- Department of Neurosurgery, AIIMS Raipur, Chhattisgarh,
- Department of Pediatric Endocrinology, Bai Jerbai Wadia Hospital for Children, Mumbai, Maharashtra, India.
Correspondence Address:
Charandeep Singh Gandhoke
Department of Pediatric Endocrinology, Bai Jerbai Wadia Hospital for Children, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_140_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Charandeep Singh Gandhoke, Anil Kumar Sharma, Raghavendra Kumar Sharma, Simran Kaur Syal. Hemifacial spasm due to multiple neurovascular conflicts: A conundrum. 11-Jul-2020;11:180
How to cite this URL: Charandeep Singh Gandhoke, Anil Kumar Sharma, Raghavendra Kumar Sharma, Simran Kaur Syal. Hemifacial spasm due to multiple neurovascular conflicts: A conundrum. 11-Jul-2020;11:180. Available from: https://surgicalneurologyint.com/surgicalint-articles/10122/
Keywords: Anterior inferior cerebellar artery, Basilar artery, Dolichoectasia, Hemifacial spasm, Neurovascular conflict
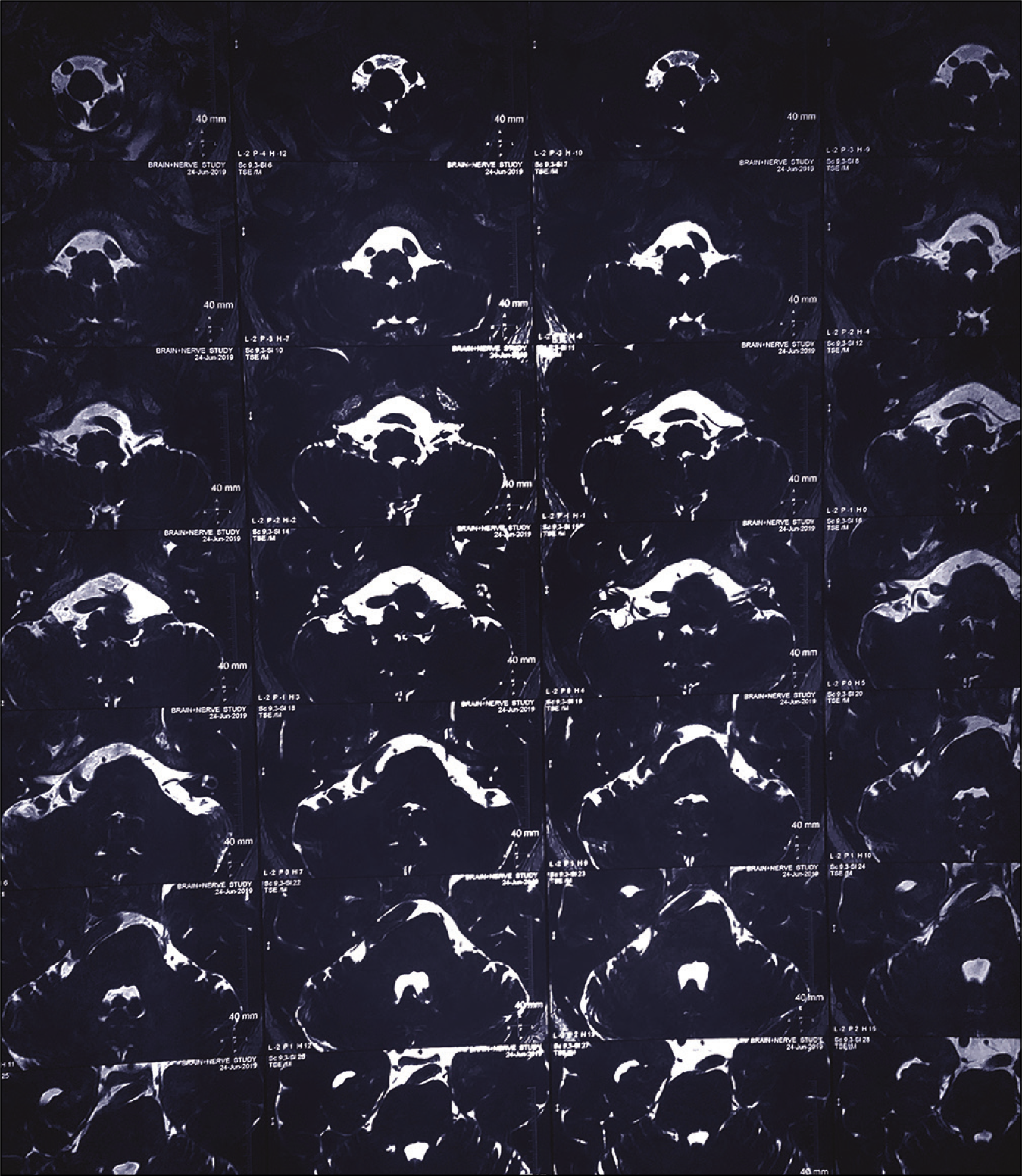
We report the case of a 54-year-old male who presented with complaints of twitching of the right side of the face for 18 months, which had increased in severity for the past 3 months. On examination, there was no neurological deficit. His radiology revealed dolichoectasia of the right vertebrobasilar artery causing compression of the right 7th–8th nerve complex [
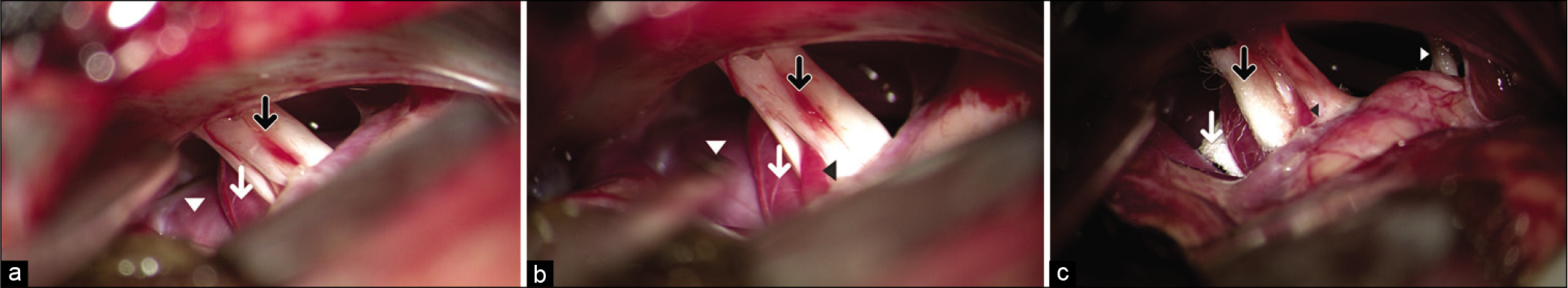
Figure 2:
