- Department of Neurosurgery, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
- Department of Diagnostic and Interventional Radiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
- Department of Anesthesia and Critical Care, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
Correspondence Address:
Deepak Kumar Jha, Department of Neurosurgery, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
DOI:10.25259/SNI_941_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vikrant Sharma1, Mayank Garg1, Suryanarayanan Bhaskar1, Sarbesh Tiwari2, Pradeep Kumar Bhatia3, Deepak Kumar Jha1. Handmade models for aneurysm surgery: A useful tool for training. 09-Dec-2022;13:571
How to cite this URL: Vikrant Sharma1, Mayank Garg1, Suryanarayanan Bhaskar1, Sarbesh Tiwari2, Pradeep Kumar Bhatia3, Deepak Kumar Jha1. Handmade models for aneurysm surgery: A useful tool for training. 09-Dec-2022;13:571. Available from: https://surgicalneurologyint.com/surgicalint-articles/12052/
Abstract
Background: Aneurysm surgery is considered difficult by young and trainee neurosurgeons. This is due to difficulty in understanding orientation of aneurysm complex (proximal and distal vessels, aneurysm neck, and fundus) in relation to the surrounding structures (skull, brain, vessels, and nerves) after head is rotated, extended, and fixed on the head frame. Virtual three-dimensional (3D) imaging studies and 3D-printed models help young neurosurgeons but are not accessible to most of the centers due to need for resources (human and equipment). Authors used handmade 3D models of aneurysm complex to train young neurosurgeons before and during surgery to make them understand steps to treat it.
Methods: RadiAnt DICOM viewer software (2022.1.1, 64-bit, Medixant, Poznan, Poland) was used for acquiring 3D Volume Rendering Technique images to make aneurysm models preoperatively. Twisted 20 Gauze galvanized iron wires were used for making proximal and distal branches and Epoxy Putty (M-seal, Pidilite® industries, Mumbai, India) was used to make smooth surfaces of the vessels, aneurysm necks, and fundi. Models were used in operating room (OR) before and during surgery to help surgeons and trainees get oriented to the aneurysm complexes.
Results: Handmade models, oriented as per patients’ head position, were useful to make surgeons and trainees to understand projection of various components of the aneurysm complex in relation to adjacent structures, especially skull base, during both preoperative planning and in OR even before completion of the dissection.
Conclusion: Handmade models of aneurysms are inexpensive tool and can help trainee neurosurgeons to plan and execute surgical management of aneurysms.
Keywords: Aneurysm, Cerebrovascular, Epoxy putty, Handmade models, Volume rendering technique
INTRODUCTION
Aneurysm clipping is considered complex and difficult especially by trainee and young neurosurgeons.[
Authors use handmade 3D models of AC to plan and execute aneurysm surgeries along with training trainees and young neurosurgeons and report the technical details of the same.
TECHNIQUE
As per protocol, patients with intracranial aneurysms planned for craniotomy and clipping underwent computed tomography angiography (Somatom Definition Flash, 256 Slice, Siemens, Germany). DSA too was done whenever required in cases of unsatisfactory visualization of AC, blister aneurysm was suspected, or cross flow assessment was required. Digital CT angiogram DICOM files were acquired and 3D VRT images were processed using RadiAnt DICOM Viewer (2022.1.1, 64-bit, Medixant, Poznan, Poland).
