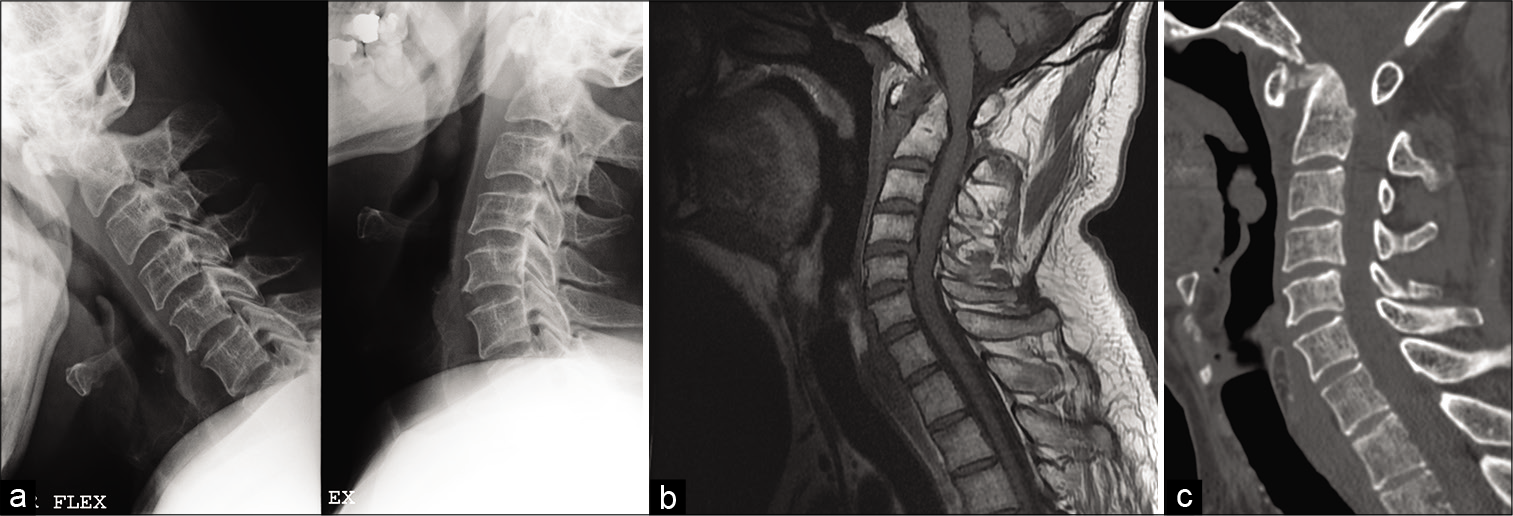
Initial complete blood count (CBC) was significant for leukocytosis – 24.12 × 109/L, ESR was 70 mm/h, and C-RP was 92.10 mg/L. In light of the lab test results and the history of infectious pharyngitis, we postulated that the bacterial infection was incompletely resolved and has now spread to the retropharyngeal space and the C1-C2 complex. Blood cultures were negative and broad-spectrum antibiotic treatment was ineffective. During the diagnostic work-up, standard dynamic X-rays were obtained to ascertain the presence of instability and the need for surgical C1-C2 fixation [
Figure 2:
(a) The atlantoaxial complex is stable on lateral dynamic X-rays with atlantodental interval (ADI) in range (<3 mm). (b) Sagittal T1 magnetic resonance imaging – no retropharyngeal mass persist, but the C2 dens is significantly dorsally displaced causing central cervical canal stenosis. ADI is pathologically increased (14 mm) with evidence of subluxation and C1-C2 stenosis. (c) Sagittal computed tomography (bone) – evidence of alar and transverse ligament involvement with calcification of the osteoligamentous complex.
However, 2 weeks before the appointment the patient became symptomatic for the upper cervical cord compression – increasing pain in the neck, occiput and shoulders, weakness in both arms, gait disturbances, and rigidity and hyperreflexia for both legs. A new emergency MRI was ordered that showed complete resolution of the retropharyngeal abscess and the C2 spondylitis; however, signs of spinal cord compression with myelopathy as well as instability were evident with atlantodental interval (ADI) out of range [
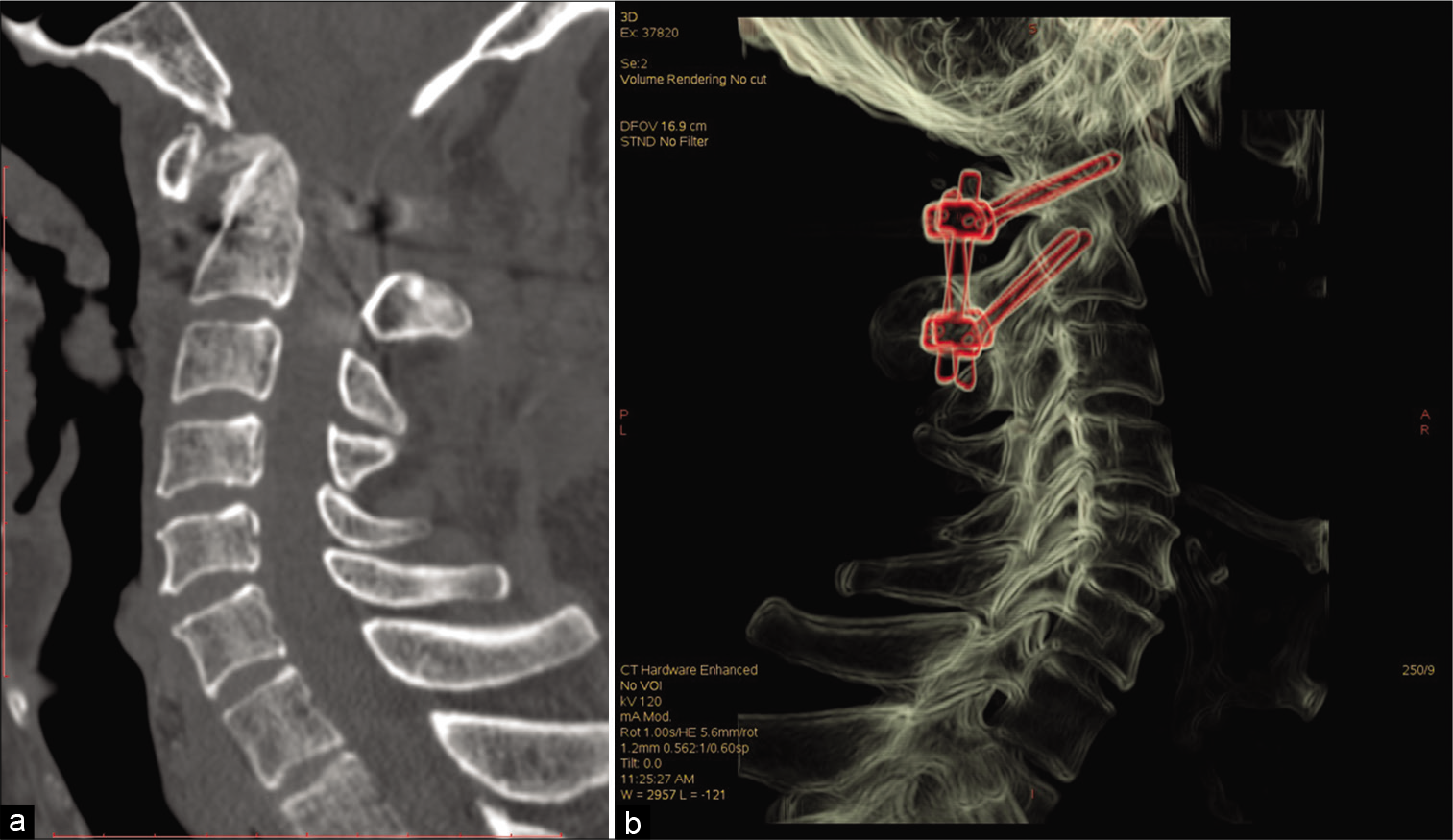
At this point, we decided to perform an emergent C1 posterior decompression with C1 lateral mass and C2 isthmus screws fixation and fusion [
DISCUSSION
Although extremely rare in adults Grisel’s syndrome should always be suspected when there is clinical evidence of paravertebral infectious processes, with secondary C1-C2 involvement. Even without evidence of instability on initial assessment these patients can deteriorate rapidly because of secondary atlantoaxial rotational hypermobility. Initial imaging studies that suggest soft-tissue inflammation, but no atlantoaxial hypermobility or subluxation, are not definitive and these patients need close follow-up. A standard lateral X-ray of the cervical spine could be sufficient to evaluate progressing instability. In our case a patient with no significant C1-C2 subluxation went on to develop Fielding Grade III AARI in <3 months.[