Intraoperative photographs showing (a) neurovascular conflict between the dolichoectatic basilar artery (white arrowhead), anterior inferior cerebellar artery (AICA) (white arrow), and the 7th–8th nerve complex (black arrow). (b) A branch of AICA splitting and traversing through the 7th–8th nerve complex (black arrowhead) (dolichoectatic basilar artery – white arrowhead, AICA – white arrow, and 7th–8th nerve complex – black arrow). (c) A Teflon patch kept between the dolichoectatic basilar artery on one side and AICA with the 7th–8th nerve complex at the root exit zone on the other side (white arrow). Another Teflon patch was kept between AICA and the 7th–8th nerve complex (black arrow). The branch of AICA traversing through the 7th–8th nerve complex was preserved (black arrowhead). The lower cranial nerves are also seen (white arrowhead).
Hemifacial spasm is usually caused by compression of the facial nerve at the REZ by a vessel, most commonly AICA.[
Declaration of patient consent
Patient’s consent not obtained as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Huang CI, Chen IH, Lee LS. Microvascular decompression for hemifacial spasm: Analyses of operative findings and results in 310 patients. Neurosurgery. 1992. 30: 53-7
2. Loeser JD, Chen J. Hemifacial spasm: Treatment by microsurgical facial nerve decompression. Neurosurgery. 1983. 13: 141-6
3. Payner TD, Tew JM. Recurrence of hemifacial spasm after microvascular decompression. Neurosurgery. 1996. 38: 686-91
4. Yeh HS, Tew JM, Ramirez RM. Microsurgical treatment of intractable hemifacial spasm. Neurosurgery. 1981. 9: 383-6