VRT images of the AC were acquired on desktop/laptop as per our earlier report.[
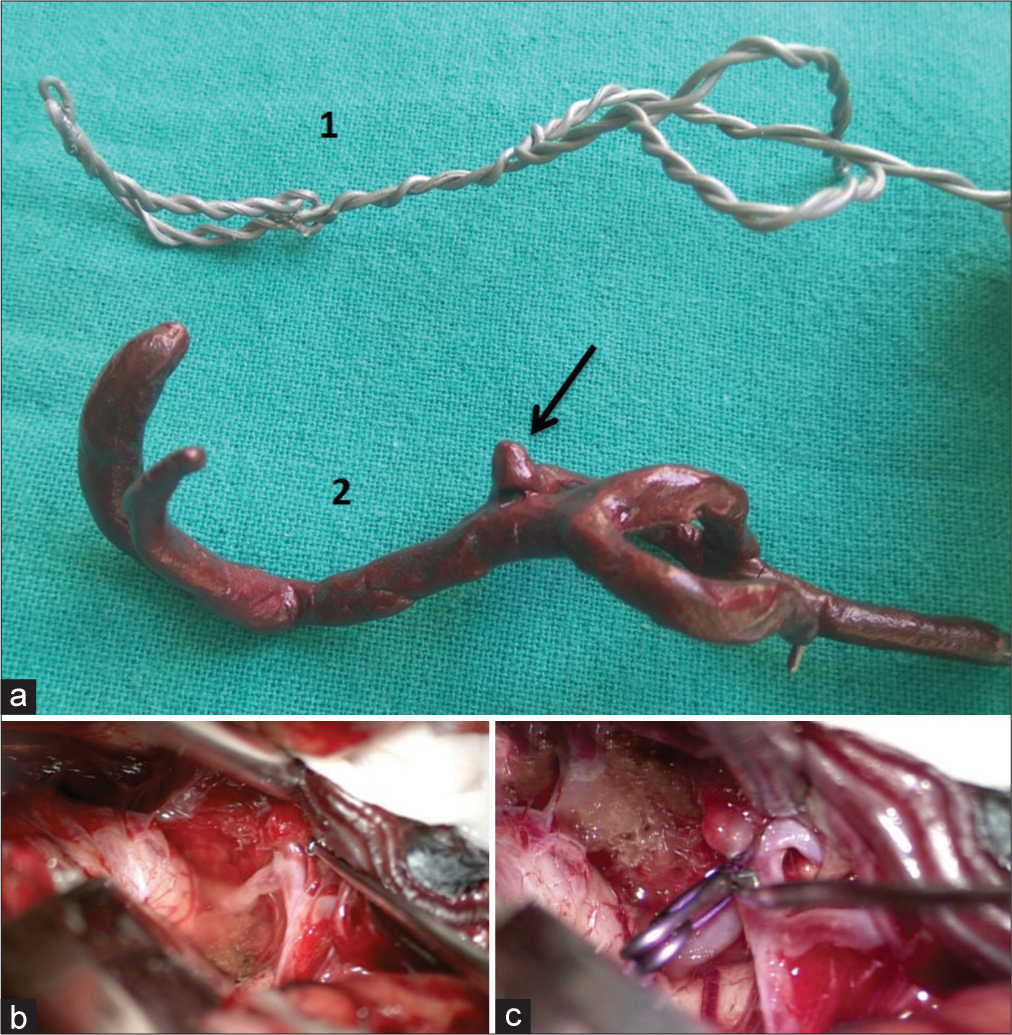
Figure 1:
(a) Shows twisted galvanized iron wire skeleton of right middle cerebral artery bifurcation aneurysm (1) which was covered buy epoxy putty to depict aneurysm (arrow) and (2) the model was colored dark red by fabric color. (b) Surgically exposed right sylvian fissure through pterional approach showing proximal and distal branches of aneurysm complex. (c) Surgical field showing clipped aneurysm and proximal and distal branches of aneurysm complex.
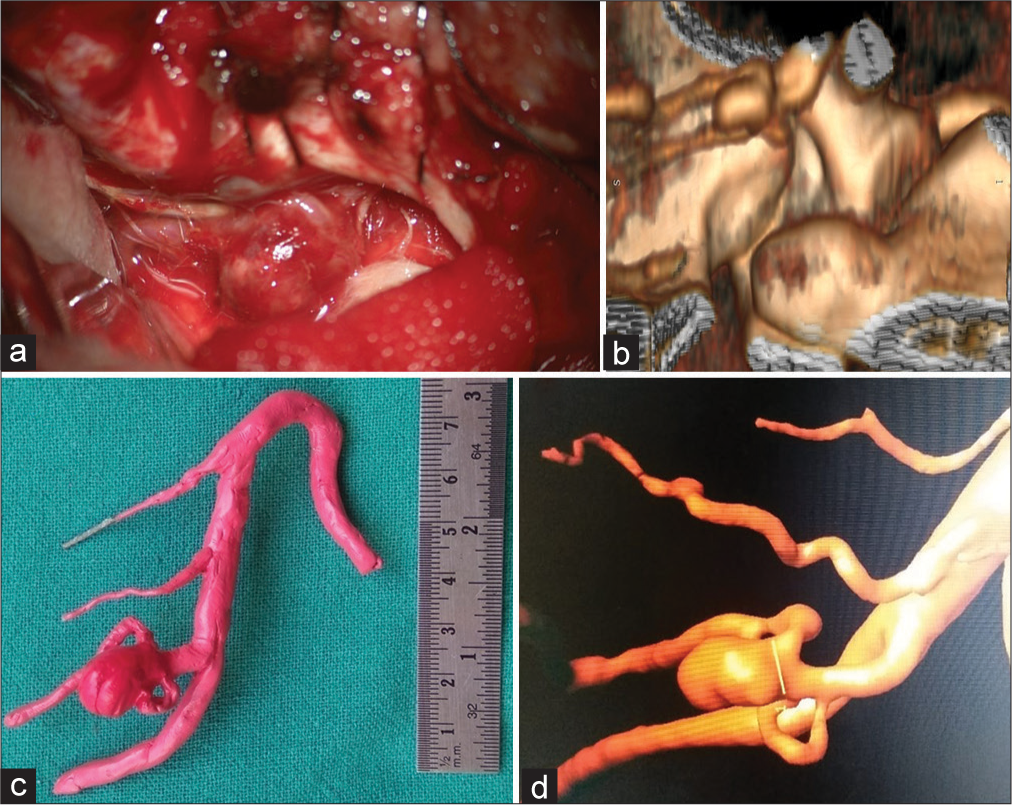
Figure 2:
Surgically exposed left posterior inferior cerebellar artery aneurysm using left para-median suboccipital craniotomy (a). Same aneurysm seen on edited CT volume rendering technique (VRT) image (b), handmade model (c), digital subtraction angiography VRT, and (d) positioned similar to patient’s head.
DISCUSSION
Cerebrovascular anatomy is taught by two dimensional images of line diagrams which are available in textbooks in the early part of medical training. Cadaver dissection and cadaver dissection images are also part of the curriculum when basic anatomy is taught in the medical schools. Detailed neuroanatomy by two-dimensional images of the line diagrams and cadaver dissection images has become part of the neurosurgical training.[
Advancements in imaging techniques such as CT, MRI, and DSA can provide 3D Multi-Planer Reformation (MPR), which can reveal AC in three axes, are very useful for assessing AC.[
Virtual 3D VRT images of CT for aneurysms are editable and are helpful in preoperative planning of craniotomy, knowing appearance of AC in relation to the adjacent bony structures in a particular head position of the patient which can be made available in the OR on a laptop. These images are rotatable and can be seen from various directions.[