CONCLUSION
Patients presenting with cervical vertebral syndrome with a history of upper respiratory tract infections should be suspected for Grisel’s syndrome, irrespective of their age. Lack of AARI on initial examination should not exclude the diagnosis and it might progress to instability with spinal compression once confirmed. There is not enough clinical evidence to support early, aggressive surgical management, although our experience and other case reports suggest that surgical immobilization of the C1-C2 complex may produce better short-term results and prevent later dynamic instability.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baker LL, Bower CM, Glasier CM. Atlanto-axial subluxation and cervical osteomyelitis: Two unusual complications of adenoidectomy. Ann Otol Rhinol Laryngol. 1996. 105: 295-9
2. Clark WC, Coscia M, Acker JD, Wainscott K, Robertson JT. Infection-related spontaneous atlantoaxial dislocation in an adult. Case report. J Neurosurg. 1988. 69: 455-8
3. Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am. 1977. 59: 37-44
4. Galer C, Holbrook E, Treves J, Leopold D. Grisel’s syndrome: A case report and review of the literature. Int J Pediatr Otorhinolaryngol. 2005. 69: 1689-92
5. Grisel P. Enucleation de l’atlas et torticollis nasopharyngien. Presse Med. 1951. 59: 1647-8
6. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001. 26: 2467-71
7. Ugur HC, Cağlar S, Unlu A, Erdem A, Kanpolat Y. Infection-related atlantoaxial subluxation in two adults: Grisel syndrome or not?. Acta Neurochir (Wien). 2003. 145: 69-72
8. Welinder NR, Hoffmann P, Håkansson S. Pathogenesis of non-traumatic atlanto-axial subluxation (Grisel’s syndrome). Eur Arch Otorhinolaryngol. 1997. 254: 251-4
9. Wetzel FT, La Rocca H. Grisel’s syndrome. Clin Orthop Relat Res. 1989. 240: 141-52
10. Youssef K, Daniel S. Grisel syndrome in adult patients, Report of two cases and review of the literature. Can J Neurol Sci. 2009. 36: 109-13