The use of 3D printers is increasing, nowadays,[
Limitations
AC model is made based on appearance of VRT images and all the deficiencies of CT VRT are associated with it especially inability to show thin vessels and perforators and blister aneurysms.[
CONCLUSION
Handmade models of aneurysm complex may be an important tool for preoperative planning and intraoperative assistance in aneurysm surgeries, especially for trainees and young neurosurgeons. It is safe and inexpensive and can be used even at resource limited settings.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ajiboye N, Chalouhi N, Starke RM, Zanaty M, Bell R. Unruptured cerebral aneurysms: Evaluation and management. ScientificWorldJournal. 2015. 2015: 954954
2. Ansari A, Kalyan S, Sae-Ngow T, Yamada Y, Tanaka R, Kawase T. Review of avoidance of complications in cerebral aneurysm surgery: The Fujita experience. Asian J Neurosurg. 2019. 14: 686-92
3. Calhoun PS, Kuszyk BS, Heath DG, Carley JC, Fishman EK. Three-dimensional volume rendering of spiral CT data: Theory and method. Radiographics. 1999. 19: 745-64
4. Cutroneo G, Bruschetta D, Trimarchi F, Cacciola A, Cinquegrani M, Duca A. In vivo CT direct volume rendering: A three-dimensional anatomical description of the heart. Pol J Radiol. 2016. 81: 21-8
5. D’Urso PS, Thompson RG, Atkinson RL, Weidmann MJ, Redmond MJ, Hall BI. Cerebrovascular biomodelling: A technical note. Surg Neurol. 1999. 52: 490-500
6. D2P: Dicom to Print: 3D Medical Image Processing Software. Available from: https://www.oqton.com/d2p [Last accessed on 2022 Oct 12].
7. Erbano BO, Opolski AC, Olandoski M, Foggiatto JA, Kubrusly LF, Dietz UA. Rapid prototyping of three-dimensional biomodels as an adjuvant in the surgical planning for intracranial aneurysms. Acta Cir Bras. 2013. 28: 756-61
8. Fong YW, Hsu SK, Huang CT, Hsieh CT, Chen MH, Huang JS. Impact of intraoperative 3-dimensional volume-rendering rotational angiography on clip repositioning rates in aneurysmal surgery. World Neurosurg. 2018. 114: e573-80
9. Hacein-Bey L, Provenzale JM. Current imaging assessment and treatment of intracranial aneurysms. AJR Am J Roentgenol. 2011. 196: 32-44
10. Hoz SS, Aktham AA, Al-Sharshahi ZF, Esene IN, Mahoney D, Chaurasia B. The most recommended neuroanatomy resources for neurosurgeons: an international survey. Surg Neurol Int. 2021. 12: 11
11. Ishida F, Kawaguchi K, Mizuno M, Hoshino T, Murao K, Taki W. The accuracy and usefulness of 3D-DSA and 3D-CT angiography for cerebral aneurysms. Interv Neuroradiol. 2001. 7: 181-6
12. Jha DK, Khera P, Bhaskar S, Garg M. Three-dimensional volume rendering: An underutilized tool in neurosurgery. World Neurosurg. 2019. 130: 485-92
13. Kimura T, Morita A, Nishimura K, Aiyama H, Itoh H, Fukaya S. Simulation of and training for cerebral aneurysm clipping with 3-dimensional models. Neurosurgery. 2009. 65: 719-26
14. Le Moal J, Peillon C, Dacher JN, Baste JM. Three-dimensional computed tomography reconstruction for operative planning in robotic segmentectomy: A pilot study. J Thorac Dis. 2018. 10: 196-201
15. Lubicz B, Levivier M, François O, Thoma P, Sadeghi N, Collignon L. Sixty-four-row multisection CT angiography for detection and evaluation of ruptured intracranial aneurysms: Interobserver and intertechnique reproducibility. AJNR Am J Neuroradiol. 2007. 28: 1949-55
16. Maruyama K, Watanabe E, Kin T, Saito K, Kumakiri A, Noguchi A. Smart glasses for neurosurgical navigation by augmented reality. Oper Neurosurg (Hagerstown). 2018. 15: 551-6
17. Mashiko T, Kaneko N, Konno T, Otani K, Nagayama R, Watanabe E. Training in cerebral aneurysm clipping using self-made 3-dimensional models. J Surg Educ. 2017. 74: 681-9
18. Moriente NV, Torné MM, Font JC, Sánchez SG, Avellí XF. Anatomical variations of the middle cerebral artery: Duplication and accessory artery. Implications in the treatment of acute stroke. Rev Neurol. 2004. 38: 732-5
19. Müller A, Krishnan KG, Uhl E, Mast G. The application of rapid prototyping techniques in cranial reconstruction and preoperative planning in neurosurgery. J Craniofac Surg. 2003. 14: 899-914
20. Pretorius ES, Fishman EK. Volume-rendered three-dimensional spiral CT: Musculoskeletal applications. Radiographics. 1999. 19: 1143-60
21. Shi WY, Li YD, Li MH, Gu BX, Chen SW, Wang W. 3D rotational angiography with volume rendering: the utility in the detection of intracranial aneurysms. Neurol India. 2010. 58: 908-13
22. Tagaytayan R, Kelemen A, Sik-Lanyi C. Augmented reality in neurosurgery. Arch Med Sci. 2018. 14: 572-8
23. Tahir RA, Haider S, Kole M, Griffith B, Marin H. Anterior cerebral artery: Variant anatomy and pathology. J Vasc Interv Neurol. 2019. 10: 16-22
24. White PM, Teasdale EM, Wardlaw JM, Easton V. Intracranial aneurysms: CT angiography and MR angiography for detection prospective blinded comparison in a large patient cohort. Radiology. 2001. 219: 739-49
25. Wurm G, Tomancok B, Pogady P, Holl K, Trenkler J. Cerebrovascular stereolithographic biomodeling for aneurysm surgery. Technical note. J Neurosurg. 2004. 100: 139-45
26. Yasui T, Kishi H, Komiyama M, Iwai Y, Yamanaka K, Nishikawa M. The limitations of three-dimensional CT angiography (3D-CTA) in the diagnosis of cerebral aneurysms. No Shinkei Geka. 2000. 28: 975-81